Abstract
Background
Impulse control disorders (ICD) are a common and disrupting complication of Parkinson’s disease (PD) treatment. Although their relationship with dopaminergic activity is well studied, their brain metabolic correlates are mostly unknown.
Methods
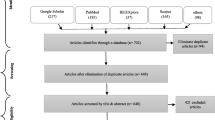
In this work we studied brain metabolism using brain 18F-FDG-PET. We performed a case-control study nested within a cohort of PD patients free of ICD at baseline to compare ICD patients right after ICD diagnosis and prior to any treatment modification with matched ICD-free patients. We also compared both PD groups with healthy controls.
Results
When compared with ICD-free PD patients, PD patients with recently diagnosed ICD showed higher glucose metabolism in widespread areas comprising prefrontal cortices, both amygdalae and default mode network hubs (p < 0.05, corrected). When compared to healthy controls, they did not show hypermetabolism, and the only hypometabolic region was the right caudate. In turn, ICD-free patients showed diffuse hypometabolism when compared to healthy controls.
Conclusion
Our results suggest brain metabolism is more preserved in PD patients with ICD than patients without ICD. This metabolic preservation could be related to ICD development.



Similar content being viewed by others
References
Maloney EM, Djamshidian A, O’Sullivan SS. Phenomenology and epidemiology of impulsive-compulsive behaviours in Parkinson’s disease, atypical Parkinsonian disorders and non-Parkinsonian populations. J Neurol Sci. 2017;374:47–52.
Berger C, Mehrhoff FW, Beier KM, Meinck H-M. Sexuelle Delinquenz und Morbus Parkinson [sexual delinquency and Parkinson’s disease]. Nervenarzt. 2003;74:370–5.
Sobrido MJ, Dias-Silva JJ, Quintáns B. Behavioral disorders in Parkinson’s disease. Genetic, pharmacological and medico-legal aspects. Rev Neurol. 2009;48(Suppl 1):S43–8.
Weintraub D, Siderowf AD, Potenza MN, Goveas J, Morales KH, Duda JE, et al. Dopamine agonist use is associated with impulse control disorders in Parkinson’s disease. Arch Neurol. 2006;63:969–73.
Weintraub D, Koester J, Potenza MN, Siderowf AD, Stacy M, Voon V, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol. 2010;67:589–95.
Bastiaens J, Dorfman BJ, Christos PJ, Nirenberg MJ. Prospective cohort study of impulse control disorders in Parkinson’s disease. Mov Disord. 2013;28:327–33.
Marinus J, Zhu K, Marras C, Aarsland D, van Hilten JJ. Risk factors for non-motor symptoms in Parkinson’s disease. Lancet Neurol. 2018;17:559–68.
Isaias IU, Siri C, Cilia R, De Gaspari D, Pezzoli G, Antonini A. The relationship between impulsivity and impulse control disorders in Parkinson’s disease. Mov Disord. 2008;23:411–5.
Marín-Lahoz J, Pagonabarraga J, Martinez-Horta S, Fernandez de Bobadilla R, Pascual-Sedano B, Pérez-Pérez J, et al. Parkinson’s Disease: Impulsivity Does Not Cause Impulse Control Disorders but Boosts Their Severity. Front Psychiatry. 2018;9:465.
Djamshidian A, O’Sullivan SS, Sanotsky Y, Sharman S, Matviyenko Y, Foltynie T, et al. Decision-making, impulsivity and addictions: do Parkinson’s disease patients jump to conclusions? Mov Disord. 2012;27:1137–45.
Joutsa J, Martikainen K, Vahlberg T, Voon V, Kaasinen V. Impulse control disorders and depression in Finnish patients with Parkinson’s disease. Parkinsonism Relat Disord. 2012;18:155–60.
Callesen MB, Weintraub D, Damholdt MF, Møller A. Impulsive and compulsive behaviors among Danish patients with Parkinson’s disease: prevalence, depression, and personality. Parkinsonism Relat Disord. 2014;20:22–6.
Eisinger RS, Ramirez-Zamora A, Carbunaru S, Ptak B, Peng-Chen Z, Okun MS, et al. Medications, Deep Brain Stimulation, and Other Factors Influencing Impulse Control Disorders in Parkinson’s Disease. Front Neurol [Internet]. 2019 [cited 2019 Mar 11];10. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2019.00086/full.
Kraemmer J, Smith K, Weintraub D, Guillemot V, Nalls MA, Cormier-Dequaire F, et al. Clinical-genetic model predicts incident impulse control disorders in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2016;87:1106–11.
