Abstract
Vaccines that autonomously transfer among individuals have been proposed as a strategy to control infectious diseases within inaccessible wildlife populations. However, rates of vaccine spread and epidemiological efficacy in real-world systems remain elusive. Here, we investigate whether topical vaccines that transfer among individuals through social contacts can control vampire bat rabies—a medically and economically important zoonosis in Latin America. Field experiments in three Peruvian bat colonies, which used fluorescent biomarkers as a proxy for the bat-to-bat transfer and ingestion of an oral vaccine, revealed that vaccine transfer would increase population-level immunity up to 2.6 times beyond the same effort using conventional, non-spreadable vaccines. Mathematical models showed that observed levels of vaccine transfer would reduce the probability, size and duration of rabies outbreaks, even at low but realistically achievable levels of vaccine application. Models further predicted that existing vaccines provide substantial advantages over culling bats—the policy currently implemented in North, Central and South America. Linking field studies with biomarkers to mathematical models can inform how spreadable vaccines may combat pathogens of health and conservation concern before costly investments in vaccine design and testing.
Similar content being viewed by others
Main
Infectious diseases of wildlife cause threats to human and animal health globally1. Controlling these pathogens within their natural animal hosts can offer substantial health, economic and conservation benefits. For example, baited vaccines targeting wildlife reservoirs eliminated fox rabies from western Europe2 and currently confine raccoon rabies to the eastern United States3. However, for many important wildlife diseases, delivery systems to vaccinate a sufficient proportion of host populations to control pathogens are unavailable, and direct (that is, individual-based) vaccination is logistically prohibitive. Interventions that spread from treated to untreated individuals are increasingly used to control arthropod-borne diseases4,5,6 and have been proposed as a solution for the mass vaccination of wildlife, since each unit of vaccine deployed would immunize multiple individuals7,8. However, as was seen with poliovirus eradication efforts, vaccines that sustain transmission may revert to virulent phenotypes9, and in wildlife, vaccine shedding may have unanticipated ecological or evolutionary impacts on competing pathogens or host species10. Vaccines with deliberately constrained capacity to transmit are therefore currently the preferred candidates for real-world applications. Encouragingly, theoretical models suggest that such weakly transmissible vaccines consistently outperform individual-based vaccination, increasing the potential for disease eradication11. Despite this theoretical promise, spreadable vaccines have only rarely been tested in natural systems (namely, rabbit haemorrhagic disease and myxoma virus in rabbits12). This gap between theory and practice reflects a number of limiting factors: vaccines may be unavailable; epidemiological knowledge of the target pathogen or the dynamics of vaccine spread may be insufficient to guide deployment or predict benefits; and losses incurred under existing management strategies may be considered insufficient to warrant the real or perceived risks of novel interventions.
Vampire bat rabies (VBR)—a universally lethal viral zoonosis found throughout Latin America—represents a tractable system with which to explore the implementation of spreadable vaccines to protect human and animal health. Where common vampire bats (Desmodus rotundus) routinely feed on human blood, VBR is estimated to cause up to 960 deaths per 100,000 people13. Losses from livestock mortality exceed US$50 million annually and disproportionately affect impoverished, rural communities14,15. Existing management strategies have been unable to mitigate the burden of VBR. Vaccines for humans and livestock are protective, but high costs and inaccessibility to remote areas limit uptake16. Rabies control programmes also cull vampire bats using anticoagulant poisons (‘vampiricide’), which are applied in topical gels that spread among bats through social contacts and are ingested during grooming (here, termed ‘orotopical transfer’)17. While culling reduces bat bites on humans and livestock, the effects on rabies transmission remain controversial18,19. Moreover, heightened bat dispersal following culls is predicted to exacerbate VBR transmission by increasing the mixing of bat colonies, analogous to the increased transmission of bovine tuberculosis induced through effects of culling on badger home range size20,21. Oral rabies vaccines that spread by the same orotopical mechanism as vampiricide offer an alternative approach. These recombinant virally vectored vaccines can indirectly immunize untreated bats in captivity, but have never been tested in wild populations22,23,24,25. Several unresolved questions must be answered before deploying vaccines for large-scale bat rabies control: (1) How efficiently would vaccines transfer among wild bats?; (2) Are certain demographic groups of bats especially difficult to vaccinate or especially effective disseminators of vaccines?; (3) Would the resulting degree of immunization significantly reduce rabies transmission?; and (4) Would vaccines reduce human and livestock rabies risk more effectively than the current policy of culling? We address these questions by coupling field studies that used fluorescent biomarkers to quantify contact networks and orotopical transfer among wild vampire bats with mathematical models that simulated how vaccines and vampiricide, which spread by identical mechanisms, would impact the size, duration and probability of rabies outbreaks.
