Abstract
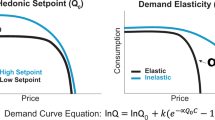
The origins and neural bases of the current opioid addiction epidemic are unclear. Genetics plays a major role in addiction vulnerability, but cannot account for the recent exponential rise in opioid abuse, so environmental factors must contribute. Individuals with history of early life adversity (ELA) are disproportionately prone to opioid addiction, yet whether ELA interacts with factors such as increased access to opioids to directly influence brain development and function, and cause opioid addiction vulnerability, is unknown. We simulated ELA in female rats and this led to a striking opioid addiction-like phenotype. This was characterized by resistance to extinction, increased relapse-like behavior, and, as in addicted humans, major increases in opioid economic demand. By contrast, seeking of a less salient natural reward was unaffected by ELA, whereas demand for highly palatable treats was augmented. These discoveries provide novel insights into the origins and nature of reward circuit malfunction that may set the stage for addiction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data forming the basis of these studies do not include genomic or imaging data sets storable in public repositories. Data will be readily made available when requested from the authors.
References
Volkow ND, Collins FS. The role of science in addressing the opioid crisis. https://doi.org/10.1056/NEJMsr1706626. 2017.
Morrow JD, Flagel SB. Neuroscience of resilience and vulnerability for addiction medicine: From genes to behavior. Prog Brain Res. 2016;223:3–18.
Cates HM, Benca-Bachman CE, de Guglielmo G, Schoenrock SA, Shu C, Kallupi M. National Institute on Drug Abuse genomics consortium white paper: Coordinating efforts between human and animal addiction studies. Genes Brain Behav. 2019;18:e12577.
Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health. 2009;99:221–7.
Gershon A, Minor K, Hayward C. Gender, victimization, and psychiatric outcomes. Psychol Med. 2008;38:1377–91.
Shand FL, Degenhardt L, Slade T, Nelson EC. Sex differences amongst dependent heroin users: Histories, clinical characteristics and predictors of other substance dependence. Addict Behav. 2011;36:27–36.
Widom CS, Marmorstein NR, White HR. Childhood victimization and illicit drug use in middle adulthood. Psychol Addict Behav. 2006;20:394–403.
Marsh JC, Park K, Lin YA, Bersamira C. Gender differences in trends for heroin use and nonmedical prescription opioid use, 2007-2014. J Subst Abus Treat. 2018;87:79–85.
Enoch M-A. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology. 2011;214:17–31.
Danese A, Moffitt TE, Arseneault L, Bleiberg BA, Dinardo PB, Gandelman SB, et al. The origins of cognitive deficits in victimized children: implications for neuroscientists and clinicians. Am J Psychiatry. 2017;174:349–61.
Chen Y, Baram TZ. Toward understanding how early-life stress reprograms cognitive and emotional brain networks. Neuropsychopharmacology. 2016;41:197.
Bolton JL, Molet J, Regev L, Chen Y, Rismanchi N, Haddad E, et al. Anhedonia following early-life adversity involves aberrant interaction of reward and anxiety circuits and is reversed by partial silencing of amygdala corticotropin-releasing hormone gene. Biol Psychiatry. 2018;83:137–47.
Ivy AS, Brunson KL, Sandman C, Baram TZ. Dysfunctional nurturing behavior in rat dams with limited access to nesting material: a clinically relevant model for early-life stress. Neuroscience. 2008;154:1132–42.
Molet J, Heins K, Zhuo X, Mei YT, Regev L, Baram TZ et al. Fragmentation and high entropy of neonatal experience predict adolescent emotional outcome. Transl Psychiatry. 2016;6:e702.
Molet J, Maras PM, Avishai‐Eliner S, Baram TZ. Naturalistic rodent models of chronic early‐life stress. Dev Psychobiol. 2014;56:1675–88.
Smith RJ, Aston‐Jones G. Orexin / hypocretin 1 receptor antagonist reduces heroin self‐administration and cue‐induced heroin seeking. Eur J Neurosci. 2012;35:798–804.
Bolton JL, Ruiz CM, Rismanchi N, Sanchez GA, Castillo E, Huang J, et al. Early-life adversity facilitates acquisition of cocaine self-administration and induces persistent anhedonia. Neurobiol Stress. 2018;8:57–67.
Porter‐Stransky KA, Bentzley BS, Aston‐Jones G. Individual differences in orexin‐I receptor modulation of motivation for the opioid remifentanil. Addict Biol. 2017;22:303–17.
Bentzley BS, Fender KM, Aston-Jones G. The behavioral economics of drug self-administration: a review and new analytical approach for within-session procedures. Psychopharmacology. 2013;226:113–25.
