当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
One-year Outcomes of Prasugrel Versus Ticagrelor In Acute Myocardial Infarction Treated With Primary Angioplasty: The PRAGUE-18 Study
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jacc.2017.11.008 Zuzana Motovska 1 , Ota Hlinomaz 2 , Petr Kala 3 , Milan Hromadka 4 , Jiri Knot 1 , Ivo Varvarovsky 5 , Jaroslav Dusek 6 , Jiri Jarkovsky 7 , Roman Miklik 3 , Richard Rokyta 4 , Frantisek Tousek 8 , Petra Kramarikova 2 , Michal Svoboda 7 , Bohumil Majtan 9 , Stanislav Simek 10 , Marian Branny 11 , Jan Mrozek 12 , Pavel Cervinka 13 , Jiri Ostransky 14 , Petr Widimsky 1 ,
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2018-01-01 , DOI: 10.1016/j.jacc.2017.11.008 Zuzana Motovska 1 , Ota Hlinomaz 2 , Petr Kala 3 , Milan Hromadka 4 , Jiri Knot 1 , Ivo Varvarovsky 5 , Jaroslav Dusek 6 , Jiri Jarkovsky 7 , Roman Miklik 3 , Richard Rokyta 4 , Frantisek Tousek 8 , Petra Kramarikova 2 , Michal Svoboda 7 , Bohumil Majtan 9 , Stanislav Simek 10 , Marian Branny 11 , Jan Mrozek 12 , Pavel Cervinka 13 , Jiri Ostransky 14 , Petr Widimsky 1 ,
Affiliation
|
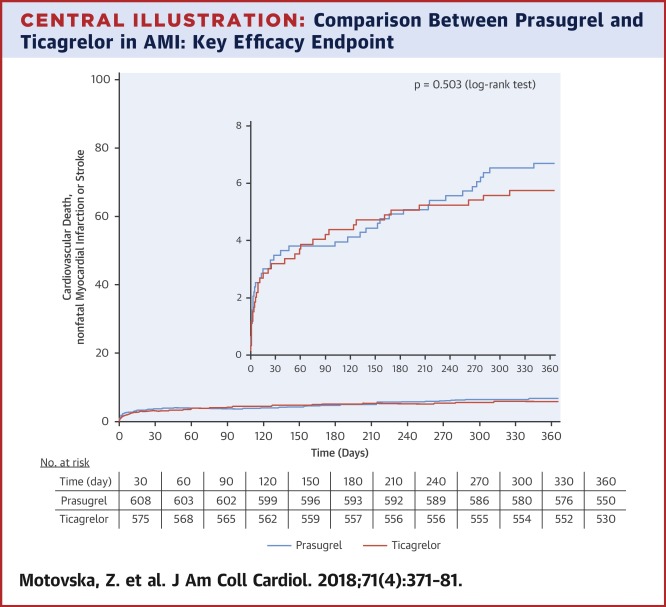
Abstract Background Early outcomes of patients in the PRAGUE-18 study did not find any significant differences between two potent P2Y12 inhibitors. Objective The one-year follow-up of the PRAGUE-18 study focused on (1) a comparison of efficacy and safety between prasugrel and ticagrelor, and (2) on the risk of major ischemic events related to an economically motivated post-discharge switch to clopidogrel. Methods A total of 1,230 patients with acute myocardial infarction (MI) treated with primary PCI were randomized to prasugrel or ticagrelor with an intended treatment duration of 12 months. The combined endpoint was cardiovascular death, MI, or stroke at one year. Since patients had to cover the costs of study medication after hospital discharge, some patients decided to switch to clopidogrel. Results The endpoint occurred in 6.6% of prasugrel patients and in 5.7% of ticagrelor patients; HR, 1.167; 95% CI, 0.742–1.835; P=0.503. No significant differences were found in: cardiovascular death (3.3% vs. 3.0%, P=0.769), MI (3.0% vs. 2.5%, P=0.611), stroke (1.1% vs. 0.7%, P=0.423), all-cause death (4.7% vs. 4.2%, P=0.654), definite stent thrombosis (1.1% vs. 1.5%, P=0.535), all bleeding (10.9% vs. 11.1%, P=0.999), and TIMI major bleeding (0.9% vs. 0.7%, P=0.754). The percentage of patients who switched to clopidogrel for economic reasons was 34.1% (N=216) for prasugrel and 44.4% (N=265) for ticagrelor, P=0.003. Patients who were economically motivated to switched to clopidogrel had (compared to patients who continued the study medications) a lower risk of major cardiovascular events, however they also had lower ischemic risk. Conclusion Prasugrel and ticagrelor are similarly effective during the first year after MI. Economically motivated early post-discharge switches to clopidogrel were not associated with an increased risk of ischemic events. Clinicaltrials.gov NCT02808767
中文翻译:

普拉格雷与替格瑞洛在原发性血管成形术治疗急性心肌梗死中的一年结果:PRAGUE-18 研究
摘要 背景 PRAGUE-18 研究中患者的早期结果未发现两种有效 P2Y12 抑制剂之间存在任何显着差异。目的 PRAGUE-18 研究的一年随访侧重于 (1) 普拉格雷和替格瑞洛之间的疗效和安全性比较,以及 (2) 与出于经济动机的出院后换药相关的主要缺血事件风险氯吡格雷。方法 共有 1,230 名接受直接 PCI 治疗的急性心肌梗死 (MI) 患者随机接受普拉格雷或替格瑞洛治疗,预期治疗持续时间为 12 个月。合并终点是一年时的心血管死亡、MI 或中风。由于患者出院后必须支付研究药物的费用,因此一些患者决定改用氯吡格雷。结果终点发生在6。6% 的普拉格雷患者和 5.7% 的替格瑞洛患者;人力资源,1.167;95% CI,0.742–1.835;P=0.503。在以下方面没有发现显着差异:心血管死亡(3.3% vs. 3.0%,P=0.769)、MI(3.0% vs. 2.5%,P=0.611)、中风(1.1% vs. 0.7%,P=0.423)、全因死亡(4.7% 对 4.2%,P=0.654)、明确支架内血栓形成(1.1% 对 1.5%,P=0.535)、所有出血(10.9% 对 11.1%,P=0.999)和 TIMI大出血(0.9% 对 0.7%,P=0.754)。出于经济原因改用氯吡格雷的患者比例,普拉格雷和替格瑞洛分别为 34.1% (N=216) 和 44.4% (N=265),P=0.003。出于经济动机改用氯吡格雷的患者(与继续服用研究药物的患者相比)发生主要心血管事件的风险较低,但他们的缺血风险也较低。结论 普拉格雷和替格瑞洛在 MI 后第一年的效果相似。出于经济原因,出院后早期改用氯吡格雷与缺血事件风险增加无关。Clinicaltrials.gov NCT02808767
更新日期:2018-01-01
中文翻译:

普拉格雷与替格瑞洛在原发性血管成形术治疗急性心肌梗死中的一年结果:PRAGUE-18 研究
摘要 背景 PRAGUE-18 研究中患者的早期结果未发现两种有效 P2Y12 抑制剂之间存在任何显着差异。目的 PRAGUE-18 研究的一年随访侧重于 (1) 普拉格雷和替格瑞洛之间的疗效和安全性比较,以及 (2) 与出于经济动机的出院后换药相关的主要缺血事件风险氯吡格雷。方法 共有 1,230 名接受直接 PCI 治疗的急性心肌梗死 (MI) 患者随机接受普拉格雷或替格瑞洛治疗,预期治疗持续时间为 12 个月。合并终点是一年时的心血管死亡、MI 或中风。由于患者出院后必须支付研究药物的费用,因此一些患者决定改用氯吡格雷。结果终点发生在6。6% 的普拉格雷患者和 5.7% 的替格瑞洛患者;人力资源,1.167;95% CI,0.742–1.835;P=0.503。在以下方面没有发现显着差异:心血管死亡(3.3% vs. 3.0%,P=0.769)、MI(3.0% vs. 2.5%,P=0.611)、中风(1.1% vs. 0.7%,P=0.423)、全因死亡(4.7% 对 4.2%,P=0.654)、明确支架内血栓形成(1.1% 对 1.5%,P=0.535)、所有出血(10.9% 对 11.1%,P=0.999)和 TIMI大出血(0.9% 对 0.7%,P=0.754)。出于经济原因改用氯吡格雷的患者比例,普拉格雷和替格瑞洛分别为 34.1% (N=216) 和 44.4% (N=265),P=0.003。出于经济动机改用氯吡格雷的患者(与继续服用研究药物的患者相比)发生主要心血管事件的风险较低,但他们的缺血风险也较低。结论 普拉格雷和替格瑞洛在 MI 后第一年的效果相似。出于经济原因,出院后早期改用氯吡格雷与缺血事件风险增加无关。Clinicaltrials.gov NCT02808767











































 京公网安备 11010802027423号
京公网安备 11010802027423号