Results
Biomarker transfer and ingestion show potential for high vaccine coverage in wild vampire bats
We estimated the potential for a spreadable vaccine to transfer among bats using rhodamine b (RB)—a biomarker that, when ingested, leads to long-lasting fluorescence in hair follicles in diverse mammalian species26,27,28. After applying a gel formulation of RB topically to bats in three colonies in Peru (colony sizes: 207–257 individuals; sex ratios: 43.1–50.6% male), orotopical transfer and ingestion were monitored by fluorescent microscopic analysis of hair samples collected in subsequent capture sessions, with fluorescence indicating RB consumption (Supplementary Table 1). At two sites (LMA5 and LMA6), an estimated 84 and 92% of bats, respectively, ingested RB, either following topical application or transfer from treated bats (Fig. 1). The third colony (LMA12) relocated to an undocumented roost soon after RB treatment, which diminished captures during the monitoring period relative to the estimated colony size (Supplementary Table 1). Consequently, the overall estimated coverage dropped to 28.8% (Fig. 1). Nevertheless, the percentage of sampled LMA12 bats at the end of the 1-month monitoring period that were RB positive (48.3%; aggregating days 24 and 25) was not statistically different from the percentages at the final capture dates in the other two colonies (58.3 and 70.0%; chi-squared test, \({\chi }^{2}\) = 3.2; d.f. = 2; P = 0.21). We further characterized patterns of RB uptake among demographic groups of bats. The sex ratios of transfer-positive bats became slightly more male biased (3–11% increases, depending on the colony) relative to the sex ratios of bats that were treated with RB, suggesting elevated transfer to males; however, these increases were not statistically significant (\({\chi }^{2}\) tests; all P > 0.05; Supplementary Fig. 1). We observed RB transfer to untreated bats in all three age classes. Across all colonies, 73.4% of sampled adults (\(\overline{n}\) = 351, averaged across microscopy readings of independent observers), 57.5% of sampled juveniles (\(\overline{n}\) = 30.5) and 89.9% of sampled subadults (\(\overline{n}\) = 34.5) became RB positive through transfer during the monitoring period. Consequently, these results implied that vaccines deployed over only 2 d of captures (17–50% of the total colony size) would yield high levels of population immunity across age classes due to orotopical transfer.
a–c, Transfer and ingestion data for the gel biomarker are shown for LMA5 (a), LMA6 (b) and LMA12 (c). Days on the x axes show the time since RB application, with the number of transfer-positive bats over total captures marked underneath. The y axes show the numbers of bats in each colony within three categories: RB negative (white); application positive (black); and transfer positive (grey). Asterisks on and after day 10 in c indicate captures from the relocated roost. Data are the means of microscopy readings from two observers, except where noted otherwise. Transfer-positive bats from day 2 had RB applied and were included in the black bar to visualize the total force of application, but were included as transfers in the statistical analyses.
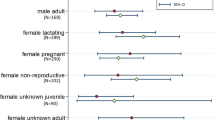
Contact heterogeneities among demographic groups of vampire bats
Next, we examined whether contact heterogeneities might make certain demographic groups of bats especially effective or ineffective spreaders of vaccines using ultraviolet powder marking, wherein different age and sex groups of bats were treated with different colours of ultraviolet powder, and transfer to untreated bats was monitored over two subsequent capture nights29,30. Across three replicate ultraviolet treatments per colony, we documented 78 instances of ultraviolet powder transfer, leading to estimated contact rates ranging from 0.23–1.25 per treated bat (Fig. 2). Male bats had significantly higher contact rates than female bats (Wilcoxon rank-sum test, W = 91; P = 0.025; mean = 1.14 versus 0.67) and had similar rates of male-to-male and male-to-female contacts (Wilcoxon rank-sum test, W = 42; P = 0.93). In contrast, females preferentially contacted other females (Fig. 2a). Transfer to juveniles could not be reliably quantified because these bats were mostly too young to forage independently, and our capture method during the monitoring period required bats to fly out of their roosts. Nevertheless, a single captured juvenile bat had ultraviolet transfer from a female. In contrast, transfer from juveniles to adults should have been detectable if it occurred due to the greater ease of capturing adults. However, none of the 27 marked juveniles transferred ultraviolet powder to adults. Together with the high observed rates of juvenile exposure to RB, these findings suggest that vaccine deployments should target adults rather than juveniles. Targeting adults would further be logistically advantageous since it would minimize the social disruption of colonies that results from entering roosts to capture juveniles.
a, Mean new contacts per marked bat, by sex. Arrow thicknesses are proportional to contact rates. b, Number and directionality of contacts by sex, location and sampling date. Contacts to juveniles are not shown since the juveniles in the studied colonies were too young to feed independently and would have been underestimated by our capture method during monitoring.
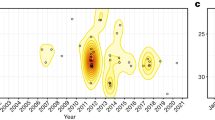
Epidemiological models show that spreadable vaccines outperform culling for rabies control
We adapted a deterministic compartmental model of VBR persistence20 to incorporate an orotopically spread vaccine, and used least squares (Fig. 3b) to estimate the expected per-capita vaccine transfer rates from the time series of RB transfers observed in our field studies, assuming that RB transfer equated to lifelong protection. This analysis revealed that each treated bat transferred RB to 1.45–2.11 untreated individuals—up to a 2.6-fold increase in population-level coverage relative to the coverage that would be expected using conventional, non-spreading vaccines (Fig. 4b, Supplementary Fig. 2 and Supplementary Table 2). We simulated the ability of spreadable vaccines to control rabies across the range of \({R}_{0}\) (the expected number of secondary infections arising from a single viral introduction into a completely susceptible population) values (0.6–2.0) suggested in the rabies literature20,31,32. Applying vaccines to approximately 20% of bats vaccinated 40% of the population and reduced rabies outbreak size by 45–75%, depending on the assumed \({R}_{0}\) of rabies (Fig. 4a–c). However, applying vaccines to a higher proportion of bats had diminishing returns for both the proportion of the colony that was ultimately protected and for rabies control. If vaccines were applied to >30% of bats, additional reductions in rabies outbreak sizes were <5%, meaning that a 5% increase in initial application led to a <5% reduction in outbreak sizes (Fig. 4d). The greatest benefit (reduction in outbreak size relative to effort) occurred at vaccination levels <15%.
