Abstract
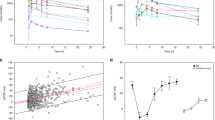
Rational new strategies are needed to treat tumors resistant to kinase inhibitors. Mechanistic studies of resistance provide fertile ground for development of new approaches. Cancer drug addiction is a paradoxical resistance phenomenon, well-described in MEK-ERK-driven solid tumors, in which drug-target overexpression promotes resistance but a toxic overdose of signaling if the inhibitor is withdrawn. This can permit prolonged control of tumors through intermittent dosing. We and others showed previously that cancer drug addiction arises also in the hematologic malignancy ALK-positive anaplastic large-cell lymphoma (ALCL) resistant to ALK-specific tyrosine kinase inhibitors (TKIs). This is driven by the overexpression of the fusion kinase NPM1-ALK, but the mechanism by which ALK overactivity drives toxicity upon TKI withdrawal remained obscure. Here we reveal the mechanism of ALK-TKI addiction in ALCL. We interrogated the well-described mechanism of MEK/ERK pathway inhibitor addiction in solid tumors and found it does not apply to ALCL. Instead, phosphoproteomics and confirmatory functional studies revealed that the STAT1 overactivation is the key mechanism of ALK-TKI addiction in ALCL. The withdrawal of TKI from addicted tumors in vitro and in vivo leads to overwhelming phospho-STAT1 activation, turning on its tumor-suppressive gene-expression program and turning off STAT3’s oncogenic program. Moreover, a novel NPM1-ALK-positive ALCL PDX model showed a significant survival benefit from intermittent compared with continuous TKI dosing. In sum, we reveal for the first time the mechanism of cancer drug addiction in ALK-positive ALCL and the benefit of scheduled intermittent dosing in high-risk patient-derived tumors in vivo.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Code availability
All codes were run on the open-source programming environment R (version 3.3.1). The area under the curve was analyzed using the equation mentioned previously and the open-source package “AUC”. The RNA-Seq was visualized as a heatmap using the open-source built-in package “heatmap”.
References
Ferguson FM, Gray NS. Kinase inhibitors: the road ahead. Nat Rev Drug Discov. 2018;17:353–77.
Suda K, Tomizawa K, Osada H, Maehara Y, Yatabe Y, Sekido Y, et al. Conversion from the “oncogene addiction” to “drug addiction” by intensive inhibition of the EGFR and MET in lung cancer with activating EGFR mutation. Lung Cancer. 2012;76:292–9.
Sun C, Wang L, Huang S, GJJE Heynen, Prahallad A, Robert C, et al. Reversible and adaptive resistance to BRAF(V600E) inhibition in melanoma. Nature. 2014;508:118–22.
Moriceau G, Hugo W, Hong A, Shi H, Kong X, Yu CC, et al. Tunable-combinatorial mechanisms of acquired resistance limit the efficacy of BRAF/MEK cotargeting but result in melanoma drug addiction. Cancer Cell. 2015;27:240–56.
Das Thakur M, Salangsang F, Landman AS, Sellers WR, Pryer NK, Levesque MP, et al. Modelling vemurafenib resistance in melanoma reveals a strategy to forestall drug resistance. Nature. 2013;494:251–5.
Kong X, Kuilman T, Shahrabi A, Boshuizen J, Kemper K, Song J-Y, et al. Cancer drug addiction is relayed by an ERK2-dependent phenotype switch. Nature. 2017;550:270–4.
Amin AD, Rajan SS, Liang WS, Pongtornpipat P, Groysman MJ, Tapia EO, et al. Evidence suggesting that discontinuous dosing of ALK kinase inhibitors may prolong control of ALK+ tumors. Cancer Res. 2015;75:2916–27.
Morris SW, Kirstein MN, Valentine MB, Dittmer KG, Shapiro DN, Saltman DL, et al. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science. 1994;263:1281–4.
Kwak EL, Bang Y-J, Camidge DR, Shaw AT, Solomon B, Maki RG, et al. Anaplastic lymphoma kinase inhibition in non–small-cell lung cancer. N. Engl J Med. 2010;363:1693–703.
Gainor JF, Dardaei L, Yoda S, Friboulet L, Leshchiner I, Katayama R, et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in alk-rearranged lung cancer. Cancer Discov. 2016;6:1118–33.
