JAMA Oncology ( IF 22.5 ) Pub Date : 2017-11-01 , DOI: 10.1001/jamaoncol.2017.0973 Jonathan E Leeman 1 , Jin-Gao Li 2 , Xin Pei 1 , Praveen Venigalla 1 , Zachary S Zumsteg 3 , Evangelia Katsoulakis 1 , Eitan Lupovitch 1 , Sean M McBride 1 , Chiaojung J Tsai 1 , Jay O Boyle 4 , Benjamin R Roman 4 , Luc G T Morris 4 , Lara A Dunn 5 , Eric J Sherman 5 , Nancy Y Lee 1 , Nadeem Riaz 1
|
Importance Even though 15% to 50% of patients with head and neck squamous cell carcinoma (HNSCC) experience recurrence, relatively little is known regarding patterns of treatment failure and postrecurrence outcomes after chemoradiotherapy using modern radiation techniques (intensity-modulated radiotherapy [IMRT]). Recurrence patterns are significantly affected by variations in the quality of radiotherapy, which may confound findings from multicenter trials.
Objective To assess patterns of treatment failure and postrecurrence outcomes for patients with HNSCC treated with contemporary radiotherapy techniques.
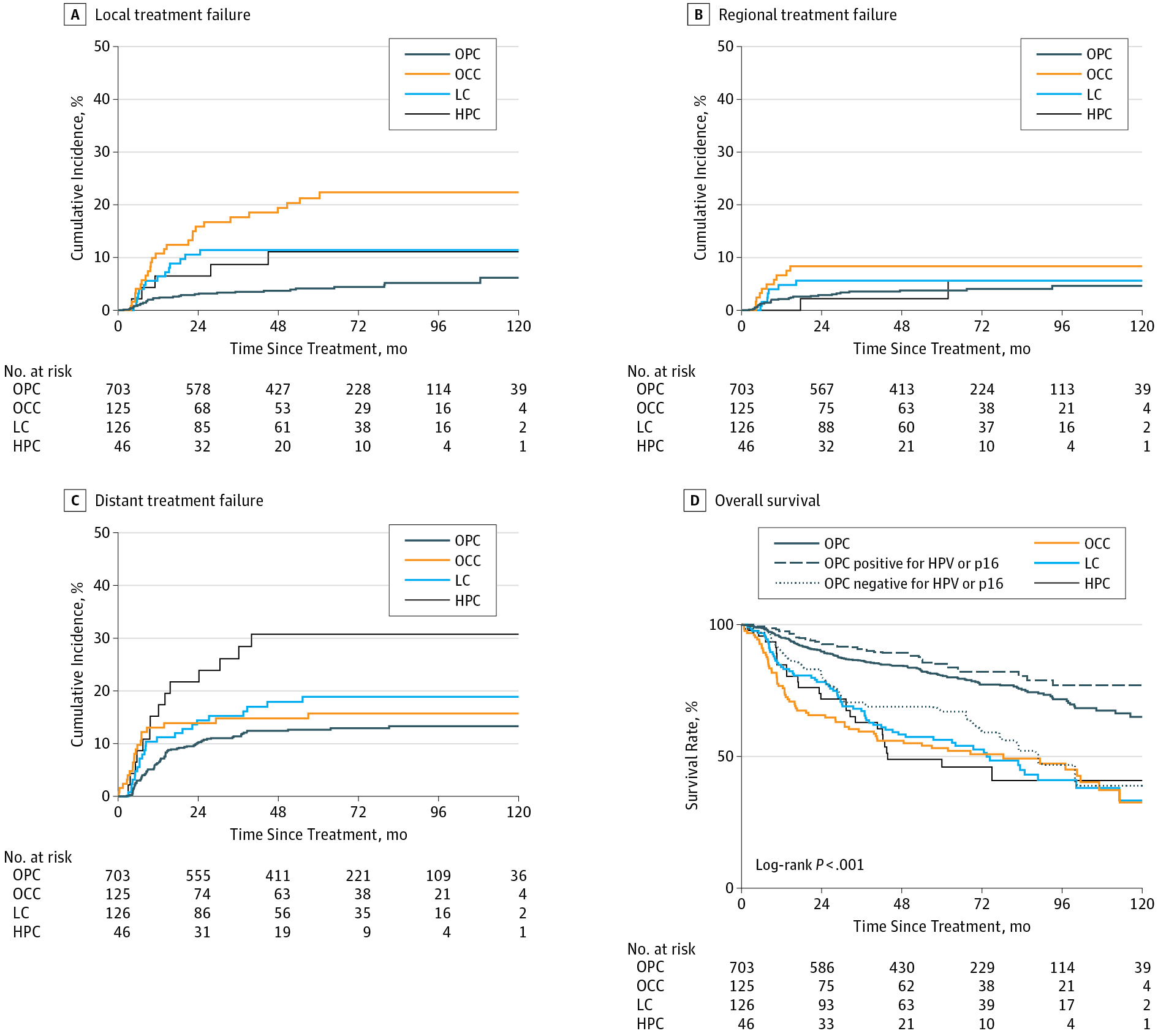
Design, Setting, and Participants This large single-institution cohort study reviewed the outcomes of 1000 consecutive patients with stage III to IVB oropharyngeal carcinoma (n = 703), laryngeal carcinoma (n = 126), or hypopharyngeal carcinoma (n = 46) treated with definitive IMRT with or without concurrent chemotherapy, as well as patients with oral cavity carcinoma (n = 125) treated with postoperative IMRT with or without concurrent systemic therapy, from December 1, 2001, to December 31, 2013, with a median follow-up of 65.1 months among surviving patients. Data analysis was performed from January 31, 2016, to February 17, 2017.