a, The full model used for the outbreak analyses included orotopical transfer and rabies transmission. Classes comprised susceptible (S), application-positive (A), transfer-positive (T), immune (I), exposed to rabies (E) and rabid bats (R). b, Biomarker transfer model structure for fitting β. In the vaccination model, the I and T classes both provide immunity from rabies, but the T class has permanent immunity. Model parameters describe the rates of: natural births (η) and deaths (ω); orotopical gel application (α), persistence (ψ) and transfer (β); rabies transmission (θ); waning of immunity (ϕ); rabies-induced mortality (τ); and the probabilities of succumbing to rabies (δ) or surviving (λ) following exposure. Supplementary Table 3 provides further details and references for parameter values.
a, Mean rabies outbreak sizes after the introduction of a single rabid bat to the colony 1 week following the application of a spreadable vaccine. Colours represent varying degrees of rabies \({R}_{0}\), with 95% confidence intervals (shading) calculated from 5,000 simulations. Dashed lines indicate the percentage of bats that RB was applied to at our study sites. Supplementary Fig. 5 shows the results calculated only from simulations where outbreaks occurred. b, Percentage of bats ultimately protected by initial vaccine application. Circle sizes indicate outbreak sizes for the three rabies \({R}_{0}\) values. The solid line represents x = y. Points above the line represent the added benefit of vaccine transfer. c, Reduction in rabies outbreak size (% fewer cases) for varying initial vaccination levels and rabies \({R}_{0}\) values. d, Percentage of additional rabies cases prevented by increasing the initial vaccine application effort by 5% (that is, the rate of change in rabies reduction from c).
Next, we compared the relative efficacy of vaccination and culling across three epidemiological scenarios representing different management strategies: (1) a preventative approach, where vaccine/vampiricide was applied to prevent VBR invasion into historically rabies-free bat populations33,34; (2) a proactive approach, which represented an intervention in a VBR endemic area, but in a colony that was not currently infected; and (3) a reactive approach where intervention followed 60 d after a single VBR-infected bat was introduced to the colony (Supplementary Fig. 4). Although we simulated outcomes across the full possible range of application efforts (that is, 0–100% of bats treated), we focused on lower application levels since capturing large proportions of bats across large geographic areas would be impractical for rabies control campaigns. Indeed, mark–recapture studies across multiple vampire bat colonies in Peru suggested that, on average, <10% of colonies were captured in a single night19. At realistic levels of application, vaccination consistently reduced the probability of viral invasion, outbreak size and outbreak duration more effectively than culling, regardless of whether control measures were preventative, proactive or reactive (Fig. 5). Culling was only favoured when at least 25% of the colony was treated, and only in reactive scenarios. However, the advantage of culling on outbreak size was relatively small (a maximum of a 20% greater reduction) relative to the larger advantages observed when vaccination was favoured (up to 45% greater reduction), and differences in outbreak duration were negligible until much larger proportions of bats were culled (Fig. 5). For the preventative and proactive scenarios, culling required the capture and treatment of much larger proportions of vampire bat populations (for example, >60%) to match the reduction in outbreak size and duration achieved by vaccination (Fig. 5). In fact, the only discernible difference at higher application levels was a greater reduction in the duration of outbreaks by culling; however, this was due to near-complete extinction of bat colonies. Even if this degree of bat culling were achievable and ethically acceptable, it may not be a favourable long-term strategy since populations that recovered from culls would be entirely susceptible to rabies, potentially causing larger future outbreaks35.
a–h, Difference in the reduction of rabies cases between equal levels of effort in vaccination versus culling (a, d and g), probability of a rabies outbreak (b and e) and duration of rabies outbreaks following vaccination and culling (c, f and h) for the preventative (a–c), proactive (d–f) and reactive (g and h) strategies. In a, d and g, values above and below 0 favour vaccination and culling, respectively. In b and e, the probability of a rabies outbreak is defined as the percentage of simulations (n = 5,000) where VBR virus introduction led to onward transmission, and shaded regions represent the difference between vaccination (circles) and culling (triangles); culling is favoured in the grey regions and vaccination is favoured in the blue, green and red regions. The probability of outbreaks was not modelled for reactive control since, by definition, outbreaks had already occurred. The horizontal line in h indicates day 60, when reactive control measures were implemented. In all panels, colours correspond to different assumed \({R}_{0}\) values for rabies.
