PLOS Neglected Tropical Diseases ( IF 3.4 ) Pub Date : 2017-09-08 , DOI: 10.1371/journal.pntd.0005901 Ruth Monyenye Nyangacha 1, 2 , David Odongo 2 , Florence Oyieke 2 , Missiani Ochwoto 3 , Richard Korir 4 , Ronald Kiprotich Ngetich 4 , Gladys Nginya 1 , Olipher Makwaga 5 , Christine Bii 4 , Peter Mwitari 1 , Festus Tolo 1
|
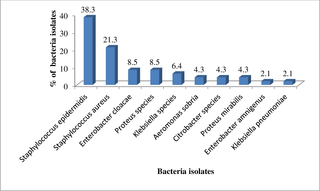
Tungiasis or jigger infestation is a parasitic disease caused by the female sand flea Tunga penetrans. Secondary infection of the lesions caused by this flea is common in endemic communities. This study sought to shed light on the bacterial pathogens causing secondary infections in tungiasis lesions and their susceptibility profiles to commonly prescribed antibiotics. Participants were recruited with the help of Community Health Workers. Swabs were taken from lesions which showed signs of secondary infection. Identification of suspected bacteria colonies was done by colony morphology, Gram staining, and biochemical tests. The Kirby Bauer disc diffusion test was used to determine the drug susceptibility profiles. Out of 37 participants, from whom swabs were collected, specimen were positive in 29 and 8 had no growth. From these, 10 different strains of bacteria were isolated. Two were Gram positive bacteria and they were, Staphylocccus epidermidis (38.3%) and Staphylococcus aureus (21.3%). Eight were Gram negative namely Enterobacter cloacae (8.5%), Proteus species (8.5%), Klebsiellla species (6.4%), Aeromonas sobria (4.3%), Citrobacter species (4.3%), Proteus mirabillis(4.3%), Enterobacter amnigenus (2.1%) and Klebsiella pneumoniae (2.1%). The methicillin resistant S. aureus (MRSA) isolated were also resistant to clindamycin, kanamycin, erythromycin, nalidixic acid, trimethorprim sulfamethoxazole and tetracycline. All the Gram negative and Gram positive bacteria isolates were sensitive to gentamicin and norfloxacin drugs. Results from this study confirms the presence of resistant bacteria in tungiasis lesions hence highlighting the significance of secondary infection of the lesions in endemic communties. This therefore suggests that antimicrobial susceptibility testing may be considered to guide in identification of appropriate antibiotics and treatment therapy among tungiasis patients.
中文翻译:

肯尼亚西部地区沙棘病患者的继发细菌感染和抗生素耐药性
Tungiasis 或 jigger infestation 是一种由雌性沙蚤Tunga penetrans引起的寄生虫病。由这种跳蚤引起的病变继发感染在流行社区中很常见。这项研究旨在揭示引起圆线虫病病变继发感染的细菌病原体及其对常用抗生素的敏感性。参与者是在社区卫生工作者的帮助下招募的。从显示继发感染迹象的病灶中采集拭子。通过菌落形态、革兰氏染色和生化测试来鉴定可疑细菌菌落。 Kirby Bauer 纸片扩散试验用于确定药物敏感性曲线。在采集了拭子的 37 名参与者中,29 人的样本呈阳性,8 人没有生长。从这些细菌中分离出 10 种不同的细菌菌株。两种是革兰氏阳性菌,它们是表皮葡萄球菌(38.3%)和金黄色葡萄球菌(21.3%)。八种为革兰氏阴性菌,即阴沟肠杆菌(8.5%)、变形杆菌属(8.5%)、克雷伯氏菌属(6.4%)、普通气单胞菌(4.3%)、柠檬酸杆菌属(4.3%)、奇异变形杆菌(4.3%)、羊肠杆菌( 2.1%)和肺炎克雷伯菌(2.1%)。耐甲氧西林S .分离出的金黄色葡萄球菌(MRSA) 也对克林霉素、卡那霉素、红霉素、萘啶酸、甲氧苄啶、磺胺甲恶唑和四环素具有耐药性。所有革兰氏阴性和革兰氏阳性细菌分离株均对庆大霉素和诺氟沙星药物敏感。 这项研究的结果证实了圆线虫病病变中存在耐药细菌,因此强调了流行社区中病变继发感染的重要性。因此,这表明抗菌药物敏感性测试可被考虑指导在盾虫病患者中确定适当的抗生素和治疗方案。











































 京公网安备 11010802027423号
京公网安备 11010802027423号