Gambacorti-Passerini C, Messa C, Pogliani EM. Crizotinib in anaplastic large-cell lymphoma. N. Engl J Med. 2011;364:775–6.
Mossé YP, Voss SD, Lim MS, Rolland D, Minard CG, Fox E, et al. Targeting ALK with crizotinib in pediatric anaplastic large cell lymphoma and inflammatory myofibroblastic tumor: a Children’s Oncology Group Study. J Clin Oncol. 2017;35:3215–21.
Ceccon M, Merlo MEB, Mologni L, Poggio T, Varesio LM, Menotti M, et al. Excess of NPM-ALK oncogenic signaling promotes cellular apoptosis and drug dependency. Oncogene. 2015. https://doi.org/10.1038/onc.2015.456.
Redaelli S, Ceccon M, Zappa M, Sharma GG, Mastini C, Mauri M, et al. Lorlatinib treatment elicits multiple on- and off-target mechanisms of resistance in ALK-driven cancer. Cancer Res. 2018;78:6866–80.
Adam P, Katzenberger T, Seeberger H, Gattenlöhner S, Wolf J, Steinlein C, et al. A case of a diffuse large B-cell lymphoma of plasmablastic type associated with the t(2;5)(p23;q35) chromosome translocation. Am J Surgical Pathol. 2003;27:1473–6.
Onciu M, Behm FG, Downing JR, Shurtleff SA, Raimondi SC, Ma Z, et al. ALK-positive plasmablastic B-cell lymphoma with expression of the NPM-ALK fusion transcript: report of 2 cases. Blood. 2003;102:2642–4.
Pearson JD, Lee JKH, Bacani JTC, Lai R, Ingham RJ. NPM-ALK: the prototypic member of a family of oncogenic fusion tyrosine kinases. J Signal Transduct. 2012;2012:1–14.
Marzec M, Kasprzycka M, Liu X, Raghunath PN, Wlodarski P, Wasik MA. Oncogenic tyrosine kinase NPM/ALK induces activation of the MEK/ERK signaling pathway independently of c-Raf. Oncogene. 2006;26:813–21.
Chiarle R, Simmons WJ, Cai H, Dhall G, Zamo A, Raz R, et al. Stat3 is required for ALK-mediated lymphomagenesis and provides a possible therapeutic target. Nat Med. 2005;11:623–9.
Kodama T, Tsukaguchi T, Yoshida M, Kondoh O, Sakamoto H. Selective ALK inhibitor alectinib with potent antitumor activity in models of crizotinib resistance. Cancer Lett. 2014;351:215–21.
Johnson TW, Richardson PF, Bailey S, Brooun A, Burke BJ, Collins MR, et al. Discovery of (10 R)-7-amino-12-fluoro-2,10,16-trimethyl-15-oxo-10,15,16,17-tetrahydro-2H-8,4-(metheno)pyrazolo[4,3-h][2,5,11]-benzoxadiazacyclotetradecine-3-carbonitrile (PF-06463922), a macrocyclic inhibitor of anaplastic lymphoma kinase (ALK) and c-ros oncogene 1 (ROS1) with preclinical brain exposure and broad-spectrum potency against ALK-resistant mutations. J Med Chem. 2014;57:4720–44.
Duncan JS, Whittle MC, Nakamura K, Abell AN, Midland AA, Zawistowski JS, et al. Dynamic reprogramming of the kinome in response to targeted MEK inhibition in triple-negative breast. Cancer Cell. 2012;149:307–21.
McDonnell SRP, Hwang SR, Rolland D, Murga-Zamalloa C, Basrur V, Conlon KP, et al. Integrated phosphoproteomic and metabolomic profiling reveals NPM-ALK-mediated phosphorylation of PKM2 and metabolic reprogramming in anaplastic large cell lymphoma. Blood. 2013. https://doi.org/10.1182/blood-2013-01-482026.
Bai R-Y, Dieter P, Peschel C, Morris SW, Duyster J. Nucleophosmin-anaplastic lymphoma kinase of large-cell anaplastic lymphoma is a constitutively active tyrosine kinase that utilizes phospholipase C-γ to mediate its mitogenicity. Mol Cell Biol. 1998;18:6951–61.
Crockett DK, Lin Z, Elenitoba-Johnson KS, Lim MS. Identification of NPM-ALK interacting proteins by tandem mass spectrometry. Oncogene. 2004;23:2617–29.