Our per-capita transfer rates probably represent lower bounds of vaccine and vampiricide spread, since the relatively high percentage of bats initially treated with RB left few others available to be exposed via transfer in two of our colonies, and relocation of the third colony reduced capture rates during the monitoring period. Indeed, some studies have suggested higher transfer rates of vampiricide17,36. Therefore, we conducted a sensitivity analysis in which both vaccines and vampiricide spread up to tenfold more efficiently than in our RB estimates (values that exceeded the largest transfer rates suggested from vampiricide applications). Additionally, we considered transfer rates that were up to 75% less efficient than our RB estimates. This analysis showed that low-level vaccination remained favoured under preventative and proactive approaches even if both the vaccine and vampiricide spread up to threefold greater than was observed in our field studies (Supplementary Figs. 6–8). If both interventions spread less effectively than RB, vaccination was either superior or equivalent to culling, except when large proportions of bat colonies were reactively culled (Supplementary Fig. 6). Under realistic levels of application (application ≤25%), even if vampiricide spread threefold better than a vaccine, it was unable to outperform vaccination under preventative or proactive approaches when \({R}_{0}\) was <2. Under reactive scenarios, culling was favoured if vampiricide spread two- to threefold better than a vaccine or if the VBR \({R}_{0}\) was 2 (Supplementary Fig. 9). Given that existing oral rabies vaccines use replication-competent viral vectors with the potential for lower effective doses than chemical poisons24,25, heightened vampiricide transfer is less likely than the converse where vaccines spread better8. The high \({R}_{0}\) scenarios where culling is favoured are also unlikely, as the estimated VBR \({R}_{0}\) is considerably lower than 2 (ref. 20). Our results therefore support previous suggestions that culling may require near-elimination of bats to locally benefit rabies prevention18, and reveal spreadable vaccines as efficient tools to reduce the size, duration and probability of rabies outbreaks in Latin America.
Discussion
This study provides proof of principle that at operationally achievable levels of deployment and empirically quantified rates of bat-to-bat spread, orotopical vaccines should reduce rabies transmission more effectively than culling (the current policy employed across Latin America). Since VBR persistence requires inter-colony spread for viral dispersal, even modest reductions in outbreak size are likely to have epidemiologically important impacts at the larger geographic scales over which disease control campaigns are implemented. In particular, by reducing the number of infected bats and the probability of viral invasion, vaccination of a limited number of colonies would disproportionately benefit regional rabies elimination by favouring stochastic viral extinctions. Because male dispersal spreads rabies between colonies, vaccination might further benefit from targeting male bats33. Although higher rates of social grooming among females were expected to undermine this strategy36,37, we found that males have equal or greater inter- and intra-sex contact rates—a possible consequence of attempted mating with females or fighting among males. Importantly, because self-grooming is common38, any vaccine transferred through these interactions would ultimately be ingested.
Designing large-scale campaigns to deploy spreadable rabies vaccines requires additional research in several areas. First, to optimize the number of vaccine doses to apply to each bat, captive and field studies should quantify individual heterogeneity in transfer rates using actual vaccines in addition to biomarkers. Second, the costs of vaccination must be estimated in economic terms in addition to the epidemiological assessment provided here. Unfortunately, vaccines are currently produced only for research, and the costs of large-scale production are unavailable. Third, vaccination of vampire bats without population reduction will be unacceptable to some stakeholders since uncontrolled bat depredation sustains exposures to non-rabies pathogens39, and anaemia from bites may reduce livestock productivity independent of rabies40. Given that culling shifts bat populations towards younger, more rabies-susceptible individuals, which could enhance rabies transmission19, future research should develop tools for reproductive suppression as an alternative to culling41. Finally, metapopulation maintenance of rabies provides opportunities for more efficient, epidemiologically informed vaccination42. For example, vaccines might be deployed with previous knowledge of rabies presence from livestock surveillance systems (for example, ring vaccination) or preventatively in areas where the locations and timings of outbreaks are predictable34. Spatially explicit rabies transmission models will be an important next step in the design of these interventions, but will require a more quantitative understanding of bat dispersal than is currently available. Excitingly, once strategies are developed, the operational capacity for their implementation is already available in most Latin American countries as the result of decades of experience with culling campaigns.
These results provide evidence that spreadable vaccines may contribute to pathogen management within wild bats. VBR provided an ideal case study because the epidemiological mechanisms underlying viral maintenance are understood and candidate vaccines are available20,25,34,43. While the exact parameter estimates and models developed here should not be applied directly to other bat pathogens, the framework linking biomarkers to mathematical models can guide future research. For several bat pathogens of public health or conservation concern, such as white nose syndrome, Hendra virus and Marburg virus, epidemiological models have been proposed44,45,46, and vaccines for bats either exist or have precedents encouraging their development47,48,49. In these cases, our approach could be implemented over relatively short timescales to evaluate the prospects for vaccines to aid management and the immunological and epidemiological characteristics that would be required for success before investing resources in vaccine development. For other bat pathogens with greater uncertainty in reservoir hosts and transmission biology, such as ebolaviruses50, implementation will require greater fundamental knowledge of viral transmission cycles. We encourage further development of virally vectored vaccines for bats, and highlight the need to quantify their spread and efficacy in the wild.
