PLOS Medicine ( IF 10.5 ) Pub Date : 2017-11-07 , DOI: 10.1371/journal.pmed.1002422 Tonia Poteat 1 , Benjamin Ackerman 2 , Daouda Diouf 3 , Nuha Ceesay 4 , Tampose Mothopeng 5 , Ky-Zerbo Odette 6 , Seni Kouanda 7, 8 , Henri Gautier Ouedraogo 7, 8 , Anato Simplice 9 , Abo Kouame 10 , Zandile Mnisi 11 , Gift Trapence 12 , L Leigh Ann van der Merwe 13 , Vicente Jumbe 14 , Stefan Baral 1
|
Introduction
Sub-Saharan Africa bears more than two-thirds of the worldwide burden of HIV; however, data among transgender women from the region are sparse. Transgender women across the world face significant vulnerability to HIV. This analysis aimed to assess HIV prevalence as well as psychosocial and behavioral drivers of HIV infection among transgender women compared with cisgender (non-transgender) men who have sex with men (cis-MSM) in 8 sub-Saharan African countries.
Methods and findings
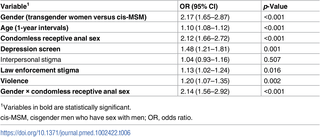
Respondent-driven sampling targeted cis-MSM for enrollment. Data collection took place at 14 sites across 8 countries: Burkina Faso (January–August 2013), Côte d’Ivoire (March 2015–February 2016), The Gambia (July–December 2011), Lesotho (February–September 2014), Malawi (July 2011–March 2012), Senegal (February–November 2015), Swaziland (August–December 2011), and Togo (January–June 2013). Surveys gathered information on sexual orientation, gender identity, stigma, mental health, sexual behavior, and HIV testing. Rapid tests for HIV were conducted. Data were merged, and mixed effects logistic regression models were used to estimate relationships between gender identity and HIV infection. Among 4,586 participants assigned male sex at birth, 937 (20%) identified as transgender or female, and 3,649 were cis-MSM. The mean age of study participants was approximately 24 years, with no difference between transgender participants and cis-MSM. Compared to cis-MSM participants, transgender women were more likely to experience family exclusion (odds ratio [OR] 1.75, 95% CI 1.42–2.16, p < 0.001), rape (OR 1.95, 95% CI 1.63–2.36, p < 0.001), and depressive symptoms (OR 1.30, 95% CI 1.12–1.52, p < 0.001). Transgender women were more likely to report condomless receptive anal sex in the prior 12 months (OR 2.44, 95% CI 2.05–2.90, p < 0.001) and to be currently living with HIV (OR 1.81, 95% CI 1.49–2.19, p < 0.001). Overall HIV prevalence was 25% (235/926) in transgender women and 14% (505/3,594) in cis-MSM. When adjusted for age, condomless receptive anal sex, depression, interpersonal stigma, law enforcement stigma, and violence, and the interaction of gender with condomless receptive anal sex, the odds of HIV infection for transgender women were 2.2 times greater than the odds for cis-MSM (95% CI 1.65–2.87, p < 0.001). Limitations of the study included sampling strategies tailored for cis-MSM and merging of datasets with non-identical survey instruments.
Conclusions
In this study in sub-Saharan Africa, we found that HIV burden and stigma differed between transgender women and cis-MSM, indicating a need to address gender diversity within HIV research and programs.
中文翻译:

8 个非洲国家男男性行为跨性别女性和顺性别男性的艾滋病毒患病率以及行为和心理社会因素:横断面分析
介绍
撒哈拉以南非洲地区承担着全世界三分之二以上的艾滋病毒负担;然而,该地区跨性别女性的数据很少。世界各地的跨性别女性都面临着感染艾滋病毒的严重风险。本分析旨在评估 8 个撒哈拉以南非洲国家中跨性别女性与男男性行为 (cis-MSM) 的顺性别(非跨性别)男性之间的艾滋病毒感染率以及艾滋病毒感染的社会心理和行为驱动因素。
方法和结果
受访者驱动的抽样针对 cis-MSM 进行登记。数据收集在8个国家的14个地点进行:布基纳法索(2013年1月至8月)、科特迪瓦(2015年3月至2016年2月)、冈比亚(2011年7月至12月)、莱索托(2014年2月至9月)、马拉维(2011年7月至2012年3月)、塞内加尔(2015年2月至11月)、斯威士兰(2011年8月至12月)和多哥(2013年1月至6月)。调查收集了有关性取向、性别认同、耻辱、心理健康、性行为和艾滋病毒检测的信息。进行了艾滋病毒快速检测。合并数据,并使用混合效应逻辑回归模型来估计性别认同与艾滋病毒感染之间的关系。在 4,586 名出生时被指定为男性的参与者中,937 名(20%)被确定为跨性别者或女性,3,649 名是顺式 MSM。研究参与者的平均年龄约为 24 岁,跨性别参与者和顺式 MSM 之间没有差异。与顺式 MSM 参与者相比,跨性别女性更有可能遭受家庭排斥(比值比 [OR] 1.75,95% CI 1.42–2.16, p < 0.001)、强奸(OR 1.95,95% CI 1.63–2.36, p < 0.001)和抑郁症状(OR 1.30,95% CI 1.12–1.52, p < 0.001)。跨性别女性更有可能在过去 12 个月内报告无安全套接受性肛交(OR 2.44,95% CI 2.05–2.90, p < 0.001),并且目前感染 HIV(OR 1.81,95% CI 1.49–2.19, p< 0.001)。跨性别女性的 HIV 总体感染率为 25% (235/926),顺式 MSM 的感染率为 14% (505/3,594)。 当根据年龄、无套肛交、抑郁、人际耻辱、执法耻辱和暴力以及性别与无套肛交的相互作用进行调整后,跨性别女性感染艾滋病毒的几率是顺性别女性的 2.2 倍-MSM(95% CI 1.65–2.87, p < 0.001)。该研究的局限性包括针对 cis-MSM 量身定制的抽样策略以及将数据集与不同的调查工具合并。
结论
在撒哈拉以南非洲的这项研究中,我们发现跨性别女性和顺式男男性接触者之间的艾滋病毒负担和耻辱有所不同,这表明需要在艾滋病毒研究和项目中解决性别多样性问题。











































 京公网安备 11010802027423号
京公网安备 11010802027423号