Abstract
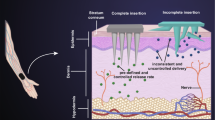
Recently, layered structures composed of nanofibers have gained attention as a novel material to mimic skin tissue in wound healing applications. The aim of this study is to develop a novel hybrid bilayer material composed of zein based composite film and nanofiber layers as a wound dressing material. The upper layer was composed of H. perforatum oil incorporated zein film including MMT and the bottom layer was comprised of 3D electrospun zein/MMT nanofibers to induce wound healing with the controlled release of H. perforatum oil. The bilayer composites were characterized in terms of mechanical test, WVP, water uptake and surface wettability. Antimicrobial activity of the wound dressings against microorganisms were investigated by disc diffusion method. In vitro cytotoxicity of monolayer film and bilayer structure was performed using WST-1 assay on HS2 keratinocyte and 3T3 cell lines. Results indicated that the prepared monolayer films showed appropriate mechanical and gas barrier properties and surface wettability for wound healing. Controlled release of H. perforatum oil was obtained from fabricated membranes up to 48 h. Bilayer membranes showed antimicrobial activity against E. coli, S. aureus, and C. albicans and did not show any toxic effect on NIH3T3 mouse fibroblast and HS2 keratinocyte cell lines. In vitro scratch assay results indicated that H. perforatum oil had a wound healing effect by inducing fibroblast migration. The proliferation study supported these results by increasing fibroblast proliferation on H. perforatum oil loaded bilayer membranes.












Similar content being viewed by others
References
Boateng JS, Mathews KH, Stevens HN, Eccleston GM. et al. Wound healing dressings and drug delivery systems: A review. J Pharm Sci. 2008;97:2892–923. https://doi.org/10.1002/jps.
Dias AMA, Braga MEM, Seabra IJ. et al. Development of natural-based wound dressings impregnated with bioactive compounds and using supercritical carbon dioxide. Int J Pharm. 2011;408:9–19. https://doi.org/10.1016/j.ijpharm.2011.01.063.
Mogoşanu GD, Grumezescu AM. Natural and synthetic polymers for wounds and burns dressing. Int J Pharm. 2014;463:127–36. https://doi.org/10.1016/j.ijpharm.2013.12.015.
Chen S, Liu B, Carlson MA, et al. Recent advances in electrospun nanofibers for wound healing. Nanomedicine. 2017;12:1335–52. https://doi.org/10.2217/nnm-2017-0017.
Venugopal J, Ramakrishna S. Biocompatible nanofiber matrices for the engineering of a dermal substitute for skin regeneration. Tissue Eng. 2005;11:847–54. https://doi.org/10.1089/ten.2005.11.847.
Figueira DR, Miguel SP, de Sá KD, Correia IJ. Production and characterization of polycaprolactone-hyaluronic acid/chitosan-zein electrospun bilayer nanofibrous membrane for tissue regeneration. Int J Biol Macromol. 2016;93:1100–10. https://doi.org/10.1016/j.ijbiomac.2016.09.080.
Hassiba A, El Zowalaty M, Webster T, et al. Synthesis, characterization, and antimicrobial properties of novel double layer nanocomposite electrospun fibers for wound dressing applications. Int J Nanomed. 2017;12:2205–13. https://doi.org/10.2147/IJN.S123417.
Corradini E, Curti PS, Meniqueti AB, et al. Recent advances in food-packing, pharmaceutical and biomedical applications of zein and zein-based materials. Int J Mol Sci. 2014;15:22438–470. https://doi.org/10.3390/ijms151222438.
Salerno A, Zeppetelli S, Oliviero M, et al. Microstructure, degradation and in vitro MG63 cells interactions of a new poly(-caprolactone), zein, and hydroxyapatite composite for bone tissue engineering. J Bioact Compat Polym. 2012;27:210–26. https://doi.org/10.1177/0883911512442564.
Luo Y, Wang Q. Zein-based micro- and nano-particles for drug and nutrient delivery: a review. J Appl Polym Sci. 2014;131:1–12. https://doi.org/10.1002/app.40696.
Paliwal R, Palakurthi S. Zein in controlled drug delivery and tissue engineering. J Control Release. 2014;189:108–22. https://doi.org/10.1016/j.jconrel.2014.06.036.
Patel AR, Velikov KP. Zein as a source of functional colloidal nano- and microstructures. Curr Opin Colloid Interface Sci. 2014;19:450–8. https://doi.org/10.1016/j.cocis.2014.08.001.
Park JH, Park SM, Kim YH, et al. Effect of montmorillonite on wettability and microstructure properties of zein/montmorillonite nanocomposite nanofiber mats. J Compos Mater. 2012;47:251–7. https://doi.org/10.1177/0021998312439221.
Alcantara ACS, Darder M, Aranda P, Ruiz-Hitzky E. Zein-fibrous clays biohybrid materials. Eur J Inorg Chem. 2012:5216–24. https://doi.org/10.1002/ejic.201200582.
Calabrese I, Gelardi G, Merli M, et al. Clay-biosurfactant materials as functional drug delivery systems: slowing down effect in the in vitro release of cinnamic acid. Appl Clay Sci. 2017;135:567–74. https://doi.org/10.1016/j.clay.2016.10.039.
Lal S, Perwez A, Rizvi MA, Datta M. Design and development of a biocompatible montmorillonite PLGA nanocomposites to evaluate in vitro oral delivery of insulin. Appl Clay Sci. 2017;147:69–79. https://doi.org/10.1016/j.clay.2017.06.031.
Ul-Islam M, Khan T, Khattak WA, Park JK. Bacterial cellulose-MMTs nanoreinforced composite films: novel wound dressing material with antibacterial properties. Cellulose. 2013;20:589–96. https://doi.org/10.1007/s10570-012-9849-3.
Saddiqe Z, Naeem I, Maimoona A. A review of the antibacterial activity of Hypericum perforatum L. J Ethnopharmacol. 2010;131:511–21. https://doi.org/10.1016/j.jep.2010.07.034.
Süntar IP, Akkol EK, Yilmazer D, et al. Investigations on the in vivo wound healing potential of Hypericum perforatum L. J Ethnopharmacol. 2010;127:468–77. https://doi.org/10.1016/j.jep.2009.10.011.
Dikmen M, Öztürk Y, Sagratini G, et al. Evaluation of the wound healing potentials of two subspecies of hypericum perforatum on cultured NIH3T3 fibroblasts. Phyther Res. 2011;25:208–14. https://doi.org/10.1002/ptr.3243.
Samadi S, Khadivzadeh T, Emami A, et al. The effect of Hypericum perforatum on the wound healing and scar of cesarean. J Alter Complement Med. 2010;16:113–7. https://doi.org/10.1089/acm.2009.0317.
Güneş S, Tıhmınlıoğlu F. Hypericum perforatum incorporated chitosan films as potential bioactive wound dressing material. Int J Biol Macromol. 2017;102. https://doi.org/10.1016/j.ijbiomac.2017.04.080.
Kiaee G, Etaat M, Kiaee B, et al. Multilayered controlled released topical patch containing tetracycline for wound dressing. J In Silico In Vitro Pharmacol. 2016;2. No. 1:9.
Tihminlioglu F, Atik ID, Özen B. Water vapor and oxygen-barrier performance of corn-zein coated polypropylene films. J Food Eng. 2010;96:342–7. https://doi.org/10.1016/j.jfoodeng.2009.08.018.
Kimna C, Tamburaci S, Tihminlioglu F. Novel zein-based multilayer wound dressing membranes with controlled release of gentamicin. J Biomed Mater Res–Part B Appl Biomater. 2018:1–14. https://doi.org/10.1002/jbm.b.34298.
Eğri Ö, Erdemir N. Production of Hypericum perforatum oil-loaded membranes for wound dressing material and in vitro tests. Artif Cells Nanomed Biotechnol. 2019;47:1404–15. https://doi.org/10.1080/21691401.2019.1596933.
Zahedi P, Karami Z, Rezaeian I, et al. Preparation and performance evaluation of tetracycline hydrochloride loaded wound dressing mats based on electrospun nanofibrous poly(lactic acid)/poly(Ïμ-caprolactone) blends. J Appl Polym Sci. 2012;124:4174–83. https://doi.org/10.1002/app.35372.
ISO 10993–5. Biological evaluation of medical devices–Part 5: Tests for in vitro cytotoxicity. 2009.
Peter M, Thodi P, Kumar S, et al. Development of novel a-chitin/nanobioactive glass ceramic composite scaffolds for tissue engineering applications. Carbohydr Polym. 2009;78:926–31. https://doi.org/10.1016/j.carbpol.2009.07.016.
Liang C-C, Park AY, Guan J-L. In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc. 2007;2:329–33. https://doi.org/10.1038/nprot.2007.30.
Akturk O, Tezcaner A, Bilgili H, Deveci M, Gecit MKD. Evaluation of sericin/collagen membranes as prospective wound dressing biomaterial. J Biosci Bioeng. 2011;112:279–88.
Priya SG, Gupta A, Jain E, et al. Bilayer cryogel wound dressing and skin regeneration grafts for the treatment of acute skin wounds. ACS Appl Mater Interfaces. 2016;8:15145–59. https://doi.org/10.1021/acsami.6b04711.
Yoshino T, Isobe S, Maekawa T. Influence of preparation conditions on the physical properties of zein films. J Am Oil Chem Soc. 2002;79:345–9. https://doi.org/10.1007/s11746-002-0486-6.
Khan MIH, Islam JMM, Kabir W, et al. Development of hydrocolloid Bi-layer dressing with bio-adhesive and non-adhesive properties. Mater Sci Eng C. 2016;69:609–15. https://doi.org/10.1016/j.msec.2016.07.029.
Arcan I. Controlled release properties of zein—fatty acid blend films for multiple bioactive compounds. J Agric Food Chem. 2014;62:8238–46.
Gu L, Wang M, Zhou J. Effects of protein interactions on properties and microstructure of zein-gliadin composite films. J Food Eng. 2013;119:288–98. https://doi.org/10.1016/j.jfoodeng.2013.05.022.
Liu SJ, Kau YC, Chou CY, et al. Electrospun PLGA/collagen nanofibrous membrane as early-stage wound dressing. J Memb Sci. 2010;355:53–9. https://doi.org/10.1016/j.memsci.2010.03.012.
Suganya S, Venugopal J, Ramakrishna S, et al. Naturally derived biofunctional nanofibrous scaffold for skin tissue regeneration. Int J Biol Macromol. 2014. https://doi.org/10.1016/j.ijbiomac.2014.04.031.
Liu Y, Wang S, Zhang R, et al. Development of poly(lactic acid)/chitosan fibers loaded with essential oil for antimicrobial applications. Nanomaterials. 2017;7:194. https://doi.org/10.3390/nano7070194.
Kim MS, Kim D, Kang JK, et al. Migration of human dermal fibroblast is affected by the diameter of the electrospun PLGA fiber. Biomater Res. 2012. 16:135–9.
Zhang Y, Chwee TL, Ramakrishna S, Huang ZM. Recent development of polymer nanofibers for biomedical and biotechnological applications. J Mater Sci Mater Med. 2005;16:933–46.
Chong EJ, Phan TT, Lim IJ, et al. Evaluation of electrospun PCL/gelatin nanofibrous scaffold for wound healing and layered dermal reconstitution. Acta Biomater. 2007;3:321–30. https://doi.org/10.1016/j.actbio.2007.01.002.
MacNeil S. Progress and opportunities for tissue-engineered skin. Nature. 2007;445:874–80.
Torres-giner S, Gimenez E, Lagaron JM. Characterization of the morphology and thermal properties of zein prolamine nanostructures obtained by electrospinning. Food Hydrocolloid 2008;22:601–14. https://doi.org/10.1016/j.foodhyd.2007.02.005.
Vogt L, Liverani L. Electrospun zein fibers incorporating poly (glycerol sebacate) for soft tissue engineering. 2018:1–16. https://doi.org/10.3390/nano8030150.