Methods
Field studies of biomarker transfer and ingestion
Field studies were carried out between January and July 2017 in three vampire bat roosts in the Barranca (LMA5: 10° 38′ 29.4′′ S, 77° 48′ 57.6′′ W), Huaura (LMA6: 11° 03′ 19.8′′ S, 77° 27′ 33.8′′ W) and Lima (LMA12: 12° 10′ 59.9′′ S 76° 50′ 60′′ W) provinces of the Department of Lima, Peru (Supplementary Table 1). Two roosts (LMA5 and LMA6) had been monitored since 2007, while the third (LMA12) was examined here for the first time19. All roosts were manmade tunnels that formed part of crop irrigation systems. Diurnal captures were carried out to mark the bats and estimate sex ratios and colony sizes. Diurnal captures involved teams entering caves and catching bats with hand nets (BioQuip; Tropics Net). In addition, 2.5-m mist nets (Ecotone) were placed at each end of the tunnels to catch the bats that attempted to escape. Diurnal capture efforts were set to 1 h across sampling dates and localities. Colony sizes were estimated using the Schnabel method51. Nocturnal captures were carried out in the same roosts to monitor biomarker spread. Nets placed at each roost exit were checked every 30 min for 4 h per night at varying hours depending on the lunar cycle. Following removal from mist nets, bats were placed in individual cloth bags until processing. All captured bats were given an individually numbered, four-digit Incoloy wing band (3.5 mm; Porzana) to identify recaptures. Age was classified using the terms juvenile, subadult or adult, based on the degree of fusion of the phylangeal epiphyses52. In total, we recorded 1,777 captures of 709 individually marked bats, with the average bat captured 2.39 times (range = 1–9).
Studies of vaccine transfer and ingestion used RB powder (50 mg) mixed with glycerine jelly (44.5 ml; Carolina Biological Supply Company) and water (55.5 ml) to form a gel. On days 1 and 2, RB was administered orally to confirm fluorescence in RB-treated bats (~0.05 ml via needle-free syringe) and applied topically (around 0.45 ml, rubbed into the dorsal fur) to all captured bats. Uptake in untreated bats was monitored using hair plucked from bats captured over 4–5 subsequent sessions per colony, carried out up to 31 d after initial application (Supplementary Table 1). Hair samples were examined with a Nikon SMZ1270 microscope at 15× using a fluorescence filter with an excitation wavelength of 540 nm and an emission wavelength of 625 nm. Each sample was examined by two individuals to minimize misclassification, except at LMA12 on days 8 and 10, when only one individual examined the hair. The presence of fluorescence in hair was interpreted to indicate the transfer and consumption of RB, but was not considered a quantitative measure of the volume of RB consumption. Because bats had identification tags, we were able to distinguish those that were positive due to transfer from RB-treated bats (that is, transfer positives) from those that had RB applied by experimenters (that is, application positives). Hair samples were collected under the Peruvian collection permit 028-2017-SERFOR/DGGSPFFS and exported to the United States under export permit 3235-SERFOR. This research was performed with the approval of the University of Glasgow School of Veterinary Medicine Animal Ethics Committee (project 25A/18).
Contact heterogeneities among demographic groups of vampire bats
Powder marking was replicated three times per colony (for a total of nine marking sessions) and bats were monitored for two nights following each marking session (Supplementary Table 1). During each session, red, green, blue or orange ultraviolet powder (DayGlo) was rubbed into the fur of the bat across the entire body using a toothbrush, with colours dependent on age and sex. Ultraviolet colours were rotated between groups for different capture dates to control for potential differences in detection probability. Ultraviolet powder markings were recorded by examining each captured bat for 30 s using handheld ultraviolet lights (Glowtech) before removal from mist nets. After removing ultraviolet-marked bats from the recaptures, directional contact rates for each sex (for example, female-to-male contacts per marked female) were calculated using equation (1):
where \({n}_{{\rm{pos}}_{X}}\) is the number of bats of a certain sex testing positive for the ultraviolet colour in question, \({\rm{UM}}_{X}\) is the number of unmarked bats of that sex captured at this time point, \({n}_{{\rm{UM}}_{X}}\) is the number of unmarked bats of that sex in the entire colony, and \({M}_{X}\) is the number of initially marked bats from that sex. Example calculations are provided in the Supplementary Information (equations (2) and (3)).
Sex biases in ultraviolet transfer were tested by comparing all estimated rates from males with all estimated rates from females, treating each site, month and recipient sex combination as independent observations (n = 36). We used a non-parametric Wilcoxon rank-sum test since rates were not normally distributed, even after log transformation (Shapiro–Wilk test, P = 0.01).
Parameter estimation and mathematical modelling
Per-capita rates of orotopical transfer and ingestion, defined as the estimated number of bat-to-bat transfers per treated individual, were estimated using the data from our RB field study. Specifically, we incorporated a susceptible (S), application-positive (A) and transfer-positive (T) deterministic compartmental model (Fig. 3b) using least-squares methods in the statistical software R. A 2-d transfer period was integrated with the number of RB application and transfer positives across time to estimate the expected transfer rate of orotopical vaccines or poisons (β). A 6-d RB transfer period was also considered to examine variation in β across time (Supplementary Table 2 and Supplementary Information). We assumed that successful transfer led to death in the culling models and lifelong protection against VBR in the vaccination models (~3.5 years of protection given the lifespan of D. rotundus; Supplementary Table 3). Importantly, waning of vaccine-induced immunity would not alter the results shown here, which focused on single outbreaks.
Mathematical models of rabies control used a stochastic model that simulated both rabies transmission and vaccine transfer. A susceptible (S), application-positive (A), transfer-positive (T), exposed to rabies (E), immune (I) and rabid (R) model, with a daily time step, was simulated for 5,000 iterations using a Gillespie algorithm (Fig. 3a and Supplementary Information). Following previous models of VBR20, and consistent with the absence of strong relationships between colony size and rabies seroprevalence19, we utilized a frequency-dependent rabies transmission function. We used 237 bats as the colony size (the mean size from our three field sites). The base model without vaccination or culling followed the mathematical structure and parameter values used by Blackwood et al.20, with the simplifications of a single infectious class and modelling of a single introduction of rabies rather than sustained introductions via immigration. This model generated similar outbreak dynamics to the Blackwood et al.20 model, characterized by short-lived outbreaks (<1 year) followed by viral extinction, persistence of the bat population, and seroprevalence levels consistent with field observations, particularly at values of \({R}_{0}\) > 0.6 (Supplementary Fig. 3). Since we modelled our vaccine spread on a recombinant raccoonpox virus-vectored vaccine that appears unlikely to spread via an infectious process (that is, from indirectly vaccinated bats)43, vaccines were modelled to spread only from those bats to which the vaccine was applied, creating a single generation of transmission. Based on the very low prevalence of rabies in free-flying bats (<1%) and infrequent dispersal in vampire bats53,54, we simulated the introduction of a single rabid bat to the population. Given that sex differences in RB transfer were non-significant, and age-biased transfer was difficult to quantify due to small sample sizes in non-adult classes, we opted against more complex age- and sex-structured models of rabies and vaccine/vampiricide spread.
Models comparing the efficacies of vampiricide and vaccination used the same model structure with the exception that bats in the exposed class died from ingesting vampiricide, while those that consumed the vaccine were not protected (see equations (8) and (9) in the Supplementary Information). This was because post-exposure vaccination has not been evaluated in bats. We generally assumed equal transfer rates of vaccines and vampiricide based on their identical mechanism of transfer; however, we relaxed this assumption in the Supplementary Information (Supplementary Fig. 9). We also assumed that both spread over relatively short time periods, since vampire bats are exceptional groomers and would quickly ingest vaccine or vampiricide38. Importantly, our focal vaccine remains viable over these timescales55. After 2 years (730 d), the cumulative number of newly infected bats was considered to be the outbreak size. Outbreak duration was defined as the total number of days when at least one bat was in the exposed class. For preventative and proactive approaches, we quantified the probability of an outbreak as the proportion of simulations in which at least one new bat became infected after a single rabid bat was introduced.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Source data for Figs. 1 and 2 are provided with this Article at https://doi.org/10.1038/s41559-019-1032-x. The complete dataset describing ultraviolet and RB transfer is available from Dryad (https://doi.org/10.5061/dryad.64t161m).
Code availability
References
Daszak, P., Cunningham, A. A. & Hyatt, A. D. Emerging infectious diseases of wildlife—threats to biodiversity and human health. Science 287, 443–449 (2000).
Brochier, B. et al. Large-scale eradication of rabies using recombinant vaccinia-rabies vaccine. Nature 354, 520–522 (1991).
Slate, D. et al. Oral rabies vaccination in North America: opportunities, complexities, and challenges. PLoS Negl. Trop. Dis. 3, e549 (2009).
Hoffmann, A. et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature 476, 454–457 (2011).
Sinkins, S. P. & Gould, F. Gene drive systems for insect disease vectors. Nat. Rev. Genet. 7, 427–435 (2006).
Aliota, M. T., Peinado, S. A., Velez, I. D. & Osorio, J. E. The wMel strain of Wolbachia reduces transmission of Zika virus by Aedes aegypti. Sci. Rep. 6, 28792 (2016).
Basinski, A. J. et al. Evaluating the promise of recombinant transmissible vaccines. Vaccine 36, 675–682 (2018).
Bull, J. J., Smithson, M. W. & Nuismer, S. L. Transmissible viral vaccines. Trends Microbiol. 26, 6–15 (2018).
Minor, P. Vaccine-derived poliovirus (VDPV): impact on poliomyelitis eradication. Vaccine 27, 2649–2652 (2009).
Behdenna, A. et al. Transmission ecology of canine parvovirus in a multi-host, multi-pathogen system. Proc. R. Soc. B Biol. Sci. 286, 20182772 (2019).
Nuismer, S. L. et al. Eradicating infectious disease using weakly transmissible vaccines. Proc. R. Soc. Lond. B Biol. Sci. 283, 20161903 (2016).
Torres, J. M. et al. First field trial of a transmissible recombinant vaccine against myxomatosis and rabbit hemorrhagic disease. Vaccine 19, 4536–4543 (2001).
Schneider, M. C. et al. Potential force of infection of human rabies transmitted by vampire bats in the Amazonian region of Brazil. Am. J. Trop. Med. Hyg. 55, 680–684 (1996).