Cui Y-X, Kerby A, McDuff FKE, Ye H, Turner SD. NPM-ALK inhibits the p53 tumor suppressor pathway in an MDM2 and JNK-dependent manner. Blood. 2009;113:5217–27.
McDonnell SRP, Hwang SR, Basrur V, Conlon KP, Fermin D, Wey E, et al. NPM-ALK signals through glycogen synthase kinase 3β to promote oncogenesis. Oncogene. 2011;31:3733–40.
Houghton PJ, Kurmasheva RT, Lyalin D, Maris JM, Kolb EA, Gorlick R, et al. Initial solid tumor testing (Stage 1) of AZD1480, an inhibitor of Janus kinases 1 and 2 by the pediatric preclinical testing program: AZD1480 pediatric preclinical testing. Pediatr Blood Cancer. 2014;61:1972–79.
Bromberg JF, Wrzeszczynska MH, Devgan G, Zhao Y, Pestell RG, Albanese C, et al. Stat3 as an oncogene. Cell. 1999;98:295–303.
Brunet A, Pagès G, Pouysségur J. Constitutively active mutants of MAP kinase kinase (MEK1) induce growth factor-relaxation and oncogenicity when expressed in fibroblasts. Oncogene. 1994;9:3379–87.
Lim MS, Carlson ML, Crockett DK, Fillmore GC, Abbott DR, Elenitoba-Johnson OF, et al. The proteomic signature of NPM/ALK reveals deregulation of multiple cellular pathways. Blood. 2009;114:1585–95.
Sattu K, Hochgräfe F, Wu J, Umapathy G, Schönherr C, Ruuth K, et al. Phosphoproteomic analysis of anaplastic lymphoma kinase (ALK) downstream signaling pathways identifies signal transducer and activator of transcription 3 as a functional target of activated ALK in neuroblastoma cells. FEBS J. 2013;280:5269–82.
Xiao Y, Qiao G, Tang J, Tang R, Guo H, Warwar S, et al. Protein tyrosine phosphatase SHP-1 modulates t cell responses by controlling Cbl-b degradation. J Immunol. 2015;195:4218–27.
Kameda H, Watanabe M, Bohgaki M, Tsukiyama T, Hatakeyama S. Inhibition of NF-κB signaling via tyrosine phosphorylation of Ymer. Biochem Biophys Res Commun. 2009;378:744–9.
Yokoyama K, Tezuka T, Kotani M, Nakazawa T, Hoshina N, Shimoda Y, et al. NYAP: a phosphoprotein family that links PI3K to WAVE1 signalling in neurons. EMBO J. 2011;30:4739–54.
Croucher DR, Hochgräfe F, Zhang L, Liu L, Lyons RJ, Rickwood D, et al. Involvement of Lyn and the atypical kinase SgK269/PEAK1 in a basal breast cancer signaling pathway. Cancer Res. 2013;73:1969–80.
Rickert KW, Patel SB, Allison TJ, Byrne NJ, Darke PL, Ford RE, et al. Structural basis for selective small molecule kinase inhibition of activated c-Met. J Biol Chem. 2011;286:11218–25.
Wu C, Molavi O, Zhang H, Gupta N, Alshareef A, Bone KM, et al. STAT1 is phosphorylated and downregulated by the oncogenic tyrosine kinase NPM-ALK in ALK-positive anaplastic large-cell lymphoma. Blood. 2015;126:336–45.
Shuai K, Stark GR, Kerr IM, Darnell JE. A single phosphotyrosine residue of Stat91 required for gene activation by interferon-gamma. Science. 1993;261:1744–6.
Shuai K, Ziemiecki A, Wilks AF, Harpur AG, Sadowski HB, Gilman MZ, et al. Polypeptide signalling to the nucleus through tyrosine phosphorylation of Jak and Stat proteins. Nature. 1993;366:580.
Tamura T, Ishihara M, Lamphier MS, Tanaka N, Oishi I, Aizawa S, et al. An IRF-1-dependent pathway of DNA damage-induced apoptosis in mitogen-activated T lymphocytes. Nature. 1995;376:596.
Tanaka N, Ishihara M, Kitagawa M, Harada H, Kimura T, Matsuyama T, et al. Cellular commitment to oncogene-induced transformation or apoptosis is dependent on the transcription factor IRF-1. Cell. 1994;77:829–39.