Han YL, Xu Q, Lu ZQ, Wang JY. Preparation of transparent zein films for cell culture applications. Colloids Surf B Biointerfaces. 2014;120:55–62. https://doi.org/10.1016/j.colsurfb.2014.04.019.
Ozcalik O, Tihminlioglu F. Barrier properties of corn zein nanocomposite coated polypropylene films for food packaging applications. J Food Eng. 2013;114:505–13. https://doi.org/10.1016/j.jfoodeng.2012.09.005.
Yuan Y, Lee TR. Contact angle and wetting properties. In: Surface science techniques. Springer, Berlin, Heidelberg, 2013. pp 3–34.
Deng L, Kang X, Liu Y, et al. Characterization of gelatin/zein films fabricated by electrospinning vs solvent casting. Food Hydrocoll. 2018;74:324–32. https://doi.org/10.1016/j.foodhyd.2017.08.023.
Shi K, Kokini JL, Huang Q. Engineering zein films with controlled surface morphology and hydrophilicity engineering zein films with controlled surface morphology and hydrophilicity. J Agric Food Chem. 2009;57:2186–92. https://doi.org/10.1021/jf803559v.
Crockett SL. Essential oil and volatile components of the genus Hypericum (Hypericaceae). Nat Prod Commun 2010;5.9:1934578X1000500926.
Li K, Yin S, Yang X, et al. Fabrication and characterization of novel antimicrobial films derived from thymol-loaded zein—sodium caseinate (SC) nanoparticles. J Agric Food Chem 2012. https://doi.org/10.1021/jf302752v.
Cojocariu A, Profire L, Aflori M, Vasile C. In vitro drug release from chitosan/Cloisite 15A hydrogels. Appl Clay Sci. 2012;57:1–9. https://doi.org/10.1016/j.clay.2011.11.030.
Elkhyat A, Mac-Mary S, Humbert P. Skin Wettability and Friction. Handbook of cosmetic science and technology, 2009;427:337–44.
Prabhakaran MP, Venugopal JR, Chyan TT, et al. Electrospun biocomposite nanofibrous scaffolds for neural tissue engineering. Tissue Eng Part A. 2008;14:1787–97. https://doi.org/10.1089/ten.tea.2007.0393.
Menzies KL, Jones L. The impact of contact angle on the biocompatibility of biomaterials. Optom Vis Sci. 2010;87:387–99. https://doi.org/10.1097/OPX.0b013e3181da863e.
Abdollahi M, Rezaei M, Farzi G. A novel active bionanocomposite film incorporating rosemary essential oil and nanoclay into chitosan. J Food Eng. 2012;111:343–50. https://doi.org/10.1016/j.jfoodeng.2012.02.012.
Kouchak M, Ameri A, Naseri B, Kargar Boldaji S. Chitosan and polyvinyl alcohol composite films containing nitrofurazone: preparation and evaluation. Iran J Basic Med Sci. 2014;17:14–20.
Shelma R, Paul W, Sharma CP. Chitin nanofibre reinforced thin chitosan films for wound healing application. Trends Biomater Artif Organs. 2008;22:107–11.
Zahedi P, Rezaeian I, Ranaei-Siadat SO, et al. A review on wound dressings with an emphasis on electrospun nanofibrous polymeric bandages. Polym Adv Technol. 2010;21:77–95.
Akin O, Tihminlioglu F. Effects of organo-modified clay addition and temperature on the water vapor barrier properties of polyhydroxy butyrate homo and copolymer nanocomposite films for packaging applications. J Polym Environ. 2018. https://doi.org/10.1007/s10924-017-1017-2.
Bonilla J, Atarés L, Vargas M, Chiralt A. Effect of essential oils and homogenization conditions on properties of chitosan-based films. Food Hydrocoll. 2012;26:9–16. https://doi.org/10.1016/j.foodhyd.2011.03.015.
