PLOS Medicine ( IF 10.5 ) Pub Date : 2017-11-08 , DOI: 10.1371/journal.pmed.1002431 Paola Castillo , Juan Carlos Hurtado , Miguel J. Martínez , Dercio Jordao , Lucilia Lovane , Mamudo R. Ismail , Carla Carrilho , Cesaltina Lorenzoni , Fabiola Fernandes , Sibone Mocumbi , Zara Onila Jaze , Flora Mabota , Anelsio Cossa , Inacio Mandomando , Pau Cisteró , Alfredo Mayor , Mireia Navarro , Isaac Casas , Jordi Vila , Maria Maixenchs , Khátia Munguambe , Ariadna Sanz , Llorenç Quintó , Eusebio Macete , Pedro Alonso , Quique Bassat , Jaume Ordi , Clara Menéndez
|
Background
Despite global health efforts to reduce maternal mortality, rates continue to be unacceptably high in large parts of the world. Feasible, acceptable, and accurate postmortem sampling methods could provide the necessary evidence to improve the understanding of the real causes of maternal mortality, guiding the design of interventions to reduce this burden.
Methods and findings
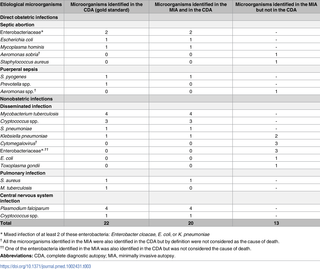
The validity of a minimally invasive autopsy (MIA) method in determining the cause of death was assessed in an observational study in 57 maternal deaths by comparing the results of the MIA with those of the gold standard (complete diagnostic autopsy [CDA], which includes any available clinical information). Concordance between the MIA and the gold standard diagnostic categories was assessed by the kappa statistic, and the sensitivity, specificity, positive and negative predictive values and their 95% confidence intervals (95% CI) to identify the categories of diagnoses were estimated. The main limitation of the study is that both the MIA and the CDA include some degree of subjective interpretation in the attribution of cause of death.
A cause of death was identified in the CDA in 98% (56/57) of cases, with indirect obstetric conditions accounting for 32 (56%) deaths and direct obstetric complications for 24 (42%) deaths. Nonobstetric infectious diseases (22/32, 69%) and obstetric hemorrhage (13/24, 54%) were the most common causes of death among indirect and direct obstetric conditions, respectively. Thirty-six (63%) women were HIV positive, and HIV-related conditions accounted for 16 (28%) of all deaths. Cerebral malaria caused 4 (7%) deaths. The MIA identified a cause of death in 86% of women. The overall concordance of the MIA with the CDA was moderate (kappa = 0.48, 95% CI: 0.31–0.66). Both methods agreed in 68% of the diagnostic categories and the agreement was higher for indirect (91%) than for direct obstetric causes (38%). All HIV infections and cerebral malaria cases were identified in the MIA. The main limitation of the technique is its relatively low performance for identifying obstetric causes of death in the absence of clinical information.
Conclusions
The MIA procedure could be a valuable tool to determine the causes of maternal death, especially for indirect obstetric conditions, most of which are infectious diseases.
The information provided by the MIA could help to prioritize interventions to reduce maternal mortality and to monitor progress towards achieving global health targets.
中文翻译:

莫桑比克微创尸检对确定孕产妇死亡原因的有效性:一项观察性研究
背景
尽管全球为减少孕产妇死亡率做出了健康方面的努力,但在世界大部分地区,其发病率仍然高得令人无法接受。可行,可接受和准确的事后抽样方法可以提供必要的证据,以增进对孕产妇死亡真正原因的了解,从而指导减少此类负担的干预措施的设计。
方法和发现
在一项观察性研究中,通过将MIA和金标准的结果进行比较,对57例孕产妇死亡进行了观察性研究,评估了微创尸检(MIA)方法在确定死亡原因方面的有效性(完全诊断尸检[CDA],其中包括任何可用的临床信息)。MIA和金标准诊断类别之间的一致性通过kappa统计进行了评估,并估计了用于识别诊断类别的敏感性,特异性,阳性和阴性预测值及其95%置信区间(95%CI)。该研究的主要局限性在于,MIA和CDA都在某种程度上对死亡原因进行了主观解释。
在CDA中,有98%(56/57)的病例是死因,间接产科疾病占32(56%)位死亡,直接产科并发症占24(42%)位死亡。非产科传染病(22 / 32,69%)和产科出血(13 / 24,54%)分别是间接和直接产科疾病中最常见的死亡原因。三十六(63%)名妇女为艾滋病毒阳性,与艾滋病毒有关的疾病占所有死亡人数的16(28%)。脑疟疾导致4(7%)人死亡。MIA在86%的女性中确定了死因。MIA与CDA的总体一致性中等(kappa = 0.48,95%CI:0.31-0.66)。两种方法在68%的诊断类别中均相符,间接原因(91%)高于直接产科原因(38%)。在MIA中确定了所有的HIV感染和脑疟疾病例。该技术的主要局限性在于,在缺乏临床信息的情况下,其识别产科死亡原因的性能相对较低。
结论
MIA程序可能是确定孕产妇死亡原因的有价值的工具,特别是对于间接产科疾病(其中大多数是传染病)而言。
MIA提供的信息可以帮助确定干预措施的优先顺序,以降低孕产妇死亡率并监测实现全球卫生目标的进展。









































 京公网安备 11010802027423号
京公网安备 11010802027423号