Abstract
Objective
Describe renal function of preterm infants <29 weeks of gestational age (GA) with twin–twin transfusion syndrome (TTTS) who received laser therapy.
Design
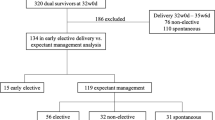
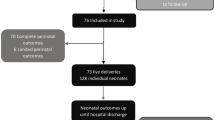
Retrospective analysis of premature TTTS compared with dichorionic–diamniotic (di–di) twins from 2006 to 2015. Primary outcome was biomarkers of renal injury.
Results
Thirty-three TTTS-laser and 101 di–di newborns with similar GA at birth (26.4 ± 1.4 vs 26.9 ± 1.6 weeks, p = 0.07) were included. Creatinine and urea levels were higher in TTTS-laser group at day of life (DOL) 2–7 (123.5 ± 12.4 vs 75.8 ± 2 μmol/L, p = 0.0001 and 11.9 ± 1.1 mmol/L vs 8.7 ± 0.3 mmol/L, p = 0.0001) and DOL 8–14, (98.1 ± 14.2 vs 64.8 ± 2.3 μmol/L, p = 0.0001 and 9.1 ± 1.2 vs 5.4 ± 0.3 mmol/L, p = 0.0001). There was a significant effect of TTTS status on creatinine level at DOL 8–14.
Conclusion
In extremely preterm with TTTS treated by laser, biomarkers of renal function were higher compared with di–di twins in the first 2 weeks of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Harkness UF, Crombleholme TM. Twin-twin transfusion syndrome: where do we go from here? Semin Perinatol. 2005;29:296–304.
Li X, Morokuma S, Fukushima K, Otera Y, Yumoto Y, Tsukimori K, et al. Prognosis and long-term neurodevelopmental outcome in conservatively treated twin-to-twin transfusion syndrome. BMC Pregnancy Childbirth. 2011;11:32.
De Lia JE, Cruikshank DP, Keye WR Jr. Fetoscopic neodymium: YAG laser occlusion of placental vessels in severe twin-twin transfusion syndrome. Obstet Gynecol. 1990;75:1046–53.
Diehl W, Diemert A, Hecher K. Twin-twin transfusion syndrome: treatment and outcome. Best Pr Res Clin Obstet Gynaecol. 2014;28:227–38.
Roberts D, Neilson JP, Kilby MD, Gates S. Interventions for the treatment of twin-twin transfusion syndrome. Cochrane Database Syst Rev. 2014;CD002073.
Sutherland M, Ryan D, Black MJ, Kent AL. Long-term renal consequences of preterm birth. Clin Perinatol. 2014;41:561–73.
Gubhaju L, Sutherland MR, Black MJ. Preterm birth and the kidney: implications for long-term renal health. Reprod Sci. 2011;18:322–33.
Breathnach FM, Malone FD. Fetal growth disorders in twin gestations. Semin Perinatol. 2012;36:175–81.
Hallan S, Euser AM, Irgens LM, Finken MJ, Holmen J, Dekker FW. Effect of intrauterine growth restriction on kidney function at young adult age: the Nord Trondelag Health (HUNT 2) Study. Am J Kidney Dis. 2008;51:10–20.
Schreuder M, Delemarre-van de Waal H, van Wijk A. Consequences of intrauterine growth restriction for the kidney. Kidney blood Press Res. 2006;29:108–25.
Sommer J, Nuyt AM, Audibert F, Dorval V, Wavrant S, Altit G, et al. Outcomes of extremely premature infants with twin-twin transfusion syndrome treated by laser therapy. J Perinatol. 2018;38:1548–55.
Lenclen R, Paupe A, Ciarlo G, Couderc S, Castela F, Ortqvist L, et al. Neonatal outcome in preterm monochorionic twins with twin-to-twin transfusion syndrome after intrauterine treatment with amnioreduction or fetoscopic laser surgery: comparison with dichorionic twins. Am J Obstet Gynecol. 2007;196:450 e451–457.
Mercanti I, Boivin A, Wo B, Vlieghe V, Le Ray C, Audibert F, et al. Blood pressures in newborns with twin–twin transfusion syndrome. J Perinatol. 2011;31:417.
Coutinho Nunes F, Domingues AP, Vide Tavares M, Belo A, Ferreira C, Fonseca E, et al. Monochorionic versus dichorionic twins: are obstetric outcomes always different? J Obstet Gynaecol. 2016;36:598–601.
Fumagalli M, Schiavolin P, Bassi L, Groppo M, Uccella S, De Carli A, et al. The impact of twin birth on early neonatal outcomes. Am J Perinatol. 2016;33:63–70.
Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999;19:550–5.
Society for Maternal-Fetal Medicine (SMFM), Simspson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013;208:3–18.
Soraisham AS, Singhal N, McMillan DD, Sauve RS, Lee SK. A multicenter study on the clinical outcome of chorioamnionitis in preterm infants. Am J Obstet Gynecol. 2009;200:372.e371–376.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
Kilby MD, Platt C, Whittle MJ, Oxley J, Lindop GB. Renin gene expression in fetal kidneys of pregnancies complicated by twin-twin transfusion syndrome. Pediatr Dev Pathol. 2001;4:175–9.
Mahieu-Caputo D, Dommergues M, Delezoide AL, Lacoste M, Cai Y, Narcy F, et al. Twin-to-twin transfusion syndrome. Role of the fetal renin-angiotensin system. Am J Pathol. 2000;156:629–36.
De Paepe ME, Stopa E, Huang C, Hansen K, Luks FI. Renal tubular apoptosis in twin-to-twin transfusion syndrome. Pediatr Dev Pathol. 2003;6:215–25.
Mahieu-Caputo D, Muller F, Joly D, Gubler MC, Lebidois J, Fermont L, et al. Pathogenesis of twin-twin transfusion syndrome: the renin-angiotensin system hypothesis. Fetal Diagn Ther. 2001;16:241–4.
Mahieu-Caputo D, Meulemans A, Martinovic J, Gubler MC, Delezoide AL, Muller F, et al. Paradoxic activation of the renin-angiotensin system in twin-twin transfusion syndrome: an explanation for cardiovascular disturbances in the recipient. