Abstract
Background
Type IV renal tubular acidosis (RTA) is a severe complication of urinary tract infection (UTI) in infants. A detailed clinical and molecular analysis is still lacking.
Methods
Infants with UTI who exhibited features of type IV RTA were prospectively enrolled. Clinical, laboratory, and image characteristics and sequencing of genes responsible for phenotype were determined with follow-up.
Results
The study cohort included 12 infants (9 males, age 1–8 months). All exhibited typical type IV RTA such as hyperkalemia with low transtubular potassium gradient, hyperchloremic metabolic acidosis with positive urine anion gap, hypovolemic hyponatremia with renal salt wasting, and high plasma renin and aldosterone levels. Seven had hyperkalemia-related arrhythmia and two of them developed life-threatening ventricular tachycardia. With prompt therapy, all clinical and biochemical abnormalities resolved within 1 week. Five had normal urinary tract anatomy, and three of them carried genetic variants on NR3C2. Three variants, c.1645T>G (S549A), c.538G>A (V180I), and c.1-2C>G, on NR3C2 were identified in four patients. During follow-up, none of them had recurrent type IV RTA, but four developed renal scaring.
Conclusions
Genetic mutation on NR3C2 may contribute to the development of type IV RTA as a complication of UTI in infants without identifiable risk factors, such as urinary tract anomalies.
Similar content being viewed by others
Introduction
Renal tubular acidosis (RTA) is traditionally classified into three forms: distal RTA (type I), proximal RTA (type II), and hyperkalemic RTA (type IV). Unlike type I and type II RTA that presents commonly with hypokalemia, type IV RTA is characterized by hyponatremia, hyperkalemia, and non-anion gap metabolic acidosis associated with reduced distal hydrogen secretion. The etiologies of type IV RTA are diverse, including inherited mutations in genes encoding mineralocorticoid receptor (MR) and renal epithelial sodium channel (ENaC) or acquired disorders, such as tubulointerstitial nephritis, lupus nephritis, and chronic kidney disease. Its course can be permanent or transient in nature. Type IV RTA has been also reported as a severe complication of urinary tract infection (UTI). Although the clinical features of type IV RTA in infants with UTI are usually non-specific and asymptomatic, cases with life-threating hyperkalemia have been reported.1 Therefore, type IV RTA should not be considered as a benign complication of UTI. A comprehensive analysis of clinical outcomes in infants with UTI complicated by type IV RTA remains lacking.
Young age and urinary tract anomalies have been identified as two important factors for the development of type IV RTA in cases with UTI.1,2,3,4,5 Nevertheless, many do not exhibit the known structure anomalies.6,7,8 Recently, a pathogenic mutation on NR3C2 has been identified in an infant with UTI complicated by type IV RTA, which suggests the possible overlap between primary and secondary type IV RTA.9 To date, the genetic sequencing of ENaC and MR has not been fully evaluated in these infants. The aim of this study was to investigate clinical features, genetic background, and outcome in infants with UTI and type IV RTA.
Materials and methods
Subjects and diagnosis of type IV RTA
The study protocol was approved by the Ethics Committee on Human Studies at Chang Gung Memorial Hospital in Taiwan, R.O.C. (IRB 00481A3). Informed consent was obtained from the parents after a detailed description of the study. Infants with UTI admitted to Chang Gung Memorial Hospital were prospectively enrolled from January 2015 to December 2018. Laboratory tests, which includes serum creatinine, Na+, K+, Cl−, HCO3−, osmolality, plasma aldosterone and renin, and urine creatinine, were measured at presentation and followed up during hospitalization. The diagnosis of type IV RTA included the findings of hyperkalemia (serum K+ >6.0 mmol/L) with impaired renal K+ excretion, non-anion gap metabolic acidosis (anion gap <12 with [HCO3−] < 22 mmol/L) with positive urine anion gap (low urine ammonium excretion), relatively low urine pH (<6.0), and normal renal function. To exclude the other causes of type IV RTA such as obstructive nephropathy, diabetic nephropathy, etc., patients who had hyporeninemia or hypoaldosteronism were excluded. As shown in Fig. 1, patients who had (1) impaired renal function defined as chronic kidney disease stage III–V, (2) pre-existing electrolyte imbalance, (3) pharmacological history that may cause type IV RTA, (4) lack of DNA for analysis, (5) no imaging studies, and (6) lost to follow-up were excluded. Finally, 12 infants with UTI who exhibited features of type IV RTA were enrolled. UTI was defined by a positive urine culture with at least 100,000 colony-forming units per mL of a single urinary tract pathogen from a specimen obtained by catheter or urine bag or any pathogen from a suprapubic puncture.
