当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
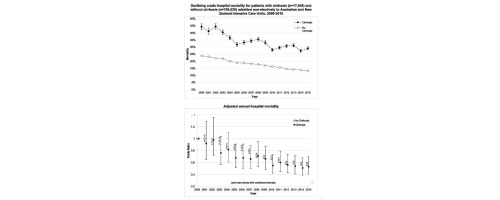
Declining mortality in critically ill patients with cirrhosis in Australia and New Zealand between 2000 and 2015
Journal of Hepatology ( IF 26.8 ) Pub Date : 2017-12-01 , DOI: 10.1016/j.jhep.2017.07.024 Avik Majumdar , Michael Bailey , William M. Kemp , Rinaldo Bellomo , Stuart K. Roberts , David Pilcher
Journal of Hepatology ( IF 26.8 ) Pub Date : 2017-12-01 , DOI: 10.1016/j.jhep.2017.07.024 Avik Majumdar , Michael Bailey , William M. Kemp , Rinaldo Bellomo , Stuart K. Roberts , David Pilcher
|
BACKGROUND & AIMS
Few studies have described the outcomes of patients with cirrhosis receiving intensive care unit (ICU) admission at a population level. We aimed to describe trends in the mortality of such patients in Australia and New Zealand (ANZ), and to investigate the relationship with associated organ failures. METHODS
We studied patients admitted to 172 ICUs on a non-elective basis, with and without cirrhosis between January 1st 2000 and December 31st 2015, as recorded by the ANZ Intensive Care Society Centre for Outcome and Resource Evaluation Adult Patient Database. We assessed severity of illness on admission using organ failure models and acute physiology scores. The primary outcome was hospital mortality. RESULTS
Patients with cirrhosis accounted for 17,044 of 776,873 non-elective ICU admissions (2.2%). Cirrhosis hospital mortality was 32.4% compared to 16.9% in the non-cirrhotic group (p<0.0001). After adjustment for key confounders, cirrhosis had an independent effect on mortality with an odds ratio (OR) of 1.10 (1.06-1.15). There was no difference in the adjusted annual decline in mortality between patients with or without cirrhosis (OR 0.96 [0.95-0.97] vs. 0.96 [0.96-0.96], p=0.67). No difference was seen in the adjusted decline in mortality of patients with cirrhosis when stratified by mechanical ventilation (p=0.92), liver transplant centre status (p=0.27) or presence of sepsis (p=0.09). Mortality increased with number of organ failures, however, the presence of cirrhosis was not found to affect this relationship (p=0.33). CONCLUSIONS
The mortality of patients with cirrhosis admitted to ICU on a non-elective basis has declined significantly over time, comparable to patients without cirrhosis, and is predominantly governed by the number of organ failures. Outcomes are similar between non-liver transplant ICUs and liver transplant centres. LAY SUMMARY
The outcomes of patients with liver cirrhosis admitted to intensive care units (ICUs) have been previously regarded as poor. We have demonstrated that in Australia and New Zealand, annual in-hospital death rates following ICU admission in this patient group are lower than previously reported, have improved over 16years to 29% and are at a rate similar to patients without cirrhosis. Our data justify recommendations that advocate better access to intensive care for patients with cirrhosis.
中文翻译:

2000 年至 2015 年澳大利亚和新西兰肝硬化危重患者死亡率下降
背景和目的 很少有研究描述了在人群水平上接受重症监护病房 (ICU) 入住的肝硬化患者的结果。我们旨在描述澳大利亚和新西兰 (ANZ) 此类患者的死亡率趋势,并调查与相关器官衰竭的关系。方法 我们研究了 2000 年 1 月 1 日至 2015 年 12 月 31 日期间非选择性入住 172 间 ICU 的患者,这些患者由 ANZ 重症监护协会结果和资源评估成人患者数据库记录,有无肝硬化。我们使用器官衰竭模型和急性生理学评分评估入院时疾病的严重程度。主要结果是住院死亡率。结果 776,873 名非选择性入住 ICU 的患者中有 17,044 名肝硬化患者 (2.2%)。肝硬化住院死亡率为 32.4%,而非肝硬化组为 16.9%(p<0.0001)。调整关键混杂因素后,肝硬化对死亡率有独立影响,优势比 (OR) 为 1.10 (1.06-1.15)。有或没有肝硬化的患者在调整后死亡率的年下降率方面没有差异(OR 0.96 [0.95-0.97] vs. 0.96 [0.96-0.96],p=0.67)。当按机械通气 (p=0.92)、肝移植中心状态 (p=0.27) 或存在败血症 (p=0.09) 进行分层时,肝硬化患者的调整后死亡率下降没有差异。死亡率随着器官衰竭的数量而增加,然而,未发现肝硬化的存在影响这种关系(p = 0.33)。结论 非选择性入住 ICU 的肝硬化患者的死亡率随着时间的推移显着下降,与没有肝硬化的患者相当,并且主要受器官衰竭数量的影响。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。与没有肝硬化的患者相当,并且主要受器官衰竭的数量控制。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。与没有肝硬化的患者相当,并且主要受器官衰竭的数量控制。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。该患者组入住 ICU 后的年度院内死亡率低于之前报告的,在 16 年中已提高至 29%,与非肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。该患者组入住 ICU 后的年度院内死亡率低于之前报告的,在 16 年中已提高至 29%,与非肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。
更新日期:2017-12-01
中文翻译:

2000 年至 2015 年澳大利亚和新西兰肝硬化危重患者死亡率下降
背景和目的 很少有研究描述了在人群水平上接受重症监护病房 (ICU) 入住的肝硬化患者的结果。我们旨在描述澳大利亚和新西兰 (ANZ) 此类患者的死亡率趋势,并调查与相关器官衰竭的关系。方法 我们研究了 2000 年 1 月 1 日至 2015 年 12 月 31 日期间非选择性入住 172 间 ICU 的患者,这些患者由 ANZ 重症监护协会结果和资源评估成人患者数据库记录,有无肝硬化。我们使用器官衰竭模型和急性生理学评分评估入院时疾病的严重程度。主要结果是住院死亡率。结果 776,873 名非选择性入住 ICU 的患者中有 17,044 名肝硬化患者 (2.2%)。肝硬化住院死亡率为 32.4%,而非肝硬化组为 16.9%(p<0.0001)。调整关键混杂因素后,肝硬化对死亡率有独立影响,优势比 (OR) 为 1.10 (1.06-1.15)。有或没有肝硬化的患者在调整后死亡率的年下降率方面没有差异(OR 0.96 [0.95-0.97] vs. 0.96 [0.96-0.96],p=0.67)。当按机械通气 (p=0.92)、肝移植中心状态 (p=0.27) 或存在败血症 (p=0.09) 进行分层时,肝硬化患者的调整后死亡率下降没有差异。死亡率随着器官衰竭的数量而增加,然而,未发现肝硬化的存在影响这种关系(p = 0.33)。结论 非选择性入住 ICU 的肝硬化患者的死亡率随着时间的推移显着下降,与没有肝硬化的患者相当,并且主要受器官衰竭数量的影响。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。与没有肝硬化的患者相当,并且主要受器官衰竭的数量控制。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。与没有肝硬化的患者相当,并且主要受器官衰竭的数量控制。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。非肝移植重症监护病房和肝移植中心的结果相似。常规总结 入住重症监护病房 (ICU) 的肝硬化患者的预后以前一直被认为是很差的。我们已经证明,在澳大利亚和新西兰,该患者组入住 ICU 后的年院内死亡率低于之前报告的,16 年来已提高至 29%,与无肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。该患者组入住 ICU 后的年度院内死亡率低于之前报告的,在 16 年中已提高至 29%,与非肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。该患者组入住 ICU 后的年度院内死亡率低于之前报告的,在 16 年中已提高至 29%,与非肝硬化患者的死亡率相似。我们的数据证明了提倡肝硬化患者更好地获得重症监护的建议。











































 京公网安备 11010802027423号
京公网安备 11010802027423号