Tanaka N, Ishihara M, Lamphier MS, Nozawa H, Matsuyama T, Mak TW, et al. Cooperation of the tumour suppressors IRF-1 and p53 in response to DNA damage. Nature. 1996;382:816.
Gardeux V, Achour I, Li J, Maienschein-Cline M, Li H, Pesce L, et al. ‘N-of-1-pathways’ unveils personal deregulated mechanisms from a single pair of RNA-Seq samples: towards precision medicine. J Am Med Inform Assoc. 2014;21:1015–25.
Satoh J, Tabunoki H. A comprehensive profile of ChIP-seq-based STAT1 target genes suggests the complexity of STAT1-mediated gene regulatory mechanisms. Gene Regul Syst Bio. 2013;7:GRSB.S11433.
Carpenter RL, Lo H-W. STAT3 target genes relevant to human cancers. Cancers. 2014;6:897–925.
Sironi JJ, Ouchi T. STAT1-induced apoptosis is mediated by caspases 2, 3, and 7. J Biol Chem. 2004;279:4066–74.
Bonvini P, Dalla Rosa H, Vignes N, Rosolen A. Ubiquitination and proteasomal degradation of nucleophosmin-anaplastic lymphoma kinase induced by 17-allylamino-demethoxygeldanamycin: role of the co-chaperone carboxyl heat shock protein 70-interacting protein. Cancer Res. 2004;64:3256–64.
Piva R, Agnelli L, Pellegrino E, Todoerti K, Grosso V, Tamagno I, et al. Gene expression profiling uncovers molecular classifiers for the recognition of anaplastic large-cell lymphoma within peripheral T-cell neoplasms. J Clin Oncol. 2010;28:1583–90.
Pensa S, Regis G, Boselli D, Novelli F, Poli V. STAT1 and STAT3 in tumorigenesis: two sides of the same coin? Austin, Texas, USA: Landes Bioscience; 2013. https://www.ncbi.nlm.nih.gov/books/NBK6568/ Accessed 5 Sept 2018.
Prutsch N, Gurnhofer E, Suske T, Liang HC, Schlederer M, Roos S, et al. Dependency on the TYK2/STAT1/MCL1 axis in anaplastic large cell lymphoma. Leukemia. 2019;33:696–709.
Haan S, Keller JF, Behrmann I, Heinrich PC, Haan C. Multiple reasons for an inefficient STAT1 response upon IL-6-type cytokine stimulation. Cell Signal. 2005;17:1542–50.
Hong A, Moriceau G, Sun L, Lomeli S, Piva M, Damoiseaux R, et al. Exploiting drug addiction mechanisms to select against MAPKi-resistant melanoma. Cancer Discov. 2018;8:74–93.
Passerini CG, Farina F, Stasia A, Redaelli S, Ceccon M, Mologni L, et al. Crizotinib in advanced, chemoresistant anaplastic lymphoma kinase–positive lymphoma patients. J Natl Cancer Inst. 2014;106:djt378.
Beebe JD, Liu J-Y, Zhang J-T. Two decades of research in discovery of anticancer drugs targeting STAT3, how close are we? Pharmacol Ther. 2018. https://doi.org/10.1016/j.pharmthera.2018.06.006.
Acknowledgements
This work was supported by a grant from National Institutes of Health/National Cancer Institute, 1R01CA190696-01 (JHS) and 5R01CA190696-05. We would also like to acknowledge the Sheila and David Fuente Graduate Program in Cancer Biology at University of Miami. SSR is a PhD candidate at University of Miami. This work is submitted in partial fulfillment of the requirement of the PhD. We would also like to thank Dr Izidore Lossos, University of Miami, for his input and suggestions in writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rajan, S.S., Amin, A.D., Li, L. et al. The mechanism of cancer drug addiction in ALK-positive T-Cell lymphoma. Oncogene 39, 2103–2117 (2020). https://doi.org/10.1038/s41388-019-1136-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-019-1136-4
This article is cited by
-
In situ self-assembly for cancer therapy and imaging
Nature Reviews Materials (2023)
-
Drug addiction unveils a repressive methylation ceiling in EZH2-mutant lymphoma
Nature Chemical Biology (2023)