Belotto, A., Leanes, L. F., Schneider, M. C., Tamayp, H. & Correa, E. Overview of rabies in the Americas. Virus Res. 111, 5–12 (2005).
Benavides, J. A., Paniagua, E. R., Hampson, K., Valderrama, W. & Streicker, D. G. Quantifying the burden of vampire bat rabies in Peruvian livestock. PLoS Negl. Trop. Dis. 11, e0006105 (2017).
Schneider, M. C. et al. Rabies transmitted by vampire bats to humans: an emerging zoonotic disease in Latin America? Rev. Panam. Salud Públ. 25, 260–269 (2009).
Linhart, S. B., FloresCrespo, R. & Mitchell, G. C. Control of vampire bats by topical application of an anticoagulant, chlorophacinone. Bol. OSP 6, 31–38 (1972).
Fornes, A. et al. Control of bovine rabies through vampire bat control. J. Wildl. Dis. 10, 310–316 (1974).
Streicker, D. G. et al. Ecological and anthropogenic drivers of rabies exposure in vampire bats: implications for transmission and control. Proc. R. Soc. B Biol. Sci. 279, 3384–3392 (2012).
Blackwood, J. C., Streicker, D. G., Altizer, S. & Rohani, P. Resolving the roles of immunity, pathogenesis, and immigration for rabies persistence in vampire bats. Proc. Natl Acad. Sci. USA 110, 20837–20842 (2013).
Donnelly, C. A. et al. Impact of localized badger culling on tuberculosis incidence in British cattle. Nature 426, 834–837 (2003).
Aguilar-Setién, A. et al. Experimental rabies infection and oral vaccination in vampire bats (Desmodus rotundus). Vaccine 16, 1122–1126 (1998).
Aguilar-Setién, A. et al. Vaccination of vampire bats using recombinant vaccinia-rabies virus. J. Wildl. Dis. 38, 539–544 (2002).
Stading, B. et al. Protection of bats (Eptesicus fuscus) against rabies following topical or oronasal exposure to a recombinant raccoon poxvirus vaccine. PLoS Negl. Trop. Dis. 11, e0005958 (2017).
Almeida, M., Martorelli, L., Aires, C., Barros, R. & Massad, E. Vaccinating the vampire bat Desmodus rotundus against rabies. Virus Res. 137, 275–277 (2008).
Cagnacci, F., Massei, G., Coats, J., DeLeeuw, A. & Cowan, D. P. Long-lasting systemic bait markers for Eurasian badgers. J. Wildl. Dis. 42, 892–896 (2006).
Fry, T. L., Atwood, T. & Dunbar, M. R. Evaluation of rhodamine B as a biomarker for raccoons. Hum. Wildl. Interact. 4, 275–282 (2010).
Fernandez, J. R. R. & Rocke, T. E. Use of rhodamine B as a biomarker for oral plague vaccination of prairie dogs. J. Wildl. Dis. 47, 765–768 (2011).
Clay, C. A., Lehmer, E. M., Previtali, A., St Jeor, S. & Dearing, M. D. Contact heterogeneity in deer mice: implications for Sin Nombre virus transmission. Proc. R. Soc. B Biol. Sci. 276, 1305–1312 (2009).
Hoyt, J. R. et al. Cryptic connections illuminate pathogen transmission within community networks. Nature 563, 710–713 (2018).
Hampson, K. et al. Transmission dynamics and prospects for the elimination of canine rabies. PLoS Biol. 7, e1000053 (2009).
Amengual, B., Bourhy, H., López-Roíg, M. & Serra-Cobo, J. Temporal dynamics of European bat lyssavirus type 1 and survival of Myotis myotis bats in natural colonies. PLoS ONE 2, 0000566 (2007).
Streicker, D. G. et al. Host–pathogen evolutionary signatures reveal dynamics and future invasions of vampire bat rabies. Proc. Natl Acad. Sci. USA 113, 10926–10931 (2016).
Benavides, J. A., Valderrama, W. & Streicker, D. G. Spatial expansions and travelling waves of rabies in vampire bats. Proc. R. Soc. Lond. B Biol. Sci. 283, 20160328 (2016).
Choisy, M. & Rohani, P. Harvesting can increase severity of wildlife disease epidemics. Proc. R. Soc. B Biol. Sci. 273, 2025–2034 (2006).
Gomes, M. N., Uieda, W. & Latorre, M. Influence of sex differences in the same colony for chemical control of vampire Desmodus rotundus (Phyllostomidae) populations in the state of Sao Paulo, Brazil. Pesqui. Vet. Bras. 26, 38–43 (2006).
Wilkinson, G. S. Social grooming in the common vampire bat, Desmodus rotundus. Anim. Behav. 34, 1880–1889 (1986).
Carter, G. & Leffer, L. Social grooming in bats: are vampire bats exceptional? PLoS ONE 10, e0138430 (2015).
Bergner, L. M. et al. Using noninvasive metagenomics to characterize viral communities from wildlife. Mol. Ecol. Res. 19, 128–143 (2019).
Thompson, R. D., Elias, D. J. & Mitchell, G. C. Effects of vampire bat control on bovine milk production. J. Wildl. Manage. 41, 736–739 (1977).
