当前位置:
X-MOL 学术
›
JAMA Pediatr.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2017-09-01 , DOI: 10.1001/jamapediatrics.2017.1689 Iona Novak 1 , Cathy Morgan 1 , Lars Adde 2 , James Blackman 3 , Roslyn N Boyd 4 , Janice Brunstrom-Hernandez 5 , Giovanni Cioni 6 , Diane Damiano 7 , Johanna Darrah 8 , Ann-Christin Eliasson 9 , Linda S de Vries 10 , Christa Einspieler 11 , Michael Fahey 12 , Darcy Fehlings 13 , Donna M Ferriero 14 , Linda Fetters 15 , Simona Fiori 6 , Hans Forssberg 9 , Andrew M Gordon 16 , Susan Greaves 17 , Andrea Guzzetta 6 , Mijna Hadders-Algra 18 , Regina Harbourne 19 , Angelina Kakooza-Mwesige 20 , Petra Karlsson 1 , Lena Krumlinde-Sundholm 9 , Beatrice Latal 21 , Alison Loughran-Fowlds 22 , Nathalie Maitre 23 , Sarah McIntyre 1 , Garey Noritz 23 , Lindsay Pennington 24 , Domenico M Romeo 25 , Roberta Shepherd 26 , Alicia J Spittle 27 , Marelle Thornton 1 , Jane Valentine 28 , Karen Walker 1, 22 , Robert White 1 , Nadia Badawi 1, 22
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2017-09-01 , DOI: 10.1001/jamapediatrics.2017.1689 Iona Novak 1 , Cathy Morgan 1 , Lars Adde 2 , James Blackman 3 , Roslyn N Boyd 4 , Janice Brunstrom-Hernandez 5 , Giovanni Cioni 6 , Diane Damiano 7 , Johanna Darrah 8 , Ann-Christin Eliasson 9 , Linda S de Vries 10 , Christa Einspieler 11 , Michael Fahey 12 , Darcy Fehlings 13 , Donna M Ferriero 14 , Linda Fetters 15 , Simona Fiori 6 , Hans Forssberg 9 , Andrew M Gordon 16 , Susan Greaves 17 , Andrea Guzzetta 6 , Mijna Hadders-Algra 18 , Regina Harbourne 19 , Angelina Kakooza-Mwesige 20 , Petra Karlsson 1 , Lena Krumlinde-Sundholm 9 , Beatrice Latal 21 , Alison Loughran-Fowlds 22 , Nathalie Maitre 23 , Sarah McIntyre 1 , Garey Noritz 23 , Lindsay Pennington 24 , Domenico M Romeo 25 , Roberta Shepherd 26 , Alicia J Spittle 27 , Marelle Thornton 1 , Jane Valentine 28 , Karen Walker 1, 22 , Robert White 1 , Nadia Badawi 1, 22
Affiliation
|
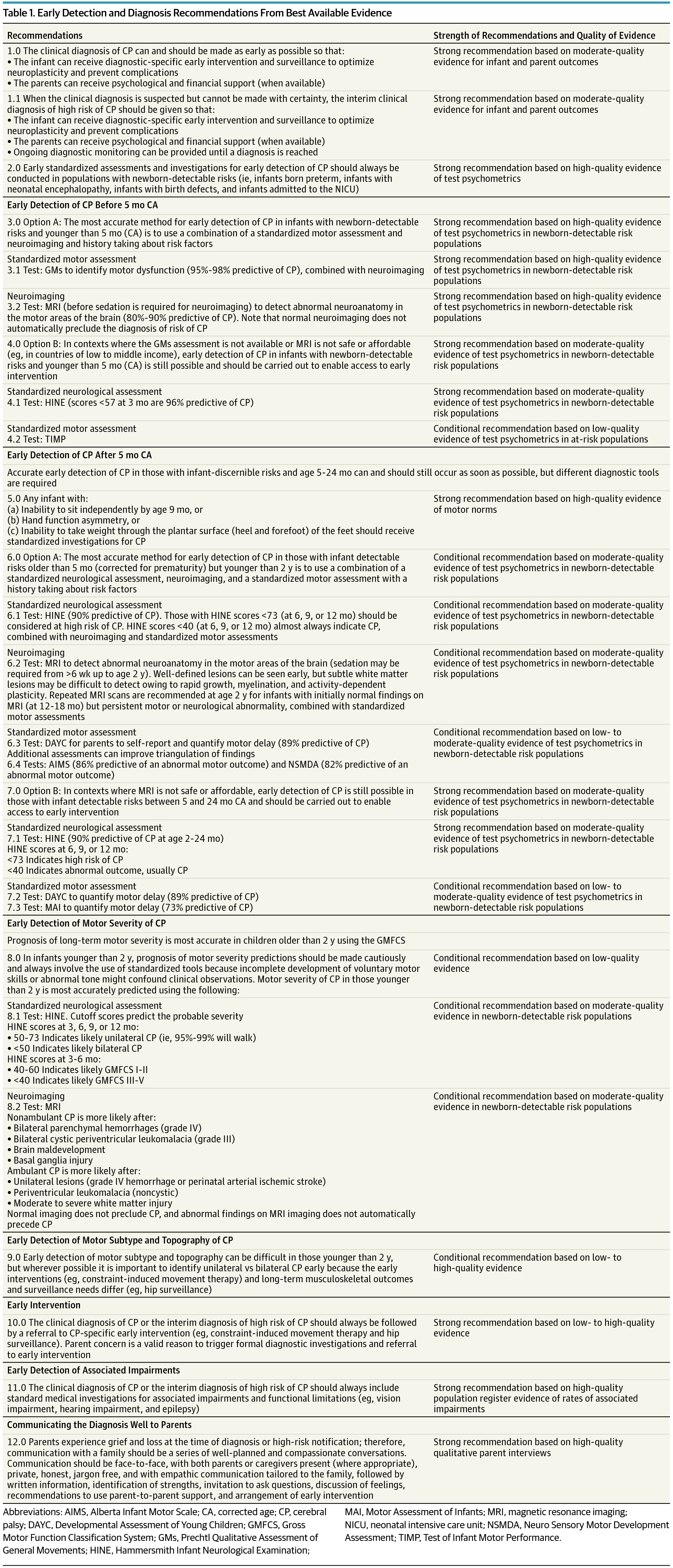
Importance Cerebral palsy describes the most common physical disability in childhood and occurs in 1 in 500 live births. Historically, the diagnosis has been made between age 12 and 24 months but now can be made before 6 months’ corrected age. Objectives To systematically review best available evidence for early, accurate diagnosis of cerebral palsy and to summarize best available evidence about cerebral palsy–specific early intervention that should follow early diagnosis to optimize neuroplasticity and function. Evidence Review