Aracil-Bolaños I, Strafella AP. Molecular imaging and neural networks in impulse control disorders in Parkinson’s disease. Parkinsonism Relat Disord. 2016;22:S101–5.
Martini A, Dal Lago D, Edelstyn NMJ, Salgarello M, Lugoboni F, Tamburin S. Dopaminergic neurotransmission in patients with Parkinson’s disease and impulse control disorders: a systematic review and meta-analysis of PET and SPECT studies. Front Neurol [Internet]. 2018 [cited 2019 Mar 26];9. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2018.01018/full.
Biundo R, Formento-Dojot P, Facchini S, Vallelunga A, Ghezzo L, Foscolo L, et al. Brain volume changes in Parkinson’s disease and their relationship with cognitive and behavioural abnormalities. J Neurol Sci. 2011;310:64–9.
Pellicano C, Niccolini F, Wu K, O’Sullivan SS, Lawrence AD, Lees AJ, et al. Morphometric changes in the reward system of Parkinson’s disease patients with impulse control disorders. J Neurol. 2015;262:2653–61.
Biundo R, Weis L, Facchini S, Formento-Dojot P, Vallelunga A, Pilleri M, et al. Patterns of cortical thickness associated with impulse control disorders in Parkinson’s disease. Mov Disord. 2015;30:688–95.
Imperiale F, Agosta F, Canu E, Markovic V, Inuggi A, Jecmenica-Lukic M, et al. Brain structural and functional signatures of impulsive–compulsive behaviours in Parkinson’s disease. Mol Psychiatry. 2018;23:459–66.
Tessitore A, De Micco R, Giordano A, di Nardo F, Caiazzo G, Siciliano M, et al. Intrinsic brain connectivity predicts impulse control disorders in patients with Parkinson’s disease. Mov Disord. 2017;32:1710–9.
Tessitore A, Santangelo G, De Micco R, Giordano A, Raimo S, Amboni M, et al. Resting-state brain networks in patients with Parkinson’s disease and impulse control disorders. Cortex. 2017;94:63–72.
Verger A, Klesse E, Chawki MB, Witjas T, Azulay J-P, Eusebio A, et al. Brain PET substrate of impulse control disorders in Parkinson’s disease: a metabolic connectivity study. Hum Brain Mapp. 2018;39:3178–86.
Navalpotro-Gomez I, Dacosta-Aguayo R, Molinet-Dronda F, Martin-Bastida A, Botas-Peñin A, Jimenez-Urbieta H, et al. Nigrostriatal dopamine transporter availability, and its metabolic and clinical correlates in Parkinson’s disease patients with impulse control disorders. Eur J Nucl Med Mol Imaging. 2019;46:2065–76.
Vriend C, Nordbeck AH, Booij J, van der Werf YD, Pattij T, Voorn P, et al. Reduced dopamine transporter binding predates impulse control disorders in Parkinson’s disease: reduced DaT BR predates ICD in PD. Mov Disord. 2014;29:904–11.
Berti V, Mosconi L, Pupi A. Brain: normal variations and benign findings in FDG PET/CT imaging. PET Clin. 2014;9:129–40.
Hirano S, Asanuma K, Ma Y, Tang C, Feigin A, Dhawan V, et al. Dissociation of metabolic and neurovascular responses to levodopa in the treatment of Parkinson’s disease. J Neurosci. 2008;28:4201–9.
Mah L, Zarate CA, Nugent AC, Singh JB, Manji HK, Drevets WC. Neural mechanisms of antidepressant efficacy of the dopamine receptor agonist pramipexole in treatment of bipolar depression. Int J Neuropsychopharmacol. 2011;14:545–51.
Kim E, Howes OD, Turkheimer FE, Kim B-H, Jeong JM, Kim JW, et al. The relationship between antipsychotic D2 occupancy and change in frontal metabolism and working memory : a dual [(11)C] raclopride and [(18) F] FDG imaging study with aripiprazole. Psychopharmacology. 2013;227:221–9.
Ko JH, Lerner RP, Eidelberg D. Effects of levodopa on regional cerebral metabolism and blood flow. Mov Disord. 2015;30:54–63.
Yakushev I, Drzezga A, Habeck C. Metabolic connectivity: methods and applications. Curr Opin Neurol. 2017;30:677–85.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease: MDS-PD Clinical Diagnostic Criteria. Mov Disord. 2015;30:1591–601.
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007;22:1689–707 quiz 1837.
Weintraub D, Hoops S, Shea JA, Lyons KE, Pahwa R, Driver-Dunckley ED, et al. Validation of the questionnaire for impulsive-compulsive disorders in Parkinson’s disease. Mov Disord. 2009;24:1461–7.