Image studies
Technetium-99m-dimercaptosuccinic acid (DMSA) renal scanning and voiding cystourethrography (VCUG) were performed following the diagnosis of UTI. Acute pyelonephritis and renal scar detected by Technetium-99m-DMSA were defined according to a previous study.11 Grading of vesicoureteral reflux (VUR) was based on the criteria previously proposed by International Reflux Study in Children.12 An experienced nuclear medicine consultant and an experienced radiologist blinded to the patients’ clinical condition interpreted the DMSA and VCUG studies, respectively.
Clinical characteristics, treatment, and outcome
Patient demographics and clinical features, treatment, and outcome data were collected in all patients. The clinical features consisted of gender, age at onset, underlying disease, symptoms at presentation. Clinical outcomes, including arrhythmia, unstable hemodynamics, renal scar, and sequelae of vital organs, were determined at follow-up.
Molecular analysis
Genomic DNA was extracted from peripheral leukocyte with DNA isolation kits (QIAamp Blood Kit; Qiagen, Dusseldorf, Germany). We sequenced the complete coding regions and intron–exon junctions of the NR3C2, SCNN1A, SCNN1B, and SCNN1G genes. The identified mutations were predicted by using eight pathogenicity computation score that was calculated using PolyPhen2, MutationTaster, Mutation Assessor, FATHMM, M-CAP, CADD, DANN, and GERP++. Score 8 from all of pathogenicity computation is a pathogenic mutation.
Results
Demographic and clinical manifestations
The overall incidence of type IV RTA in infants with UTI was around 0.57% (29/512) in this study. There were 9 males and 3 females, who presented at mean age 2.6 ± 1.2 months (ranging from 1 to 8 months). Three-fourths (75%) of patients had disease onset at <3 months of age. As shown in Table 1, poor oral feeding and vomiting were the most common symptoms at presentation. The duration from the onset of UTI to the diagnosis of type IV RTA ranged from 1 to 5 days. Of note, half of them developed type IV RTA after resolution of fever.
Laboratory characteristics
All patients manifested moderate-to-severe hyperkalemia (K+ 6.4 ± 0.2 mmol/L) with inappropriately low renal K+ excretion (transtubular potassium gradient 3.3 ± 0.5), non-anion gap metabolic acidosis (HCO3− 15.1 ± 1.5 mmol/L), and positive urine anion gap (14.2 ± 5.6 mEq/L). They also had hypovolemic hyponatremia (Na+ 125.3 ± 3.3 mmol/L) with renal Na+ wasting (fractional excretion of sodium 2.4 ± 0.2 %) and inappropriately high plasma renin (476.2 ± 295.2 pg/mL) and aldosterone levels (869.8 ± 280.3 pg/mL) (Table 1), excluding the hyporeninemia or hypoaldosteronism causes for type IV RTA. The serum creatinine levels ranged from 0.18 to 0.30 mg/dL. There were no leukocytosis, thrombocytosis, or traumatic blood sampling. The most common pathogens cultured from the urine are Escherichia coli followed by Enterococcus spp. and Klebsiella pneumoniae.
Molecular analysis of corresponding genes
Sanger sequence of NR3C2, SCNN1A, SNN1B, and SCNN1G were conducted in all patients. Three genetic variants, c.1-2C>G (slicing site), c.538G>A, and c.1645T>G, on NR3C2 were detected in four patients (Table 2). The genetic variant c.1645T>G, but not c.1-2C>G or c.538G>A, was predicted to be pathogenic by in silico analysis. This novel and heterozygous thymine-to-guanine substitution at position 1645 (c.1645T>G) in exon 2 resulted in amino acid substitution of serine for alanine (S549A) in patient 9. This specific genetic variant was not found in 200 healthy subjects and was inherited from his father (Fig. 2).