Main Outcomes and Measures Patterns of treatment failure and overall survival following locoregional failure or distant metastasis.
Results Among the 1000 patients (186 women and 814 men; mean [SD] age, 59.3 [10.8] years), there were no marginal or isolated out-of-radiation-field failures. Among subsites, the cumulative incidence of local failure was highest among patients with oral cavity carcinoma vs those with oropharyngeal carcinoma (hazard ratio, 5.2; 95% CI, 3.1-8.6; P < .001). Furthermore, patients with oral cavity carcinoma experienced significantly shorter survival following distant metastasis (hazard ratio, 3.66; 95% CI, 1.98-6.80; P < .001). Patients with oropharyngeal carcinoma positive for human papillomavirus or p16 lived longer after locoregional failure compared with patents with oropharyngeal carcinoma negative for human papillomavirus or p16 (median survival, 36.5 vs 13.6 months; P = .007) but not after distant metastasis. Salvage surgery was associated with improved overall survival following locoregional failure (hazard ratio, 0.51; 95% CI, 0.34-0.77; P = .001); oligometastatic disease (1 vs ≥2 lesions: hazard ratio, 0.32; 95% CI, 0.16-0.63; P = .001) was associated with improved overall survival following distant metastasis.
Conclusions and Relevance Overall survival after recurrence of HNSCC is influenced by the HNSCC subsite and human papillomavirus or p16 status, as well surgical and systemic interventions. An oligometastatic phenotype characterizes patients with solitary metastasis after chemoradiotherapy. These findings have important implications for clinical trial designs for HNSCC in the recurrent and oligometastatic setting.
中文翻译:

使用现代放射技术进行放化疗后局部晚期头颈部鳞状细胞癌患者的治疗失败模式和复发后结果
重要性 尽管 15% 至 50% 的头颈部鳞状细胞癌 (HNSCC) 患者会复发,但对于使用现代放射技术(调强放疗 [IMRT])进行放化疗后的治疗失败模式和复发后结果知之甚少. 复发模式受到放疗质量变化的显着影响,这可能会混淆多中心试验的结果。
目的 评估采用现代放射治疗技术治疗的 HNSCC 患者的治疗失败模式和复发后结果。
设计、设置和参与者 这项大型单机构队列研究回顾了 1000 名连续接受治疗的 III 至 IVB 期口咽癌 (n = 703)、喉癌 (n = 126) 或下咽癌 (n = 46) 患者的结果2001 年 12 月 1 日至 2013 年 12 月 31 日,接受明确 IMRT 联合或不联合同步化疗的患者,以及接受术后 IMRT 联合或不联合全身治疗的口腔癌患者 (n = 125),中位随访时间为在幸存的患者中增加了 65.1 个月。数据分析时间为 2016 年 1 月 31 日至 2017 年 2 月 17 日。
主要结果和措施 局部区域失败或远处转移后治疗失败和总生存期的模式。
结果 在 1000 名患者(186 名女性和 814 名男性;平均 [SD] 年龄,59.3 [10.8] 岁)中,没有边缘或孤立的辐射场外故障。在亚部位中,口腔癌患者与口咽癌患者相比,局部失败的累积发生率最高(风险比,5.2;95% CI,3.1-8.6;P < .001)。此外,口腔癌患者在远处转移后的生存期显着缩短(风险比,3.66;95% CI,1.98-6.80;P < .001)。与人乳头瘤病毒或 p16 阴性口咽癌患者相比,人乳头瘤病毒或 p16 阳性口咽癌患者在局部失败后的寿命更长(中位生存期,36.5 个月 vs 13.6 个月;P = .007)但在远处转移后没有。挽救性手术与改善局部区域失败后的总体生存率相关(风险比,0.51;95% CI,0.34-0.77;P = .001);寡转移性疾病(1 vs ≥2 个病灶:风险比,0.32;95% CI,0.16-0.63;P = 0.001)与远处转移后总生存期的改善相关。
结论和相关 性 HNSCC 复发后的总生存期受 HNSCC 亚位和人乳头瘤病毒或 p16 状态以及手术和全身干预的影响。寡转移表型是放化疗后孤立转移患者的特征。这些发现对复发性和寡转移性 HNSCC 的临床试验设计具有重要意义。











































 京公网安备 11010802027423号
京公网安备 11010802027423号