Abstract
Aims
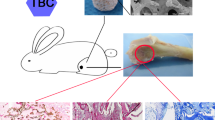
The present study aimed to evaluate whether the non-Smad dependent TAK1 signaling pathway (BMP-2-TAK1-p38-Osx signaling pathway) played an important role in bone repair mediated by hollow hydroxyapatite (HA) microspheres/chitosan (CS) composite.
Methods
Firstly, the biological activity of rhBMP-2 released from the complex was investigated. Then, differentiation test of osteoblasts including ALP activity and calcium deposition, X-ray scoring and three-point bending test were performed. Finally, the mRNAs expression of TAK1, p38, Osx and osteogenic markers was tested by reverse transcription-polymerase chain reaction (RT-PCR).
Results
RhBMP-2 could be loaded and released from the complex in bioactive form. Additionally, the complex provided a prolonged period of time compared with HA/CS scaffolds. Serum ALP activity was significantly decreased in the TAK1 inhibitor group and p38 inhibitor group. In the X-ray radiography, bone callus was observed in rhBMP-2-loaded hollow HA microspheres/CS composite group. In the three-point bending test, load values in p38 inhibitor group decreased. In the animal model, the mRNA expression of BSP on day 90 was significantly decreased in the p38 inhibitor group and TAK1 inhibitor group. In MC3T3-E1 cells, the mRNA expression of OSX was remarkably up-regulated in both rhBMP-2 group or rhBMP-2-loaded hollow HA microspheres/CS composite group; while the mRNA expression of OSX was significantly down-regulated in TAK1 inhibitor group and p38 inhibitor group.
Conclusion
The BMP-2-TAK1-p38-OSX signaling pathway may play an important role in bone formation and repair mediated by rhBMP-2-loaded hollow HA microspheres/CS composite.







Similar content being viewed by others
References
Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: an update. Injury. 2005;36(Suppl 3):S20. https://doi.org/10.1016/j.injury.2005.07.029.
Bauer TW, Muschler GF. Bone graft materials. An overview of the basic science. Clin Orthop Relat Res. 2000;10:27.
Fleming JE,Jr, Cornell CN, Muschler GF. Bone cells and matrices in orthopedic tissue engineering. Orthop Clin North Am. 2000;31:357.
Laurencin C, Khan Y, El-Amin SF. Bone graft substitutes. Expert Rev Med Devices. 2006;3:49. https://doi.org/10.1586/17434440.3.1.49.
Perry CR. Bone repair techniques, bone graft, and bone graft substitutes. Clin Orthop Relat Res. 1999;71:86.
Zimmermann G, Moghaddam A. Allograft bone matrix versus synthetic bone graft substitutes. Injury. 2011;42(Suppl 2):S16. https://doi.org/10.1016/j.injury.2011.06.199.
Crowley C, Wong JM, Fisher DM, Khan WS. A systematic review on preclinical and clinical studies on the use of scaffolds for bone repair in skeletal defects. Curr Stem Cell Res Ther. 2013;8:243.
Moore WR, Graves SE, Bain GI. Synthetic bone graft substitutes. ANZ J Surg. 2001;71:354.
Finkemeier CG. Bone-grafting and bone-graft substitutes. J Bone Jt Surg Am. 2002;84:454.
Kirker-Head CA. Potential applications and delivery strategies for bone morphogenetic proteins. Adv Drug Deliv Rev. 2000;43:65.
Fu H, Rahaman MN, Day DE, Brown RF. Hollow hydroxyapatite microspheres as a device for controlled delivery of proteins. J Mater Sci Mater Med. 2011;22:579. https://doi.org/10.1007/s10856-011-4250-6.
Shiels SM, Solomon KD, Pilia M, Appleford MR, Ong JL. BMP-2 tethered hydroxyapatite for bone tissue regeneration: coating chemistry and osteoblast attachment. J Biomed Mater Res Part A. 2012;100:3117. https://doi.org/10.1002/jbm.a.34241.
Babensee JE, McIntire LV, Mikos AG. Growth factor delivery for tissue engineering. Pharm Res. 2000;17:497.
Hong MH, Son JS, Kim KM, Han M, Oh DS, Lee YK. Drug-loaded porous spherical hydroxyapatite granules for bone regeneration. J Mater Sci Mater Med. 2011;22:349. https://doi.org/10.1007/s10856-010-4197-z.
Kean T, Thanou M. Biodegradation, biodistribution and toxicity of chitosan. Adv Drug Deliv Rev. 2010;62:3. https://doi.org/10.1016/j.addr.2009.09.004.
Onishi H, Machida Y. Biodegradation and distribution of water-soluble chitosan in mice. Biomaterials. 1999;20:175.
Dimitriou R, Tsiridis E, Giannoudis PV. Current concepts of molecular aspects of bone healing. Injury. 2005;36:1392. https://doi.org/10.1016/j.injury.2005.07.019.
