PLOS Medicine ( IF 10.5 ) Pub Date : 2017-10-24 , DOI: 10.1371/journal.pmed.1002414 Jiangrong Wang , Bengt Andrae , Karin Sundström , Alexander Ploner , Peter Ström , K. Miriam Elfström , Joakim Dillner , Pär Sparén
|
Background
The relatively high incidence of cervical cancer in women at older ages is a continuing concern in countries with long-established cervical screening. Controversy remains on when and how to cease screening. Existing population-based studies on the effectiveness of cervical screening at older ages have not considered women’s screening history. We performed a nationwide cohort study to investigate the incidence of cervical cancer after age 60 years and its association with cervical screening at age 61–65, stratified by screening history at age 51–60.
Methods and findings
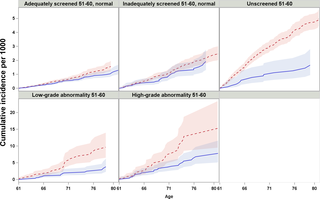
Using the Total Population Register, we identified 569,132 women born between 1 January 1919 and 31 December 1945, resident in Sweden since age 51. Women’s cytological screening records, cervical cancer occurrence, and FIGO stage (for those diagnosed with cancer) were retrieved from national registers and medical charts. We calculated the cumulative incidence of cervical cancer from age 61 to age 80 using a survival function considering competing risk, and estimated the hazard ratio (HR) of cervical cancer in relation to screening status at age 61–65 from Cox models, adjusted for birth cohort and level of education, conditioning on women’s screening history in their 50s. In women unscreened in their 50s, the cumulative incidence up to age 80 was 5.0 per 1,000 women, and screening at age 61–65 was associated with a lower risk for cervical cancer (HR = 0.42, 95% CI 0.24–0.72), corresponding to a decrease of 3.3 cancer cases per 1,000 women. A higher cumulative incidence and similarly statistically significant risk decrease was seen for women with abnormal smears in their 50s. In women adequately or inadequately screened with only normal results between age 51 and age 60, the cumulative incidence of cervical cancer from age 61 to 80 was 1.6 and 2.5 per 1,000 women, respectively, and further screening at age 61–65 was not associated with statistically significant decreases of cervical cancer risk up to age 80, but with fewer cancer cases of advanced stages at age 61–65. Adjustment for potential lifestyle confounders was limited.
Conclusions
In this study, cervical screening with cytology at age 61–65 was associated with a statistically significant reduction of subsequent cervical cancer risk for women who were unscreened, or screened with abnormalities, in their 50s. In women screened with normal results in their 50s, the risk for future cancer was not sizeable, and the risk reduction associated with continued screening appeared limited. These findings should inform the current debate regarding age and criteria to discontinue cervical screening.
中文翻译:

根据筛查历史对60岁以下人群进行宫颈筛查的有效性:瑞典全国队列研究
背景
在建立长期宫颈检查的国家中,老年妇女宫颈癌的相对较高发病率一直是人们持续关注的问题。关于何时以及如何停止筛查仍存在争议。现有的基于人口的年龄较大的宫颈筛查有效性研究尚未考虑妇女的筛查史。我们进行了一项全国性队列研究,以调查60岁后宫颈癌的发病率及其与61-65岁时宫颈筛查的相关性,并根据51-60岁时的筛查史进行分层。
方法和发现
通过总人口登记,我们确定了569132名1919年1月1日至1945年12月31日之间出生的妇女,自51岁以来一直居住在瑞典。妇女的细胞学筛查记录,子宫颈癌的发生和FIGO分期(对于诊断为癌症的妇女)均来自美国寄存器和病历表。我们使用生存功能考虑竞争风险,计算了61岁至80岁之间子宫颈癌的累积发生率,并根据Cox模型(针对出生率进行了调整)估算了与61-65岁年龄段筛查状况相关的子宫颈癌风险比(HR)。人群和受教育程度,以50年代女性的筛查历史为条件。在50年代未接受筛查的女性中,直至80岁的累积发病率是每千名女性中有5.0例,在61-65岁之间进行筛查与宫颈癌风险较低(HR = 0.42,95%CI 0.24-0.72),每千名女性减少3.3例癌症病例。在50多岁出现异常涂片的女性中,观察到较高的累积发生率,并且具有类似的统计学上显着的风险降低。在年龄在51岁至60岁之间的筛查结果充分或不足的妇女中,从61至80岁的子宫颈癌的累积发病率分别为每千名女性1.6和2.5,而在61-65岁时进一步筛查与在80岁以下子宫颈癌的风险有统计上的显着降低,但在61-65岁的晚期癌症病例却较少。对潜在的生活方式混杂因素的调整是有限的。000名妇女。在50多岁出现异常涂片的女性中,观察到较高的累积发生率,并且具有类似的统计学上显着的风险降低。在年龄在51岁至60岁之间的筛查结果充分或不足的妇女中,从61至80岁的子宫颈癌的累积发病率分别为每千名女性1.6和2.5,而在61-65岁时进一步筛查与在80岁以下子宫颈癌的风险有统计上的显着降低,但在61-65岁的晚期癌症病例却较少。对潜在的生活方式混杂因素的调整是有限的。000名妇女。在50多岁出现异常涂片的女性中,观察到较高的累积发生率,并且具有类似的统计学上显着的风险降低。在年龄在51岁至60岁之间的筛查结果充分或不足的妇女中,从61至80岁的子宫颈癌的累积发病率分别为每千名女性1.6和2.5,而在61-65岁时进一步筛查与到80岁为止,宫颈癌风险有统计学上的显着降低,但61-65岁的晚期癌症病例却较少。对潜在的生活方式混杂因素的调整是有限的。从61岁到80岁的子宫颈癌的累积发生率分别为每千名女性1.6和2.5,并且在61-65岁时进行进一步筛查与统计学上显着降低直到80岁的子宫颈癌风险没有关联,但是癌症病例较少在61-65岁的晚期阶段。对潜在的生活方式混杂因素的调整是有限的。从61岁到80岁的子宫颈癌的累积发生率分别为每千名女性1.6和2.5,并且在61-65岁时进行进一步筛查与统计学上显着降低直到80岁的子宫颈癌风险没有关联,但是癌症病例较少在61-65岁的晚期阶段。对潜在的生活方式混杂因素的调整是有限的。
结论
在这项研究中,对年龄在60-65岁之间未接受筛查或筛查异常的女性进行宫颈细胞学筛查,其年龄在61-65岁之间,具有统计学意义上的随后子宫颈癌风险的显着降低。在50年代筛查结果正常的女性中,未来患癌症的风险不大,与继续筛查相关的降低风险似乎是有限的。这些发现应为当前关于年龄和终止宫颈筛查的标准的争论提供参考。











































 京公网安备 11010802027423号
京公网安备 11010802027423号