This study systematically searched the literature about early diagnosis of cerebral palsy in MEDLINE (1956-2016), EMBASE (1980-2016), CINAHL (1983-2016), and the Cochrane Library (1988-2016) and by hand searching. Search terms included cerebral palsy, diagnosis, detection, prediction, identification, predictive validity, accuracy, sensitivity, and specificity. The study included systematic reviews with or without meta-analyses, criteria of diagnostic accuracy, and evidence-based clinical guidelines. Findings are reported according to the PRISMA statement, and recommendations are reported according to the Appraisal of Guidelines, Research and Evaluation (AGREE) II instrument. Findings Six systematic reviews and 2 evidence-based clinical guidelines met inclusion criteria. All included articles had high methodological Quality Assessment of Diagnostic Accuracy Studies (QUADAS) ratings. In infants, clinical signs and symptoms of cerebral palsy emerge and evolve before age 2 years; therefore, a combination of standardized tools should be used to predict risk in conjunction with clinical history. Before 5 months’ corrected age, the most predictive tools for detecting risk are term-age magnetic resonance imaging (86%-89% sensitivity), the Prechtl Qualitative Assessment of General Movements (98% sensitivity), and the Hammersmith Infant Neurological Examination (90% sensitivity). After 5 months’ corrected age, the most predictive tools for detecting risk are magnetic resonance imaging (86%-89% sensitivity) (where safe and feasible), the Hammersmith Infant Neurological Examination (90% sensitivity), and the Developmental Assessment of Young Children (83% C index). Topography and severity of cerebral palsy are more difficult to ascertain in infancy, and magnetic resonance imaging and the Hammersmith Infant Neurological Examination may be helpful in assisting clinical decisions. In high-income countries, 2 in 3 individuals with cerebral palsy will walk, 3 in 4 will talk, and 1 in 2 will have normal intelligence. Conclusions and Relevance Early diagnosis begins with a medical history and involves using neuroimaging, standardized neurological, and standardized motor assessments that indicate congruent abnormal findings indicative of cerebral palsy. Clinicians should understand the importance of prompt referral to diagnostic-specific early intervention to optimize infant motor and cognitive plasticity, prevent secondary complications, and enhance caregiver well-being.