Altiok D, Altiok E, Tihminlioglu F. Physical, antibacterial and antioxidant properties of chitosan films incorporated with thyme oil for potential wound healing applications. J Mater Sci Mater Med. 2010;21:2227–36. https://doi.org/10.1007/s10856-010-4065-x.
Rojas-Graü Ma, Avena-Bustillos RJ, Olsen C, et al. Effects of plant essential oils and oil compounds on mechanical, barrier and antimicrobial properties of alginate-apple puree edible films. J Food Eng. 2007;81:634–41. https://doi.org/10.1016/j.jfoodeng.2007.01.007.
Xu R, Xia H, He W, et al. Controlled water vapor transmission rate promotes wound-healing via wound re-epithelialization and contraction enhancement. Sci Rep. 2016;6:1–12. https://doi.org/10.1038/srep24596.
Dreifke MB, Jayasuriya AA, Jayasuriya AC. Current wound healing procedures and potential care. Mater Sci Eng C. 2015;48:651–62. https://doi.org/10.1016/j.msec.2014.12.068.
Kataria K, Gupta A, Rath G, et al. In vivo wound healing performance of drug loaded electrospun composite nanofibers transdermal patch. Int J Pharm. 2014;469:102–10. https://doi.org/10.1016/j.ijpharm.2014.04.047.
Abdollahzadeh E, Rezaei M, Hosseini H. Antibacterial activity of plant essential oils and extracts: the role of thyme essential oil, nisin, and their combination to control Listeria monocytogenes inoculated in minced fish meat. Food Control. 2014;35:177–83. https://doi.org/10.1016/j.foodcont.2013.07.004.
Kıyan S, Uyanikgil Y, Altunci AY. Investigation of acute effects of hypericum perforatum (Kantaron) treatment in experimental thermal burns and comparison with silver sulfadiazine treatment. Turkish J Trauma Emerg Surg. 2015;21:323–36. https://doi.org/10.5505/tjtes.2015.63822.
Nazlı O, Baygar T, Elif Ç, et al. Antimicrobial and antibiofilm activity of polyurethane/Hypericum perforatum extract (PHPE) composite. Bioorg Chem. 2019;82:224–8. https://doi.org/10.1016/j.bioorg.2018.08.017.
Viseras C, Carazo ESC, Borrego-Sánchez A, et al. Clay Minerals in Skin Drug Delivery. Clays and Clay Minerals, 2019;67:59–71.
Mishra RK, Ramasamy K, Lim SM, et al. Antimicrobial and in vitro wound healing properties of novel clay based bionanocomposite films. J Mater Sci Mater Med. 2014;25:1925–39. https://doi.org/10.1007/s10856-014-5228-y.
Sun QS, Dong J, Lin ZX, et al. Comparison of cytocompatibility of zein film with other biomaterials and its degradability in vitro. Biopolymers. 2005;78:268–74. https://doi.org/10.1002/bip.20298.
Nakatani S, Mano H, Sampei C, et al. Chondroprotective effect of the bioactive peptide prolyl-hydroxyproline in mouse articular cartilage in vitro and in vivo. Osteoarthr Cartil. 2009;17:1620–7. https://doi.org/10.1016/j.joca.2009.07.001.
Shigemura YS, Iwai K, Morimatsu F, Iwamoto T, Mori T, Chikako O et al. Effect of prolyl-hydroxyproline (Pro-Hyp), a food-derived collagen peptide in human blood, on growth of fibroblasts from mouse skin. J Agric Food Chem. 2009;57:444–9.
Acknowledgements
The authors are grateful to İzmir Institute of Technology (Iztech) Biotechnology and Bioengineering Research and Application Center (IZTECH BIOMER) for antimicrobial activity tests, microscopy analyses and Center for Materials Research (IZTECH CMR) for SEM and AFM analyses. The content stored in and created with MindtheGraph.com was used in graphical abstract.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Gunes, S., Tamburaci, S. & Tihminlioglu, F. A novel bilayer zein/MMT nanocomposite incorporated with H. perforatum oil for wound healing. J Mater Sci: Mater Med 31, 7 (2020). https://doi.org/10.1007/s10856-019-6332-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6332-9