Abstract
Background
Bone strain index (BSI) is a tool measuring bone strain, derived from dual x-ray photon absorptiometry. It is able to characterise an aspect of bone quality that, joined to the quantity and quality parameters of bone mineral density (BMD) and trabecular bone score (TBS), permits an accurate definition of fracture risk. As no data are available about BSI precision, our aim was to assess its in vitro reproducibility.
Methods
A Hologic spine phantom was used to perform BSI scans with three different scan modes: fast array (FA), array (A), and high definition (HD). Different soft tissue thicknesses (1, 3, 6 cm) of fresh pork rind layers as a surrogate of abdominal fat were interposed. For each scan mode, the phantom was consecutively scanned 25 times without repositioning.
Results
In all scan modes (FA, A, HD) and at every fat thickness, BSI reproducibility was lower than that of BMD. The highest reproducibility was found using HD-mode with 1 cm of pork rind and the lowest one using HD-mode with 6 cm of pork rind. Increasing fat thickness, BSI reproducibility tended to decrease. BSI least significant change appeared to be about three times that of BMD in all modalities and fat thicknesses. Without pork rind superimposition and with 1-cm fat layer, BSI reproducibility was highest with HD-mode; with 3 or 6 cm fat thickness, it was higher with A-mode.
Conclusions
BSI reproducibility was worse than that of BMD, but it is less sensitive to fat thickness increase, similarly to TBS.
Similar content being viewed by others
Key points
-
Bone strain index (BSI) is an index of bone quality derived from dual-energy x-ray absorptiometry.
-
BSI reproducibility was tested in a spine phantom study.
-
BSI reproducibility was lower than that of bone mineral density (BMD) and tended to decrease with the increase of interposed swine fat tissue.
-
BSI reproducibility was less sensitive to the increase of interposed fat thickness than BMD.
-
BSI behaviour is similar to that of other bone quality indexes, such as trabecular bone score.
Background
Osteoporosis is defined as a skeletal condition characterised by reduced bone strength, due to an impaired bone mass and compromised microarchitecture that cause an increased risk of non-traumatic fragility fractures [1]. Fragility fractures are important clinical events because they increase the disability and mortality related to this disease, with high social costs [1]. In addition, the presence of a fragility fracture itself predisposes to the recurrence of new fractures [1,2,3].
Dual x-ray photon absorptiometry (DXA) is considered the gold standard method for the diagnosis of reduced bone mass and for its follow-up [4]. Bone mineral density (BMD) is the most relevant parameter of bone load resistance and is calculated as bone mineral content on area (g/cm2). It is expressed by T-score and Z-score, indicating how the measured data diverge from the mean value of a normal population or from the mean value of a population of the same sex and age, respectively. According to the World Health Organization criteria, a T-score lower than -2.5 defines the cutoff for the diagnosis of osteoporosis in postmenopausal women and men over 50, while a Z-score lower than -2.0 represents the cutoff for the diagnosis of reduced bone mass in premenopausal women and men under 50 [5].
However, while BMD is clearly one of the major determinants of bone strength [6], the assessment of fracture risk based on BMD alone could lack sensitivity. In fact, many fragility fractures occur in osteopenic individuals (T score between -2.5 and -1.0), not only in subjects with osteoporosis (T score below -2.5) [7]. Other factors in addition to BMD account for bone strength and fracture risk, concurring to determine bone quality [8]. They are represented by trabecular architecture, bone geometry, and bone turnover. The last one is evaluated by biochemical assays, while the first two can be directly measured by bone biopsy. Recently, the use of DXA has been enriched with new software that are capable to provide information on bone microarchitecture and turnover, such as the trabecular bone score (TBS) and the hip structural analysis [9].
In this scenario, another DXA-derived software has been recently developed with the aim of further investigating bone quality, a tool called bone strain index (BSI) [10]. This software applies a mathematical model called finite element method (FEM) to DXA lumbar spine scans. FEM derived from quantitative computed tomography scans demonstrated to be predictive of experimental vertebra strength [11]. The BSI parameter uses the format of digital imaging and communications in medicine (DICOM) files to obtain an average strain field from FEM analysis, calculated within each lumbar vertebra. The force acting on the surface of each vertebra has been related to the height and weight of each patient. A classical mathematical matricial approach using a triangular mesh and FEM has been applied defining the stiffness matrix dependent from the local BMD. The result of this process is the distribution of the strain that is defined as the spatial deformation of every single element in which the vertebra was divided before the calculation [12]. In order to make this analysis easier in daily usage, the model described above has been completely automated integrating both the segmentation process and FEM analysis in a single software [10]. A recent analysis of the BSI software showed a good correlation between BSI and the yield strain applied to porcine vertebrae, meaning that BSI can be a predictor of elastic and plastic changes in the mechanical response of the bone. As a consequence, BSI could be applied in the prediction of the possible region of fracture within the vertebrae. When the software was applied to DXA scan of human vertebrae, a good correlation was found with T-score, in patients presenting T-score values lower than -3.0 and high values of BSI. Thus, high BSI values are associated with lower BMD values [10]. Finally, in recent clinical studies, BSI appeared to be useful to identify the osteoporotic patients’ subgroup particularly prone to fragility fractures [13], and to characterise young patients affected by secondary osteoporosis [14, 15].