Brown RIF. Some contributions of the study of gambling to the study of other addictions. In: Eadington WR, Cornelius JA, editors. Gambling behavior and problem gambling. 1st ed. Reno: Univ of Nevada Pr; 1993.
Griffiths M. A ‘components’ model of addiction within a biopsychosocial framework. J Subst Abus. 2005;10:191–7.
Weintraub D, Mamikonyan E, Papay K, Shea JA, Xie SX, Siderowf A. Questionnaire for impulsive-compulsive disorders in Parkinson’s disease-rating scale. Mov Disord. 2012;27:242–7.
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23:2129–70.
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord. 2010;25:2649–53.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Marinus J, Leentjens AF, Visser M, Stiggelbout AM, van Hilten JJ. Evaluation of the hospital anxiety and depression scale in patients with Parkinson’s disease. Clin Neuropharmacol. 2002;25:318–24.
Starkstein SE, Mayberg HS, Preziosi TJ, Andrezejewski P, Leiguarda R, Robinson RG. Reliability, validity, and clinical correlates of apathy in Parkinson’s disease. J Neuropsychiatry Clin Neurosci. 1992;4:134–9.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74.
Pagonabarraga J, Kulisevsky J, Llebaria G, García-Sánchez C, Pascual-Sedano B, Gironell A. Parkinson’s disease-cognitive rating scale: a new cognitive scale specific for Parkinson’s disease. Mov Disord. 2008;23:998–1005.
de Bobadilla RF, Pagonabarraga J, Martínez-Horta S, Pascual-Sedano B, Campolongo A, Kulisevsky J. Parkinson’s disease-cognitive rating scale: Psychometrics for mild cognitive impairment. Mov Disord. 2013;28:1376–83.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Någren K, et al. EANM procedure guidelines for PET brain imaging using [18F] FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10.
Martínez-Horta S, Moreu A, Perez-Perez J, Sampedro F, Horta-Barba A, Pagonabarraga J, et al. The impact of bilingualism on brain structure and function in Huntington’s disease. Parkinsonism Relat Disord. 2019;60:92–7.
Chen J, Swope D, Dashtipour K. Comprehensive review of rasagiline, a second-generation monoamine oxidase inhibitor, for the treatment of Parkinson’s disease. Clin Ther. 2007;29:1825–49.
Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci U S A. 2000;97:11050–5.
Greve DN, Svarer C, Fisher PM, Feng L, Hansen AE, Baare W, et al. Cortical surface-based analysis reduces bias and variance in kinetic modeling of brain PET data. Neuroimage. 2014;92:225–36.
Greve DN, Salat DH, Bowen SL, Izquierdo-Garcia D, Schultz AP, Catana C, et al. Different partial volume correction methods lead to different conclusions: an (18)F-FDG-PET study of aging. Neuroimage. 2016;132:334–43.
Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE. Permutation inference for the general linear model. Neuroimage. 2014;92:381–97.
Rao H, Mamikonyan E, Detre JA, Siderowf AD, Stern MB, Potenza MN, et al. Decreased ventral striatal activity with impulse control disorders in Parkinson’s disease. Mov Disord. 2010;25:1660–9.
Balodis IM, Kober H, Worhunsky PD, Stevens MC, Pearlson GD, Potenza MN. Diminished fronto-striatal activity during processing of monetary rewards and losses in pathological gambling. Biol Psychiatry. 2012;71:749–57.
Sampedro F, Vilaplana E, de Leon MJ, Alcolea D, Pegueroles J, Montal V, et al. APOE-by-sex interactions on brain structure and metabolism in healthy elderly controls. Oncotarget [Internet]. 2015 [cited 2019 Nov 26];6. Available from: http://www.oncotarget.com/fulltext/5185.
Riba J, Krämer UM, Heldmann M, Richter S, Münte TF. Dopamine agonist increases risk taking but blunts reward-related brain activity. PLoS One [Internet]. 2008 [cited 2019 Mar 11];3. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2423613/.
Ye Z, Hammer A, Camara E, Münte TF. Pramipexole modulates the neural network of reward anticipation. Hum Brain Mapp. 2011;32:800–11.
Dragogna F, Mauri MC, Marotta G, Armao FT, Brambilla P, Altamura AC. Brain metabolism in substance-induced psychosis and schizophrenia: a preliminary PET study. Neuropsychobiology. 2014;70:195–202.
Siri C, Cilia R, Reali E, Pozzi B, Cereda E, Colombo A, et al. Long-term cognitive follow-up of Parkinson’s disease patients with impulse control disorders. Mov Disord. 2015;30:696–704.
