PLOS Medicine ( IF 10.5 ) Pub Date : 2017-08-08 , DOI: 10.1371/journal.pmed.1002373 Jordan E Cates 1 , Holger W Unger 2, 3 , Valerie Briand 4 , Nadine Fievet 4 , Innocent Valea 5, 6 , Halidou Tinto 5, 6 , Umberto D'Alessandro 7 , Sarah H Landis 8 , Seth Adu-Afarwuah 9 , Kathryn G Dewey 10 , Feiko O Ter Kuile 11 , Meghna Desai 12 , Stephanie Dellicour 11 , Peter Ouma 13 , Julie Gutman 12 , Martina Oneko 13 , Laurence Slutsker 14 , Dianne J Terlouw 11, 15 , Simon Kariuki 13 , John Ayisi 13 , Mwayiwawo Madanitsa 11, 16 , Victor Mwapasa 16 , Per Ashorn 17 , Kenneth Maleta 16 , Ivo Mueller 18 , Danielle Stanisic 19 , Christentze Schmiegelow 20 , John P A Lusingu 20, 21 , Anna Maria van Eijk 11 , Melissa Bauserman 22, 23 , Linda Adair 23 , Stephen R Cole 1 , Daniel Westreich 1 , Steven Meshnick 1 , Stephen Rogerson 3
|
Background
Four studies previously indicated that the effect of malaria infection during pregnancy on the risk of low birthweight (LBW; <2,500 g) may depend upon maternal nutritional status. We investigated this dependence further using a large, diverse study population.
Methods and findings
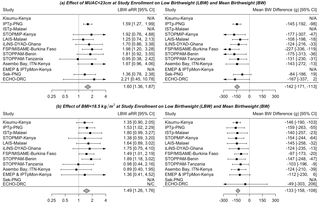
We evaluated the interaction between maternal malaria infection and maternal anthropometric status on the risk of LBW using pooled data from 14,633 pregnancies from 13 studies (6 cohort studies and 7 randomized controlled trials) conducted in Africa and the Western Pacific from 1996–2015. Studies were identified by the Maternal Malaria and Malnutrition (M3) initiative using a convenience sampling approach and were eligible for pooling given adequate ethical approval and availability of essential variables. Study-specific adjusted effect estimates were calculated using inverse probability of treatment-weighted linear and log-binomial regression models and pooled using a random-effects model. The adjusted risk of delivering a baby with LBW was 8.8% among women with malaria infection at antenatal enrollment compared to 7.7% among uninfected women (adjusted risk ratio [aRR] 1.14 [95% confidence interval (CI): 0.91, 1.42]; N = 13,613), 10.5% among women with malaria infection at delivery compared to 7.9% among uninfected women (aRR 1.32 [95% CI: 1.08, 1.62]; N = 11,826), and 15.3% among women with low mid-upper arm circumference (MUAC <23 cm) at enrollment compared to 9.5% among women with MUAC ≥ 23 cm (aRR 1.60 [95% CI: 1.36, 1.87]; N = 9,008). The risk of delivering a baby with LBW was 17.8% among women with both malaria infection and low MUAC at enrollment compared to 8.4% among uninfected women with MUAC ≥ 23 cm (joint aRR 2.13 [95% CI: 1.21, 3.73]; N = 8,152). There was no evidence of synergism (i.e., excess risk due to interaction) between malaria infection and MUAC on the multiplicative (p = 0.5) or additive scale (p = 0.9). Results were similar using body mass index (BMI) as an anthropometric indicator of nutritional status. Meta-regression results indicated that there may be multiplicative interaction between malaria infection at enrollment and low MUAC within studies conducted in Africa; however, this finding was not consistent on the additive scale, when accounting for multiple comparisons, or when using other definitions of malaria and malnutrition. The major limitations of the study included availability of only 2 cross-sectional measurements of malaria and the limited availability of ultrasound-based pregnancy dating to assess impacts on preterm birth and fetal growth in all studies.
Conclusions
Pregnant women with malnutrition and malaria infection are at increased risk of LBW compared to women with only 1 risk factor or none, but malaria and malnutrition do not act synergistically.
中文翻译:

疟疾、营养不良和出生体重:使用个体参与者数据的荟萃分析
背景
先前的四项研究表明,怀孕期间感染疟疾对低出生体重(LBW;<2,500 g)风险的影响可能取决于母亲的营养状况。我们使用大量不同的研究人群进一步调查了这种依赖性。
方法和发现
我们使用来自 1996 年至 2015 年在非洲和西太平洋地区进行的 13 项研究(6 项队列研究和 7 项随机对照试验)的 14,633 例妊娠的汇总数据,评估了孕产妇疟疾感染和孕产妇人体测量状况对 LBW 风险的相互作用。研究由孕产妇疟疾和营养不良 (M3) 倡议使用便利抽样方法确定,并且在获得足够的伦理批准和基本变量的可用性的情况下有资格合并。使用治疗加权线性和对数二项式回归模型的逆概率计算研究特定的调整效应估计值,并使用随机效应模型进行汇总。在产前登记时患有疟疾感染的女性中,经调整后分娩 LBW 婴儿的风险为 8.8%,而这一比例为 7。N = 13,613),分娩时感染疟疾的女性中为 10.5%,而未感染女性中为 7.9%(aRR 1.32 [95% CI:1.08, 1.62];N = 11,826),中上臂低位女性中为 15.3%入组时周长(MUAC <23 cm),而 MUAC ≥ 23 cm 的女性为 9.5%(aRR 1.60 [95% CI: 1.36, 1.87];N = 9,008)。入组时患有疟疾感染和低 MUAC 的女性分娩 LBW 婴儿的风险为 17.8%,而 MUAC ≥ 23 cm 的未感染女性分娩的风险为 8.4%(联合 aRR 2.13 [95% CI: 1.21, 3.73];N = 8,152)。没有证据表明疟疾感染和 MUAC 在乘法(p = 0.5)或加法量表(p= 0.9)。使用体重指数 (BMI) 作为营养状况的人体测量指标时,结果相似。元回归结果表明,在非洲进行的研究中,登记时的疟疾感染与低 MUAC 之间可能存在乘法相互作用;然而,在考虑多重比较或使用疟疾和营养不良的其他定义时,这一发现在加法量表上并不一致。该研究的主要局限性包括仅提供 2 次疟疾横断面测量值,以及在所有研究中评估对早产和胎儿生长影响的基于超声的妊娠约会的可用性有限。
结论
与只有 1 个风险因素或没有风险因素的女性相比,营养不良和疟疾感染的孕妇发生 LBW 的风险增加,但疟疾和营养不良不会协同作用。











































 京公网安备 11010802027423号
京公网安备 11010802027423号