Kidney and urinary tract anomalies
Nine patients had pyelonephritis diagnosed by DMSA renal scan, and two of them had bilateral pyelonephritis (Table 2). Urinary tract anomalies, including VUR, ureteropelvic junction obstruction, ectopic ureter, and unilateral renal agenesis, were identified in seven patients. Of note, VUR was the most common anomaly. Seven patients had both pyelonephritis and urinary tract anomalies. Five patients did not have urinary tract anomalies and one of them (patient 9) harbored hoterozygous mutation on NR3C2 gene.
Complications, treatment, and follow-up outcome
Seven patients exhibited arrhythmia with predominant tented T wave and two of them developed ventricular tachycardia (Table 2) requiring intravenous calcium and insulin administration. Intravenous antibiotics, salt and fluid hydration, and furosemide were administered to all patients for the treatment of the underlying UTI, hyponatremia, and hyperkalemia, respectively. Four patients received NaHCO3 supplement for severe metabolic acidosis. All patients achieved full recovery with resolution of type IV RTA within the first week of hospitalization. Prolonged hospital stay was noted in one patient (patient 6) due to complications from seizure and aspiration pneumonia. During their 6-month follow-up, four patients had renal scar detected by DMSA renal scan. None of the patients had recurrence of type IV RTA. Patient 9 who harbored genetic defect on NR3C2 had a normal high serum K+ (5.2 mmol/L) at the age of 1 year during follow-up.
Discussion
In this study, we found that nearly half of the patients with UTI-associated type IV RTA did not have urinary tract anomalies. Over half of the patients developed arrhythmia, and two patients had ventricular tachycardia. All patients had full resolution of type IV RTA within 1 week after treatment and did not have recurrence during follow-up. In the investigation of genetic background of these infants, we identified one novel missense mutation at the phosphorylation site of NR3C2.
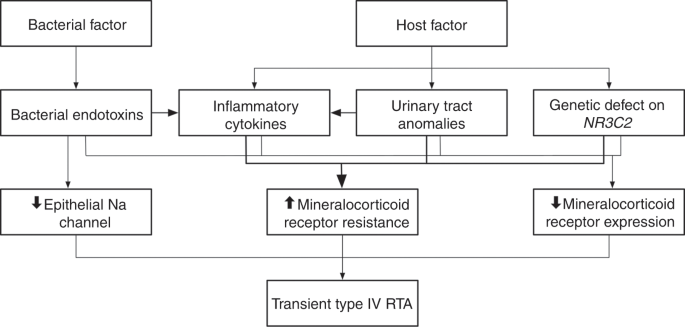
The cardinal presentations for UTI in this cohort, such as vomiting and poor oral feeding, were non-specific, thus increasing the difficulty of diagnosing type IV RTA correctly and promptly without measurement of blood electrolytes and acid–base status. Previous studies have pointed out that young age is a necessary factor for the development of UTI-associated type IV RTA. All our patients were aged <8 months. The relatively immature renal tubules in infants have limited compensatory capacity, resulting from both/either physiological partial aldosterone resistance and/or low renal MR expression associated with UTIs.6,10,13,14,15 Similar to the previous reports, we found that VUR was the leading anomaly of urinary tract in our patients with UTI-associated type IV RTA.6 Urinary tract anomaly is also shown to be associated with the decreased expression of MR receptor and increased MR resistance.16,17 However, the percentage of urinary tract anomalies in this study was approximately 60% (7/12), which was less than that previously reported (90%).6 Furthermore, recent studies reveal that bacterial endotoxins and inflammatory cytokines, such as transforming growth factor-β, interferon-α, interleukin (IL)-1, and IL-6, were involved in the pathogenesis of transient type IV RTA in infants with UTI.16,17,18,19,20,21 Accordingly, both bacterial and host factors may predispose the development of UTI-associated type IV RTA.
Three genetic variants, c.1-2C>G (slicing site), c.538G>A, and c.1645T>G, on NR3C2 encoding the MR were identified in four patients. The c.1-2C>G and c.538G>A genetic variants were predicted as benign. However, c.538G>A (V180I) has been reported to cause defective MR function in in–vitro functional study.22,23 It remains to be determined whether UTI alone or a combination of genetic defect and UTI was responsible for the development of transient type IV RTA in infants with UTI carrying this mutation.9,20 A novel and heterozygous mutation, S549A, was identified at a phosphorylation site for MR in patient 9, who had no urinary tract anomalies. The mutation was found in the father, which is consistent with the diagnosis of autosomal-dominant pseudohypoaldosteronism type I affecting the MR. Based on the absence of this variant in 200 healthy subjects and predictions from different mutation softwares, we believe this mutation to be pathogenic. A functional study is still warranted to confirm the pathogenicity of the phosphorylation site mutant S549A on MR. In summary, we proposed that bacterial factor (endotoxins) and/or host factors (inflammatory cytokines, urinary tract anomalies, genetic background) can contribute to the development of UTI-associated type IV RTA (Fig. 3).
