当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Clinical outcomes of donation after circulatory death liver transplantation in primary sclerosing cholangitis
Journal of Hepatology ( IF 26.8 ) Pub Date : 2017-11-01 , DOI: 10.1016/j.jhep.2017.06.027 Palak J. Trivedi , Irene Scalera , Emma Slaney , Richard W. Laing , Bridget Gunson , Gideon M. Hirschfield , Andrea Schlegel , James Ferguson , Paolo Muiesan
Journal of Hepatology ( IF 26.8 ) Pub Date : 2017-11-01 , DOI: 10.1016/j.jhep.2017.06.027 Palak J. Trivedi , Irene Scalera , Emma Slaney , Richard W. Laing , Bridget Gunson , Gideon M. Hirschfield , Andrea Schlegel , James Ferguson , Paolo Muiesan
|
BACKGROUND & AIM
Primary sclerosing cholangitis (PSC) is a progressive fibro-inflammatory cholangiopathy for which liver transplantation is the only life-extending intervention. These patients may benefit from accepting liver donation after circulatory death (DCD), however their subsequent outcome is unknown. The aim of this study was to determine the clinical impact of using DCD liver grafts in patients specifically undergoing transplantation for PSC. METHODS
Clinical outcomes were prospectively evaluated in PSC patients undergoing transplantation from 2006 to 2016 stratified by donor type (DCD, n=35 vs. donation after brainstem death [DBD], n=108). RESULTS
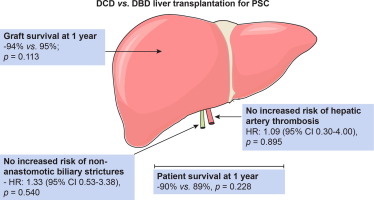
In liver transplantation for PSC; operating time, days requiring critical care support, total ventilator days, incidence of acute kidney injury, need for renal replacement therapy (RRT) or total days requiring RRT were not significantly different between DCD vs. DBD recipients. Although the incidence of ischaemic-type biliary lesions was greater in the DCD group (incidence rate [IR]: 4.4 vs. 0 cases/100-patient-years; p<0.001) there was no increased risk of post-transplant biliary strictures overall (hazard ratio [HR]: 1.20, 0.58-2.46; p=0.624), or in sub-analysis specific to anastomotic strictures or recurrent PSC, between donor types. Graft loss and mortality rates were not significantly different following transplantation with DCD vs. DBD livers (IR: 3.6 vs. 3.1 cases/100-patient-years, p=0.34; and 3.9 vs. 4.7, p=0.6; respectively). DCD liver transplantation in PSC did not impart a heightened risk of graft loss (HR: 1.69, 0.58-4.95, p=0.341) or patient mortality (0.75, 0.25-2.21, p=0.598). CONCLUSION
Transplantation with DCD (vs. DBD) livers in PSC patients does not impact graft loss or patient survival. In an era of organ shortage, DCD grafts represent a viable therapeutic option for liver transplantation in PSC patients. Lay summary: This study examines the impact of liver transplantation in primary sclerosing cholangitis (PSC) with organs donated after circulatory death (DCD), compared to donation after brainstem death (DBD). We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. In an era of organ shortage and increasing wait-list times, DCD livers represent a potential treatment option for transplantation in PSC.
中文翻译:

原发性硬化性胆管炎循环死亡肝移植后捐献的临床结局
背景与目的 原发性硬化性胆管炎 (PSC) 是一种进行性纤维炎性胆管病,肝移植是唯一延长生命的干预措施。这些患者在循环死亡 (DCD) 后接受肝脏捐赠可能会受益,但他们的后续结果尚不清楚。本研究的目的是确定在专门接受 PSC 移植的患者中使用 DCD 肝移植物的临床影响。方法 前瞻性评估 2006 年至 2016 年接受移植的 PSC 患者的临床结果,这些患者按供体类型(DCD,n=35 与脑干死亡后捐赠 [DBD],n=108)分层。结果 PSC 肝移植;手术时间、需要重症监护支持的天数、呼吸机总天数、急性肾损伤的发生率、DCD 与 DBD 受者之间需要肾脏替代治疗 (RRT) 或需要 RRT 的总天数没有显着差异。尽管 DCD 组缺血型胆道病变的发生率更高(发病率 [IR]:4.4 对 0 例/100 患者年;p<0.001),但总体上没有增加移植后胆道狭窄的风险(风险比 [HR]:1.20,0.58-2.46;p=0.624),或在特定于吻合口狭窄或复发性 PSC 的亚组分析中,供体类型之间。DCD 与 DBD 肝脏移植后,移植物丢失率和死亡率没有显着差异(IR:分别为 3.6 与 3.1 例/100 患者年,p=0.34;3.9 与 4.7,p=0.6;)。PSC 中的 DCD 肝移植不会增加移植物丢失的风险(HR:1.69,0.58-4.95,p=0.341)或患者死亡率(0.75,0.25-2.21,p=0.598)。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DBD) PSC 患者的肝脏不影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DBD) PSC 患者的肝脏不影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DCD 移植物代表了 PSC 患者肝移植的可行治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DCD 移植物代表了 PSC 患者肝移植的可行治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。本研究检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,与脑干死亡 (DBD) 后捐赠的器官相比,循环死亡 (DCD) 后捐赠的器官。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。本研究检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,与脑干死亡 (DBD) 后捐赠的器官相比,循环死亡 (DCD) 后捐赠的器官。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。
更新日期:2017-11-01
中文翻译:

原发性硬化性胆管炎循环死亡肝移植后捐献的临床结局
背景与目的 原发性硬化性胆管炎 (PSC) 是一种进行性纤维炎性胆管病,肝移植是唯一延长生命的干预措施。这些患者在循环死亡 (DCD) 后接受肝脏捐赠可能会受益,但他们的后续结果尚不清楚。本研究的目的是确定在专门接受 PSC 移植的患者中使用 DCD 肝移植物的临床影响。方法 前瞻性评估 2006 年至 2016 年接受移植的 PSC 患者的临床结果,这些患者按供体类型(DCD,n=35 与脑干死亡后捐赠 [DBD],n=108)分层。结果 PSC 肝移植;手术时间、需要重症监护支持的天数、呼吸机总天数、急性肾损伤的发生率、DCD 与 DBD 受者之间需要肾脏替代治疗 (RRT) 或需要 RRT 的总天数没有显着差异。尽管 DCD 组缺血型胆道病变的发生率更高(发病率 [IR]:4.4 对 0 例/100 患者年;p<0.001),但总体上没有增加移植后胆道狭窄的风险(风险比 [HR]:1.20,0.58-2.46;p=0.624),或在特定于吻合口狭窄或复发性 PSC 的亚组分析中,供体类型之间。DCD 与 DBD 肝脏移植后,移植物丢失率和死亡率没有显着差异(IR:分别为 3.6 与 3.1 例/100 患者年,p=0.34;3.9 与 4.7,p=0.6;)。PSC 中的 DCD 肝移植不会增加移植物丢失的风险(HR:1.69,0.58-4.95,p=0.341)或患者死亡率(0.75,0.25-2.21,p=0.598)。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。结论 PSC 患者中 DCD(与 DBD)肝脏移植不会影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DBD) PSC 患者的肝脏不影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DBD) PSC 患者的肝脏不影响移植物丢失或患者存活。在器官短缺的时代,DCD 移植是 PSC 患者肝移植的一种可行的治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DCD 移植物代表了 PSC 患者肝移植的可行治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。DCD 移植物代表了 PSC 患者肝移植的可行治疗选择。总结:本研究通过与脑干死亡 (DBD) 后捐赠的器官相比,检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,其中器官在循环死亡 (DCD) 后捐赠。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。本研究检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,与脑干死亡 (DBD) 后捐赠的器官相比,循环死亡 (DCD) 后捐赠的器官。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。本研究检查了肝移植对原发性硬化性胆管炎 (PSC) 的影响,与脑干死亡 (DBD) 后捐赠的器官相比,循环死亡 (DCD) 后捐赠的器官。We show that in appropriately selected patients, the outcomes for DCD transplantation mirror those using DBD livers, with no significant differences in complication rate, patient survival or transplanted liver survival. 在器官短缺和等待名单时间增加的时代,DCD 肝脏代表了 PSC 移植的潜在治疗选择。











































 京公网安备 11010802027423号
京公网安备 11010802027423号