Abarrategi A, Gutierrez MC, Moreno-Vicente C, Hortigüela MJ, Ramos V, López-Lacomba JL, et al. Multiwall carbon nanotube scaffolds for tissue engineering purposes. Biomaterials. 2008;29:94. https://doi.org/10.1016/j.biomaterials.2007.09.021.
Abarrategi A, Moreno-Vicente C, Ramos V, Aranaz I, Sanz Casado JV, Lopez-Lacomba JL. Improvement of porous beta-TCP scaffolds with rhBMP-2 chitosan carrier film for bone tissue application. Tissue Eng Part A. 2008;14:1305. https://doi.org/10.1089/ten.tea.2007.0229.
Lopez-Lacomba JL, Garcia-Cantalejo JM, Sanz Casado JV, Abarrategi A, Correas Magana V, Ramos V. Use of rhBMP-2 Activated Chitosan Films To Improve Osseointegration. Biomacromolecules. 2006;7:792. https://doi.org/10.1021/bm050859e.
Stephan SJ, Tholpady SS, Gross B, Petrie-Aronin CE, Botchway EA, Nair LS, et al. Injectable tissue-engineered bone repair of a rat calvarial defect. Laryngoscope. 2010;120:895. https://doi.org/10.1002/lary.20624.
Yao AH, Li XD, Xiong L, Zeng JH, Xu J, Wang DP. Hollow hydroxyapatite microspheres/chitosan composite as a sustained delivery vehicle for rhBMP-2 in the treatment of bone defects. J Mater Sci Mater Med. 2015;26:5336. https://doi.org/10.1007/s10856-014-5336-8.
Xiong L, Zeng J, Yao A, Tu Q, Li J, Yan L, et al. BMP2-loaded hollow hydroxyapatite microspheres exhibit enhanced osteoinduction and osteogenicity in large bone defects. Int J Nanomed. 2015;10:517. https://doi.org/10.2147/ijn.s74677.
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, et al. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell. 2002;108:17.
Zhou X, Zhang Z, Feng JQ, Dusevich VM, Sinha K, Zhang H, et al. Multiple functions of Osterix are required for bone growth and homeostasis in postnatal mice. Proc Natl Acad Sci USA. 2010;107:12919. https://doi.org/10.1073/pnas.0912855107.
Chen G, Deng C, Li YP. TGF-β and BMP signaling in osteoblast differentiation and bone formation. Int J Biol Sci. 2012;8:272. https://doi.org/10.7150/ijbs.2929.
Yang F, Wang J, Hou J, Guo H, Liu C. Bone regeneration using cell-mediated responsive degradable PEG-based scaffolds incorporating with rhBMP-2. Biomaterials. 2013;34:1514. https://doi.org/10.1016/j.biomaterials.2012.10.058.
Athanasiou VT, Papachristou DJ, Panagopoulos A, Saridis A, Scopa CD, Megas P. Histological comparison of autograft, allograft-DBM, xenograft, and synthetic grafts in a trabecular bone defect: an experimental study in rabbits. Med Sci Monit. 2010;16:Br24.
Marom R, Shur I, Solomon R, Benayahu D. Characterization of adhesion and differentiation markers of osteogenic marrow stromal cells. J Cell Physiol. 2005;202:41. https://doi.org/10.1002/jcp.20109.
Stucki U, Schmid J, Hammerle CF, Lang NP. Temporal and local appearance of alkaline phosphatase activity in early stages of guided bone regeneration. A descriptive histochemical study in humans. Clin Oral Implants Res. 2001;12:121.
Bigham AS, Dehghani SN, Shafiei Z, Torabi Nezhad S. Xenogenic demineralized bone matrix and fresh autogenous cortical bone effects on experimental bone healing: radiological, histopathological and biomechanical evaluation. J Orthop Traumatol. 2008;9:73. https://doi.org/10.1007/s10195-008-0006-6.
Acknowledgements
This study was funded by National Natural Science Foundation of China of “The mechanism research of non-Smad dependent TAK1 signaling pathway in the treatment of bone defects by recombination BMP-2-loaded hollow hydroxyapatite microspheres/chitosan composite” (81560355) and “Mechanism study of bone repair mediated by rhBMP-2/rhCXCL13-loaded hollow hydroxyapatite microspheres/chitosan composite” (81560377).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving Animals
All animal studies were approved by the Jiangxi Provincial People’s Hospital Affiliated to Nanchang University and were in accordance with the Guidelines for Care and Use of Experimental Animals.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Xiong, S., Ding, L. et al. The mechanism research of non-Smad dependent TAK1 signaling pathway in the treatment of bone defects by recombination BMP-2-loaded hollow hydroxyapatite microspheres/chitosan composite. J Mater Sci: Mater Med 30, 130 (2019). https://doi.org/10.1007/s10856-019-6340-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6340-9