Martini A, Dal Lago D, Edelstyn NMJ, Grange JA, Tamburin S. Impulse control disorder in Parkinson’s disease: a meta-analysis of cognitive, affective, and motivational correlates. Front Neurol [Internet]. 2018 [cited 2019 Jun 4];9. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2018.00654/full#h10.
Schindlbeck KA, Eidelberg D. Network imaging biomarkers: insights and clinical applications in Parkinson’s disease. Lancet Neurol. 2018;17:629–40.
Pagonabarraga J, Kulisevsky J. Cognitive impairment and dementia in Parkinson’s disease. Neurobiol Dis. 2012;46:590–6.
Sampedro F, Marín-Lahoz J, Martínez-Horta S, Pagonabarraga J, Kulisevsky J. Dopaminergic degeneration induces early posterior cortical thinning in Parkinson’s disease. Neurobiol Dis. 2019;124:29–35.
Firbank MJ, Yarnall AJ, Lawson RA, Duncan GW, Khoo TK, Petrides GS, et al. Cerebral glucose metabolism and cognition in newly diagnosed Parkinson’s disease: ICICLE-PD study. J Neurol Neurosurg Psychiatry. 2017;88:310–6.
Tan H, Li X, Wei K, Guan Y. Study on brain glucose metabolic networks in Parkinson’s disease patients with visual spatial dysfunction by 18F-FDG PET imaging. Tradit Med Mod Med. 2018;01:27–31.
Matthews DC, Lerman H, Lukic A, Andrews RD, Mirelman A, Wernick MN, et al. FDG PET Parkinson’s disease-related pattern as a biomarker for clinical trials in early stage disease. NeuroImage Clin. 2018;20:572–9.
Martinez-Horta S, Sampedro F, Pagonabarraga J, Fernandez-Bobadilla R, Marin-Lahoz J, Riba J, et al. Non-demented Parkinson’s disease patients with apathy show decreased grey matter volume in key executive and reward-related nodes. Brain Imaging Behav. 2017;11:1334–42.
Dujardin K, Sockeel P, Delliaux M, Destée A, Defebvre L. Apathy may herald cognitive decline and dementia in Parkinson’s disease. Mov Disord. 2009;24:2391–7.
Martínez-Horta S, Riba J, de Bobadilla RF, Pagonabarraga J, Pascual-Sedano B, Antonijoan RM, et al. Apathy in Parkinson’s disease: neurophysiological evidence of impaired incentive processing. J Neurosci. 2014;34:5918–26.
Leroi I, Andrews M, McDonald K, Harbishettar V, Elliott R, Byrne EJ, et al. Apathy and impulse control disorders in Parkinson’s disease: a direct comparison. Parkinsonism Relat Disord. 2012;18:198–203.
Delrieu J, Desmidt T, Camus V, Sourdet S, Boutoleau-Bretonnière C, Mullin E, et al. Apathy as a feature of prodromal Alzheimer’s disease: an FDG-PET ADNI study. Int J Geriatr Psychiatry. 2015;30:470–7.
Gatchel JR, Donovan NJ, Locascio JJ, Becker JA, Rentz DM, Sperling RA, et al. Regional 18F-Fluorodeoxyglucose hypometabolism is associated with higher apathy scores over time in early Alzheimer disease. Am J Geriatr Psychiatry. 2017;25:683–93.
Martínez-Horta S, Perez-Perez J, Sampedro F, Pagonabarraga J, Horta-Barba A, Carceller-Sindreu M, et al. Structural and metabolic brain correlates of apathy in Huntington’s disease. Mov Disord. 2018;33:1151–9.
Funding
This work was financially supported by CIBERNED and grants from la Marató de TV3 (2014/U/477 and 20142910) and Fondo de Investigaciones Sanitarias del Ministerio de Sanidad y Consumo (PI15/00962). None of the supporting organizations played a direct role on the inception, development, or publication of this work.
Author information
Authors and Affiliations
Contributions
Study design: JML, JK, SMH, IC.
Study execution: JML, AHB, SMH, IAB, MC, JP, HBM.
Image analysis: FS.
Statistical analysis: FS, JML.
First draft: JML, FS.
Manuscript review: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurology.
Electronic supplementary material
ESM 1
(DOCX 3200 kb)
Rights and permissions
About this article
Cite this article
Marín-Lahoz, J., Sampedro, F., Horta-Barba, A. et al. Preservation of brain metabolism in recently diagnosed Parkinson’s impulse control disorders. Eur J Nucl Med Mol Imaging 47, 2165–2174 (2020). https://doi.org/10.1007/s00259-019-04664-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04664-2