Bone densitometry precision is one of the most important factors in clinical practice, especially for patient’s monitoring. Precision of DXA-related measurements such as BMD and TBS has been widely assessed [16,17,18,19]. Currently, no data are available about BSI precision. Thus, the aim of this study was to evaluate the reproducibility of BSI measurements on a phantom and to compare it with BMD reproducibility.
Methods
This phantom study was carried out at the IRCCS Istituto Ortopedico Galeazzi of Milan, Italy, in 2017–2018. For the in vitro study, the Institutional Review Board approval was not requested, because no patients were involved.
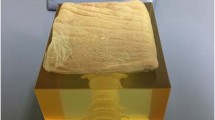
A spine phantom (Model DPA/QDR-1, S/N: 13129, fan beam BMD = 0.985 g/cm2) provided by Hologic (Hologic Inc, Marlborough, Massachusetts, USA) for daily quality control was used. All measurements were performed using a QDR-Discovery W densitometer, software version n. 13.6.0.2 able to perform exams with three different scan modes: fast array (FA), array (A), and high definition (HD). To reproduce the human soft tissues, 5-mm layers of fresh pork rind were interposed as a surrogate of subcutaneous and visceral abdominal fat, given its high lipids’ content (80%). For each scan mode, the phantom was consecutively scanned 25 times without repositioning, with the specific purpose to test the best reproducibility for the software. The set of the three scan modes was performed without any layer of pork rind and then with layers creating an increasing thickness of 1 cm, 3 cm, and 6 cm. Thus, a total of 300 acquisitions (3 modes x 25 scans x 4 different pork rind thicknesses) were acquired. The region of interest (ROI) of the first scan was automatically set by the computer. At this stage, the operator could make image corrections if needed, for example in case of phantom ROI contour inaccuracies or intervertebral lines misplacement. After delineating the first ROI, the software automatically used it for the following acquisitions, thus avoiding any variability due to manual correction. Once DXA analysis was completed, data were obtained from the same ROI used for phantom BMD. For each scan, a standard measure of 190 cm and 80 kg was used in order to reproduce the same normal human body mass index (BMI) value of 22 kg/m2 for all acquisitions.
Statistical analysis
Normality of the data was assessed using Shapiro-Wilk test. Mean ± standard deviation (SD) of BMD and BSI were calculated. Precision was obtained in accordance to the suggestions of the International Society for Clinical Densitometry official positions, and the coefficient of variation (CoV) was calculated as the ratio between standard deviation and mean. Least significant change percentage (LSC%) was calculated as 2.77 × CoV. Reproducibility was calculated as the complement to 100% of LSC% [20].
We first evaluated BMD and BSI mean values differences with increasing thickness and between the three scan modes using one-way analysis of variance (ANOVA) with Tukey post-hoc test, after verification of variance homogeneity according to Levene test. As the BSI HD subset showed variance in homogeneity, we used the Welch ANOVA with the Games-Howell post-hoc test. The comparison between BMD and BSI reproducibility at different thicknesses was performed by calculating the SD distribution of all measurements. The resulting distributions were again tested using one-way ANOVA. A p value lower than 0.05 was considered statistically significant.
Results
The general overview of the results is reported in Table 1, with a direct comparison of BMD and BSI reproducibility for each modality with different thicknesses of interposed soft tissue. In general, without soft tissue superimposition, the LSC% of BSI was about three times higher than that of BMD, with the greatest difference for A-mode and FA-mode. This difference was somewhat lower at increasing thickness, with BSI LSC reaching the lowest value of 1.7% with 1 cm thickness of interposed soft tissue using HD-mode (versus BMD LSC = 0.7%). Overall, the reproducibility of BSI was lower compared to that of BMD.
Table 2 shows a direct comparison between BMD and BSI reproducibility values with different thicknesses of interposed soft tissue using the three modalities. Regarding BMD, the highest reproducibility was 99.4% (0 cm soft tissue thickness, HD-mode), while the lowest was 98.4% (6 cm soft tissue thickness, HD-mode). For BMD, the increase in soft tissue thickness was associated with a decrease in reproducibility, which showed to be significant only for HD-mode (p < 0.001). On the other hand, the highest value of BSI reproducibility was 98.3% (1-cm soft tissue thickness, HD-mode), whereas the lowest was 96.1% (6 cm soft tissue thickness, HD-mode).
Table 3 shows the comparisons between the mean values of BMD and BSI at 0 cm and 6 cm soft tissue thickness for each scan mode. There was a significant increase in BMD values in each scan mode, with the highest difference of 1.46% for HD-mode and the lowest difference of 0.76% for FA-mode. Differently from BMD, BSI values significantly decreased from 0 to 6 cm soft tissue thickness in all scan modes, and the variation was more pronounced than for BMD. In fact, the highest negative variation was 1.57% for FA-mode, while the lowest negative variation was 1.03% in A-mode.
Discussion
This is the first study in which the reproducibility of BSI is tested on a phantom, showing that this new software has higher CoV and LSC% compared to BMD, being about two to three times higher. As a consequence, BSI reproducibility was lower than that of BMD, and it ranged from 96.1% (6 cm soft tissue thickness, HD-mode) to 98.3% (1 cm soft tissue thickness, HD-mode). BMD reproducibility confirmed to be very good, but was affected by the increase of soft tissue thickness.
This is not the first phantom study aimed to evaluate the reproducibility of DXA measurements. The important aspect of these studies relies on the fact that phantoms are usually less affected by external factors, and this represents a methodological advantage to better understand the working principle of new techniques, such as the BSI. Previous studies have been published with data regarding BMD and TBS reproducibility [16,17,18, 21]. Concerning TBS, phantom studies showed that its reproducibility is somewhat lower compared to that of BMD, being between 96.4–98.3% [21] and 97.7–98.3% [18]. Usually, BMD reproducibility is known to be very good and typically represents the standard of reference for other DXA-based measurements. This was confirmed by our study, as BMD showed high values of reproducibility being around 99% in all the three scan modalities. On the other hand, the reproducibility of BSI was lower than that of BMD, and this finding has implication in clinical practice especially for patient’s monitoring. From a clinical point of view, the lower is the reproducibility the longer has to be the time of follow-up to observe a clinically significant variation.
From a practical point of view, the increase in soft tissue thickness is a condition that is frequently found in clinical DXA routine, in patients with high values of BMI and waist circumference. In our study, we tried to understand the behaviour of this new technology by simulating this frequent clinical scenario, showing that BSI, despite having lower reproducibility, was equally affected as BMD. The increase in soft tissue thickness was associated to a reduction of precision, but this was statistically significant for both BMD and BSI only for the HD-mode. Thus, we found a detrimental effect of increasing soft tissue on BSI reproducibility, similar to that of BMD.
When considering BMD and BSI mean values difference between 0 and 6 cm, we notice again a similar behaviour of these two parameters, as a statistically significant variation was found for both for BMD and BSI, despite the first increased its value and the latter showed a decrease. This divergence is expected, as higher BSI values are associated to lower BMD values and vice versa. Nevertheless, the amplitude of variation between 0 and 6 cm was slightly higher for BSI compared to BMD, a difference that was more evident for the FA-mode.
This study presents some limitations. The first one is that we evaluated BSI reproducibility on a phantom that was designed for BMD quality control. Thus, the intrinsic value of BSI measurement may not be directly transferred to clinical practice, despite the evaluation of reproducibility remains independent from BSI significance. Another limitation is that we performed this study on a single phantom with a single densitometer. Thus, these results may present variations when applied to other settings, and the precision of this software may vary when a different phantom or densitometer is used, and of course, the precision may vary among patients with different degrees of bone quality. Lastly, we simulated fat tissue using a material (pork rind) which is similar but not equal to human fat; therefore, we may not directly apply these results to real BMI variations.
In conclusion, this phantom study assessed the reproducibility of BSI compared to that of BMD in different scan modes and interposed fat thicknesses, showing that BSI reproducibility was overall lower than that of BMD and only slightly negatively influenced by interposed fat thickness increase respect to BMD.
Abbreviations
- A:
-
Array
- BMD:
-
Bone mineral density
- BSI:
-
Bone strain index
- CoV:
-
Coefficient of variation
- DXA:
-
Dual x-ray photon absorptiometry
- FA:
-
Fast array
- FEM:
-
Finite element method
- HD:
-
High definition
- LSC%:
-
Least significant change percentage
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- TBS:
-
Trabecular bone score
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795. https://doi.org/10.1001/jama.285.6.785
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44. https://doi.org/10.1007/s00198-018-4704-5
Lindsay R, Silverman SL, Cooper C et al (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323. https://doi.org/10.1001/jama.285.3.320
Compston J, Cooper A, Cooper C et al (2017) UK clinical guidelines for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43. https://doi.org/10.1007/s11657-017-0324-5
Messina C, Sconfienza LM, Bandirali M, Guglielmi G, Ulivieri FM (2016) Adult dual-energy x-ray absorptiometry in clinical practice: how I report it. Semin Musculoskelet Radiol 20:246–253. https://doi.org/10.1055/s-0036-1592370
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194. https://doi.org/10.1359/JBMR.050304
Hans D, Barthe N, Boutroy S, Pothuaud L, Winzenrieth R, Krieg MA (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy x-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14:302–312. https://doi.org/10.1016/j.jocd.2011.05.005
Brandi ML (2009) Microarchitecture, the key to bone quality. Rheumatology (Oxford) 4:iv3–iv8. https://doi.org/10.1093/rheumatology/kep273
Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD (2015) Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions Part 2: Trabecular Bone Score. J Clin Densitom 18:309–330. https://doi.org/10.1016/j.jocd.2015.06.008
Tecnologie avanzate (website). https://tecnologie-avanzate.com/ricerca-e-sviluppo/bone-strain-index/. Accessed 3 June 2019
Choisne J, Valiadis JM, Travert C, Kolta S, Roux C, Skalli W (2018) Vertebral strength prediction from Bi-planar dual energy x-ray absorptiometry under anterior compressive force using a finite element model: an in vitro study. J Mech Behav Biomed Mater 87:190–196. https://doi.org/10.1016/j.jmbbm.2018.07.026
Khennane A (2013) Introduction to finite element analysis using MATLAB and Abaqus. CRC Press, Taylor & Francis Group, Boca Raton FL, USA. https://mihanbana.com/dl/matlab-Abaqus-mihanbana.com.pdf
Ulivieri FM, Piodi LP, Grossi E et al (2018) The role of carboxy-terminal cross-linking telopeptide of type I collagen, dual x-ray absorptiometry bone strain and Romberg test in a new osteoporotic fracture risk evaluation: a proposal from an observational study. PLoS One 13:e0190477. https://doi.org/10.1371/journal.pone.0190477
Ulivieri FM, Rebagliati GAA, Piodi LP et al (2018) Usefulness of bone microarchitectural and geometric DXA-derived parameters in haemophilic patients. Haemophilia 24:980–987. https://doi.org/10.1111/hae.13611
Rodari G, Scuvera G, Ulivieri FM et al (2018) Progressive bone impairment with age and pubertal development in neurofibromatosis type I. Arch Osteoporos 13:93. https://doi.org/10.1007/s11657-018-0507-8
Bandirali M, Di Leo G, Messina C et al (2014) Reproducibility of trabecular bone score with different scan modes using dual-energy x-ray absorptiometry: a phantom study. Skeletal Radiol 44:573–576. https://doi.org/10.1007/s00256-014-1980-9
Messina C, Poloni A, Chianca V et al (2018) Increasing soft tissue thickness does not affect trabecular bone score reproducibility: a phantom study. Endocrine 61:336–342. https://doi.org/10.1007/s12020-018-1647-8
Bandirali M, Poloni A, Sconfienza LM et al (2015) Short-term precision assessment of trabecular bone score and bone mineral density using dual-energy x-ray absorptiometry with different scan modes: an in vivo study. Eur Radiol 25:2194–2198. https://doi.org/10.1007/s00330-015-3606-6
Delnevo A, Bandirali M, Di Leo G et al (2013) Differences among array, fast array, and high-definition scan modes in bone mineral density measurement at dual-energy x-ray absorptiometry on a phantom. Clin Radiol 68:616–619. https://doi.org/10.1016/j.crad.2012.11.017
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom 16:455–466. https://doi.org/10.1016/j.jocd.2013.08.00421
Amnuaywattakorn S, Sritara C, Utamakul C et al (2016) Simulated increased soft tissue thickness artefactually decreases trabecular bone score: a phantom study. BMC Musculoskelet Disord 17:17. https://doi.org/10.1186/s12891-016-0886-1
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, FMU, upon reasonable request.
Funding
This study was not supported by any funding.
Authors’ contributions
CM, LPP, LMS, and FMU contributed to the design and the implementation of the research and wrote the manuscript. CM contributed also to the statistical analysis of the results. LR contributed to scientific technical-mathematical advice. IE and FP contributed to the implementation of the data. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Consent and ethical committee’s approval were not applicable due to the nature of the study, because no patients were involved and the work responds to clinical good practice criteria.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. LR receives salary from TECHNOLOGIC S.r.l. as an employee. TECHNOLOGIC S.r.l. did not have any role in the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Messina, C., Piodi, L.P., Rinaudo, L. et al. Bone strain index reproducibility and soft tissue thickness influence: a dual x-ray photon absorptiometry phantom study. Eur Radiol Exp 3, 33 (2019). https://doi.org/10.1186/s41747-019-0110-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41747-019-0110-9