Hardy, C. et al. Biological control of vertebrate pests using virally vectored immunocontraception. J. Reprod. Immunol. 71, 102–111 (2006).
Beyer, H. L. et al. The implications of metapopulation dynamics on the design of vaccination campaigns. Vaccine 30, 1014–1022 (2012).
Stading, B. R. et al. Infectivity of attenuated poxvirus vaccine vectors and immunogenicity of a raccoonpox vectored rabies vaccine in the Brazilian free-tailed bat (Tadarida brasiliensis). Vaccine 34, 5352–5358 (2016).
Langwig, K. E. et al. Resistance in persisting bat populations after white-nose syndrome invasion. Phil. Trans. R. Soc. B Biol. Sci. 372, 20160044 (2017).
Plowright, R. K. et al. Urban habituation, ecological connectivity and epidemic dampening: the emergence of Hendra virus from flying foxes (Pteropus spp.). Proc. R. Soc. B Biol. Sci. 278, 3703–3712 (2011).
Hayman, D. T. Biannual birth pulses allow filoviruses to persist in bat populations. Proc. R. Soc. B Biol. Sci. 282, 20142591 (2015).
Rocke, T. E. et al. Virally-vectored vaccine candidates against white-nose syndrome induce anti-fungal immune response in little brown bats (Myotis lucifugus). Sci. Rep. 9, 6788 (2019).
Marzi, A. et al. Cytomegalovirus-based vaccine expressing Ebola virus glycoprotein protects nonhuman primates from Ebola virus infection. Sci. Rep. 6, 21674 (2016).
Pallister, J. et al. A recombinant Hendra virus G glycoprotein-based subunit vaccine protects ferrets from lethal Hendra virus challenge. Vaccine 29, 5623–5630 (2011).
Olival, K. & Hayman, D. Filoviruses in bats: current knowledge and future directions. Viruses 6, 1759–1788 (2014).
Schnabel, Z. E. The estimation of total fish population of a lake. Am. Math. Monthly 45, 348–352 (1938).
Anthony, E. L. P. in Ecological and Behavioral Methods for the Study of Bats (ed. Kunz, T. H.) 47–58 (Smithsonian Institution Press, 1988).
Constantine, D. G., Tierkel, E. S., Kleckner, M. D. & Hawkins, D. M. Rabies in New Mexico cavern bats. Public Health Rep. 83, 303–316 (1968).
Delpietro, H., Russo, R., Carter, G., Lord, R. & Delpietro, G. Reproductive seasonality, sex ratio and philopatry in Argentina’s common vampire bats. R. Soc. Open Sci. 4, 160959 (2017).
Stading, B. Development of a Novel Rabies Mosaic Antigen and the Use of Attenuated Poxviruses as Vaccine Vectors in Bats (University of Wisconsin–Madison, 2015).
Acknowledgements
K.M.B. was supported by NIH award F32AI134016, and computational resources were provided by NIH award U01GM110712. D.G.S. was supported by a Sir Henry Dale Fellowship that was jointly funded by the Wellcome Trust and Royal Society (102507/Z/13/Z). Additional funding was provided via a Challenge Grant from the Royal Society to D.G.S., T.E.R., J.E.O., C.S. and N.F. (CH160097). The authors are grateful to D. Walsh, M. Viana and the Streicker Group for comments on earlier versions of this manuscript. Any use of trade, product or firm names does not imply endorsement by the US Government.
Author information
Authors and Affiliations
Contributions
D.G.S., T.E.R. and J.E.O. conceived and designed the experiments. R.C.A., C.T. and J.E.C. performed the experiments. K.M.B. and D.G.S. analysed the data. T.E.R., J.E.O., W.V., C.S. and N.F. contributed materials and/or analysis tools. K.M.B. and D.G.S. wrote the first draft of the paper. All authors contributed revisions.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–9, Tables 1–3, methods and results.
Supplementary Software 1
R script to carry out least-squares estimation of RB transfer rates.
Supplementary Software 2
R script to carry out mathematical modelling.
Source data
Source Data Fig. 1
RB marking and detection histories for wild bats in the field study.
Source Data Fig. 2
Ultraviolet powder marking and detection histories for wild bats in the field study.
Rights and permissions
About this article
Cite this article
Bakker, K.M., Rocke, T.E., Osorio, J.E. et al. Fluorescent biomarkers demonstrate prospects for spreadable vaccines to control disease transmission in wild bats. Nat Ecol Evol 3, 1697–1704 (2019). https://doi.org/10.1038/s41559-019-1032-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41559-019-1032-x
This article is cited by
-
Rabies in a postpandemic world: resilient reservoirs, redoubtable riposte, recurrent roadblocks, and resolute recidivism
Animal Diseases (2023)
-
A review of the diet of the common vampire bat (Desmodus rotundus) in the context of anthropogenic change
Mammalian Biology (2023)
-
Safety and security concerns regarding transmissible vaccines
Nature Ecology & Evolution (2021)
-
Knowledge gaps about rabies transmission from vampire bats to humans
Nature Ecology & Evolution (2020)
-
Epidemiology and biology of a herpesvirus in rabies endemic vampire bat populations
Nature Communications (2020)