Oleson EB, Roberts D. Parsing the addiction phenomenon: Self-administration procedures modeling enhanced motivation for drug and escalation of drug intake. Drug Discov Today. 2009;5:217–26.
Cox BM, Bentzley BS, Regen-Tuero H, See RE, Reichel CM, Aston-Jones G. Oxytocin acts in nucleus accumbens to attenuate methamphetamine seeking and demand. Biol Psychiatry. 2017;81:949–58.
Bland JM, Altman DG. The logrank test. BMJ 2004;328:1073.
Milton AL, Everitt BJ. The persistence of maladaptive memory: addiction, drug memories and anti-relapse treatments. Neurosci Biobehav Rev. 2012;36:1119–39.
Vanderschuren LJ, Ahmed SH. Animal studies of addictive behavior. Cold Spring Harb Perspect Med. 2013;3:a011932.
Weiss F. Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharm. 2005;5:9–19.
Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Annu Rev Clin Psychol. 2007;3:257–84.
Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–77.
Hursh SR. Economic concepts for the analysis of behavior. J Exp Anal Behav. 1980;34:219–38.
Bentzley BS, Jhou TC, Aston-Jones G. Economic demand predicts addiction-like behavior and therapeutic efficacy of oxytocin in the rat. Proc Natl Acad Sci. 2014;111:11822–7.
Strickland JC, Lile JA, Stoops WW. Evaluating non-medical prescription opioid demand using commodity purchase tasks: test-retest reliability and incremental validity. Psychopharmacology. 2019;236:2641–52.
Slattery DA, Cryan JF. Modelling depression in animals: at the interface of reward and stress pathways. Psychopharmacology. 2017;234:1451–65.
Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012;35:68–77.
Russo SJ, Nestler EJ. The brain reward circuitry in mood disorders. Nat Rev Neurosci. 2013;14:609–25.
Espinosa JS, Stryker MP. Development and plasticity of the primary visual cortex. Neuron. 2012;75:230–49.
Barkat TR, Polley DB, Hensch TK. A critical period for auditory thalamocortical connectivity. Nat Neurosci. 2011;14:1189–94.
Davis EP, Stout SA, Molet J, Vegetabile B, Glynn LM, Sandman CA, et al. Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proc Natl Acad Sci USA. 2017;114:10390–5.
Rincón-Cortés M, Herman JP, Lupien S, Maguire J, Shansky RM. Stress: Influence of sex, reproductive status and gender. Neurobiol Stress. 2019;10:100155.
Luby JL, Barch D, Whalen D, Tillman R, Belden A. Association between early life adversity and risk for poor emotional and physical health in adolescence: a putative mechanistic neurodevelopmental pathway. JAMA Pediatr. 2017;171:1168–75.
Doherty TS, Blaze J, Keller SM, Roth TL. Phenotypic outcomes in adolescence and adulthood in the scarcity-adversity model of low nesting resources outside the home cage. Dev Psychobiol. 2017;59:703–14.
Goodwill HL, Manzano-Nieves G, Gallo M, Lee H-I, Oyerinde E, Serre T et al. Early life stress leads to sex differences in development of depressive-like outcomes in a mouse model. Neuropsychopharmacology. 2019;44:711–720.
Mavrikaki M, Pravetoni M, Page S, Potter D, Chartoff E. Oxycodone self-administration in male and female rats. Psychopharmacology. 2017;234:977–87.
Cicero TJ, Aylward SC, Meyer ER. Gender differences in the intravenous self-administration of mu opiate agonists. Pharm Biochem Behav. 2003;74:541–9.
Acknowledgements
We thank the National Institute on Drug Abuse (NIDA) Drug Supply Program (Research Triangle Park, NC, USA), for providing heroin and remifentanil.
Funding
The research was supported in part by NIH grants MH096889; NS28912; DA035251; DA044118; GM008620; MH119049 and the Hewitt Foundation for Biomedical Research
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Levis, S.C., Bentzley, B.S., Molet, J. et al. On the early life origins of vulnerability to opioid addiction. Mol Psychiatry 26, 4409–4416 (2021). https://doi.org/10.1038/s41380-019-0628-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-019-0628-5
This article is cited by
-
Early life stress in male mice blunts responsiveness in a translationally-relevant reward task
Neuropsychopharmacology (2023)
-
A Guide to Expanding the Use of Buprenorphine Beyond Standard Initiations for Opioid Use Disorder
Drugs in R&D (2023)
-
Neuroscience in addiction research
Journal of Neural Transmission (2023)
-
Oxytocin as an adolescent treatment for methamphetamine addiction after early life stress in male and female rats
Neuropsychopharmacology (2022)
-
Enduring disruption of reward and stress circuit activities by early-life adversity in male rats
Translational Psychiatry (2022)