Although the outcome of UTI-associated type IV RTA is usually favorable, some patients may present with life-threatening hyperkalemia and severe metabolic acidosis.10,24,25,26 Half of our patients developed hyperkalemia-related arrhythmia and two of them presented with ventricular arrhythmia requiring emergent management. Early recognition and timely treatment to normalize electrolyte status is crucial to avoid the complications of transient type IV RTA in infants with UTI. Furthermore, we emphasize that any form of stress, especially infections in infancy not limited to UTI, could trigger the clinical manifestations of type IV RTA in infants harboring the genetic defect in NR3C2. Close monitoring of recurrence of type IV RTA should be considered in these infants during their acute illness.
Conclusion
Although UTI-associated type IV RTA is usually transient with a benign outcome, rapid-onset and life-threatening complications such as hyperkalemia-related arrhythmia and severe metabolic acidosis can occur and require emergent therapy. Aside from young age and urinary tract anomalies, underlying genetic defects on NR3C2 could be a contributing factor for UTI-associated type IV RTA without other identifiable risk factors.
References
Rodríguez-Soriano, J., Vallo, A., Oliveros, R. & Castillo, G. Transient pseudohypoaldosteronism secondary to obstructive uropathy in infancy. J. Pediatr. 103, 375–380 (1983).
Levin, T. L. et al. Salt losing nephropathy simulating congenital adrenal hyperplasia in infants with obstructive uropathy and/or vesicoureteral reflux–value of ultrasonography in diagnosis. Pediatr. Radiol. 21, 413–415 (1991).
Perez-Brayfield, M. R., Gatti, J., Smith, E. & Kirsch, A. J. Pseudohypoaldosteronism associated with ureterocele and upper pole moiety obstruction. Urology 57, 1178 (2001).
Schoen, E. J., Bhatia, S., Ray, G. T., Clapp, W. & To, T. T. Transient pseudohypoaldosteronism with hyponatremia-hyperkalemia in infant urinary tract infection. J. Urol. 167, 680–682 (2002).
Watanabe, T. Reversible secondary pseudohypoaldosteronism. Pediatr. Nephrol. 18, 486 (2003).
Bogdanović, R., Stajić, N., Putnik, J. & Paripović, A. Transient type 1 pseudo-hypoaldosteronism: report on an eight-patient series and literature review. Pediatr. Nephrol. 24, 2167–2175 (2009).
Gerigk, M., Glanzmann, R., Rascer, W. & Gnehm, H. E. Hyponatraemia and hyperkalaemia in acute pyelonephritis without urinary tract anomalies. Eur. J. Pediatr. 154, 582–584 (1995).
Kashimada, K., Omori, T., Takizawa, F. & Mizutani, S. Two cases of transient pseudohypoaldosteronism due to group B Streptococcus pyelonephritis. Pediatr. Nephrol. 23, 1569–1570 (2008).
Bowden, S. A. et al. Autosomal dominant pseudohypoaldosteronism type 1 in an infant with salt wasting crisis associated with urinary tract infection and obstructive uropathy. Case Rep. Endocrinol. 2013, 524647 (2013).
Melzi, M. L. et al. Acute pyelonephritis as a cause of hyponatremia/hyperkalemia in young infants with urinary tract malformations. Pediatr. Infect. Dis. J. 114, 56–59 (1995).
Patel, K., Charron, M., Hoberman, A., Brown, M. L. & Rogers, K. D. Intra- and interobserver variability in interpretation of DMSA scans using a set of standardized criteria. Pediatr. Radiol. 23, 506–509 (1993).
Lebowitz, R. L., Olbing, H., Parkkulainen, K. V., Smellie, J. M. & Tamminen-Möbius, T. E. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr. Radiol. 115, 105–109 (1985).
Al-Dahhan, J., Haycock, G. B., Chantler, C. & Stimmler, L. Sodium homeostasis in term and preterm neonates. I. Renal aspects. Arch. Dis. Child. 58, 335–342 (1983).
