PLOS Medicine ( IF 10.5 ) Pub Date : 2017-09-26 , DOI: 10.1371/journal.pmed.1002392 Marie-Louise H. Rasmussen , Marin Strøm , Jan Wohlfahrt , Poul Videbech , Mads Melbye
|
Background
Some 5%–15% of all women experience postpartum depression (PPD), which for many is their first psychiatric disorder. The purpose of this study was to estimate the incidence of postpartum affective disorder (AD), duration of treatment, and rate of subsequent postpartum AD and other affective episodes in a nationwide cohort of women with no prior psychiatric history.
Methods and findings
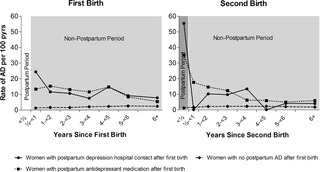
Linking information from several Danish national registers, we constructed a cohort of 457,317 primiparous mothers with first birth (and subsequent births) from 1 January 1996 to 31 December 2013 (a total of 789,068 births) and no prior psychiatric hospital contacts and/or use of antidepressants. These women were followed from 1 January 1996 to 31 December 2014. Postpartum AD was defined as use of antidepressants and/or hospital contact for PPD within 6 months after childbirth. The main outcome measures were risk of postpartum AD, duration of treatment, and recurrence risk. We observed 4,550 (0.6%) postpartum episodes of AD. The analyses of treatment duration showed that 1 year after the initiation of treatment for their first episode, 27.9% of women were still in treatment; after 4 years, 5.4%. The recurrence risk of postpartum AD for women with a PPD hospital contact after first birth was 55.4 per 100 person-years; for women with postpartum antidepressant medication after first birth, it was 35.0 per 100 person-years. The rate of postpartum AD after second birth for women with no history of postpartum AD was 1.2 per 100 person-years. After adjusting for year of birth and mother’s age, women with PPD hospital contact after first birth had a 46.4 times higher rate (95% CI 31.5–68.4) and women with postpartum antidepressant medication after their first birth had a 26.9 times higher rate (95% CI 21.9–33.2) of a recurrent postpartum episode after their second birth compared to women with no postpartum AD history. Limitations include the use of registry data to identify cases and limited confounder control.
Conclusions
In this study, an episode of postpartum AD was observed for 0.6% of childbirths among women with no prior psychiatric history. The observed episodes were characterized by a relatively short treatment duration, yet the women had a notably high rate of later AD and recurrent episodes of postpartum AD. The recurrence risk of postpartum AD was markedly higher among women with PPD hospital contact after first birth compared to women with postpartum antidepressant medication after first birth. Our results underline the necessity of measures targeted at specific vulnerable groups, such as women who experience PPD as a first psychiatric episode.
中文翻译:

无精神病史的女性产后情感障碍的风险,治疗持续时间和复发风险:一项基于人群的队列研究
背景
所有妇女中约有5%–15%患有产后抑郁症(PPD),对许多人来说,这是她们的第一种精神病。这项研究的目的是评估全国范围内没有既往精神病史的女性队列中的产后情感障碍(AD)的发生率,治疗时间以及随后的产后AD和其他情感发作的发生率。
方法和发现
结合丹麦多个国家/地区的登记信息,我们建立了457,317例初产母亲的队列,这些母亲在1996年1月1日至2013年12月31日期间出生(共789,068例),并且没有事先与精神病医院联系和/或使用过抗抑郁药。自1996年1月1日至2014年12月31日对这些妇女进行随访。产后AD定义为在分娩后6个月内使用抗抑郁药和/或医院接触PPD。主要的预后指标是产后AD的风险,治疗的持续时间和复发风险。我们观察到4,550(0.6%)的AD产后发作。对治疗持续时间的分析表明,开始治疗第一年后的第一年,仍有27.9%的妇女仍在接受治疗。4年后为5.4%。PPD医院接触的妇女在首次分娩后发生产后AD的复发风险为每100人年55.4。对于第一胎后产后服用抗抑郁药的妇女,每100人年为35.0。没有产后AD史的妇女第二胎后产后AD的发生率为每100人年1.2。在对出生年份和母亲的年龄进行调整后,第一次出生后与PPD医院接触的妇女发生率高46.4倍(95%CI 31.5-68.4),而第一次出生后有产后抗抑郁药的妇女发生率高26.9倍(95)与没有产后AD史的女性相比,第二胎后复发性产后发作的百分比CI 21.9–33.2)。局限性包括使用注册表数据来识别案例和有限的混杂因素控制。
结论
在这项研究中,没有精神病史的女性中约有0.6%的分娩发生了AD发作。所观察到的发作以相对较短的治疗持续时间为特征,但这些妇女的晚期AD和产后AD复发发作的发生率显着较高。与第一胎后服用抗抑郁药的妇女相比,第一胎后接触PPD医院的妇女产后AD的复发风险明显更高。我们的结果表明,有必要针对特定的弱势群体采取措施,例如将PPD视为首次精神病发作的妇女。











































 京公网安备 11010802027423号
京公网安备 11010802027423号