中文翻译:

脑瘫的早期、准确诊断和早期干预
重要性 脑瘫是儿童时期最常见的身体残疾,每 500 名活产婴儿中就有 1 人发生脑瘫。历史上,诊断是在 12 至 24 个月之间做出的,但现在可以在 6 个月的校正年龄之前做出。目的 系统地回顾早期、准确诊断脑瘫的最佳现有证据,并总结有关脑瘫特异性早期干预的最佳现有证据,这些早期干预应遵循早期诊断,以优化神经可塑性和功能。证据回顾本研究系统检索了MEDLINE(1956-2016)、EMBASE(1980-2016)、CINAHL(1983-2016)和Cochrane图书馆(1988-2016)中关于脑瘫早期诊断的文献并手工检索。搜索术语包括脑瘫、诊断、检测、预测、识别、预测有效性、准确性、敏感性和特异性。该研究包括有或没有荟萃分析的系统评价、诊断准确性标准和循证临床指南。研究结果根据 PRISMA 声明进行报告,建议根据指南、研究和评估 (AGREE) II 工具进行评估。结果 6 项系统评价和 2 项循证临床指南符合纳入标准。所有纳入的文章均具有较高的诊断准确性研究方法质量评估 (QUADAS) 评级。在婴儿中,脑瘫的临床体征和症状在 2 岁之前出现并发展;因此,应结合临床病史结合使用标准化工具来预测风险。 在 5 个月校正年龄之前,检测风险的最具预测性的工具是足月磁共振成像(86%-89% 敏感性)、Prechtl 全身运动定性评估(98% 敏感性)和 Hammersmith 婴儿神经学检查( 90% 灵敏度)。校正年龄 5 个月后,检测风险的最具预测性的工具是磁共振成像(86%-89% 敏感性)(在安全可行的情况下)、Hammersmith 婴儿神经检查(90% 敏感性)和青少年发育评估儿童(C 指数 83%)。脑瘫的地形和严重程度在婴儿期更难以确定,磁共振成像和哈默史密斯婴儿神经学检查可能有助于协助临床决策。在高收入国家,三分之二的脑瘫患者会走路,四分之三的人会说话,二分之一的人智力正常。结论和相关性早期诊断从病史开始,涉及使用神经影像学、标准化神经学和标准化运动评估,以表明一致的异常结果表明脑瘫。临床医生应了解及时转诊进行针对诊断的早期干预的重要性,以优化婴儿运动和认知可塑性、预防继发并发症并提高护理人员的福祉。
更新日期:2017-09-01
中文翻译:

脑瘫的早期、准确诊断和早期干预
重要性 脑瘫是儿童时期最常见的身体残疾,每 500 名活产婴儿中就有 1 人发生脑瘫。历史上,诊断是在 12 至 24 个月之间做出的,但现在可以在 6 个月的校正年龄之前做出。目的 系统地回顾早期、准确诊断脑瘫的最佳现有证据,并总结有关脑瘫特异性早期干预的最佳现有证据,这些早期干预应遵循早期诊断,以优化神经可塑性和功能。证据回顾本研究系统检索了MEDLINE(1956-2016)、EMBASE(1980-2016)、CINAHL(1983-2016)和Cochrane图书馆(1988-2016)中关于脑瘫早期诊断的文献并手工检索。搜索术语包括脑瘫、诊断、检测、预测、识别、预测有效性、准确性、敏感性和特异性。该研究包括有或没有荟萃分析的系统评价、诊断准确性标准和循证临床指南。研究结果根据 PRISMA 声明进行报告,建议根据指南、研究和评估 (AGREE) II 工具进行评估。结果 6 项系统评价和 2 项循证临床指南符合纳入标准。所有纳入的文章均具有较高的诊断准确性研究方法质量评估 (QUADAS) 评级。在婴儿中,脑瘫的临床体征和症状在 2 岁之前出现并发展;因此,应结合临床病史结合使用标准化工具来预测风险。 在 5 个月校正年龄之前,检测风险的最具预测性的工具是足月磁共振成像(86%-89% 敏感性)、Prechtl 全身运动定性评估(98% 敏感性)和 Hammersmith 婴儿神经学检查( 90% 灵敏度)。校正年龄 5 个月后,检测风险的最具预测性的工具是磁共振成像(86%-89% 敏感性)(在安全可行的情况下)、Hammersmith 婴儿神经检查(90% 敏感性)和青少年发育评估儿童(C 指数 83%)。脑瘫的地形和严重程度在婴儿期更难以确定,磁共振成像和哈默史密斯婴儿神经学检查可能有助于协助临床决策。在高收入国家,三分之二的脑瘫患者会走路,四分之三的人会说话,二分之一的人智力正常。结论和相关性早期诊断从病史开始,涉及使用神经影像学、标准化神经学和标准化运动评估,以表明一致的异常结果表明脑瘫。临床医生应了解及时转诊进行针对诊断的早期干预的重要性,以优化婴儿运动和认知可塑性、预防继发并发症并提高护理人员的福祉。











































 京公网安备 11010802027423号
京公网安备 11010802027423号