Martinerie, L. et al. Physiological partial aldosterone resistance in human newborns. Pediatr. Radiol. 66, 323–328 (2009).
Martinerie, L. et al. Low renal mineralocorticoid receptor expression at birth contributes to partial aldosterone resistance in neonates. Endocrinology 150, 4414–4424 (2009).
Klahr, S. Obstructive nephropathy. Intern. Med. 39, 3553–3561 (2000).
Rugo, H. S., O'Hanley, P. & Bishop, A. G. Local cytokine production in a murine model of Escherichia coli pyelonephritis. J. Clin. Invest. 89, 1032–1039 (1992).
Husted, R. F., Matsushita, K. & Stokes, J. B. Induction of resistance to mineralocorticoid hormone in cultured inner medullary collecting duct cells by TGF-beta 1. Am. J. Physiol. 267, F767–F775 (1994).
Caverzasio, J., Rizzoli, R., Dayer, J. M. & Bonjour, J. P. Interleukin-1 decreases renal sodium reabsorption: possible mechanism of endotoxin-induced natriuresis. Am. J. Physiol. 252, F943–F946 (1987).
Bayer, M. & Kutílek, S. A hereditary form of pseudohypoaldosteronism may be manifested in the course of pyelonephritis. Acta Paediatr. 82, 504 (1993).
De Seigneux, S., Leroy, V. & Ghzili, H. NF-kappaB inhibits sodium transport via down-regulation of SGK1 in renal collecting duct principal cells. J. Biol. Chem. 283, 25671–25681 (2008).
Jeong, H. A., Park, Y. K. & Jung, Y. S. Pseudohypoaldosteronism in a newborn male with functional polymorphisms in the mineralocorticoid receptor genes. Ann. Pediatr. Endocrinol. Metab. 20, 230–234 (2015).
Viengchareun, S. et al. The mineralocorticoid receptor: insights into its molecular and (patho)physiological biology. Nucl. Recept. Signal. 5, e012–e027 (2007).
Geller, D. S., Zhang, J. & Zennaro, M. C. Autosomal dominant pseudohypoaldosteronism type 1: mechanisms, evidence for neonatal lethality, and phenotypic expression in adults. J. Am. Soc. Nephrol. 17, 1429–1436 (2006).
Thies, K. C. et al. Ventricular flutter in a neonate–severe electrolyte imbalance caused by urinary tract infection in the presence of urinary tract malformation. J. Emerg. Med. 18, 47–50 (2000).
Mastrandrea, L. D., Martin, D. J. & Springate, J. E. Clinical and biochemical similarities between reflux/obstructive uropathy and salt-wasting congenital adrenal hyperplasia. Clin. Pediatr. 44, 809–812 (2005).
Acknowledgements
This study was supported in part by research fund of Chang Gung Memorial Hospital (CMRPG3H0361, CMRPG3H0911, CMRPG3I0021), the Ministry of Science and Technology (MOST 106-2314-B-182A-123-MY3), and the Research Fund of Tri-Service General Hospital (TSGH-C106-110, TSGH-C108-132). We thank Professor Martin Konrad for critical review of the revised manuscript and Professor Yu-Ching Chou for the critical help of statistical analysis.
Author information
Authors and Affiliations
Contributions
M.-H.T. and S.-H.L. interpreted the data analyses and reviewed and revised the manuscript. J.-L.H., S.-M.H., and J.-D.T. carried out the data analysis, assisted with interpretation of the data analyses, and reviewed and revised the manuscript for important intellectual content. T.-W.W. assisted with acquisition of the data, interpreted the data analyses, and reviewed and revised the manuscript for important intellectual content. W.-L.F. and J.-J.D. conceptualized and designed the study, assisted with acquisition of data, and provided analysis and interpretation of the data. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tseng, MH., Huang, JL., Huang, SM. et al. Clinical features, genetic background, and outcome in infants with urinary tract infection and type IV renal tubular acidosis. Pediatr Res 87, 1251–1255 (2020). https://doi.org/10.1038/s41390-019-0727-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0727-7
This article is cited by
-
Pseudo-hypoaldosteronism secondary to infantile urinary tract infections: role of ultrasound
Italian Journal of Pediatrics (2022)
-
Aldosterone signaling defect in young infants: single-center report and review
BMC Endocrine Disorders (2021)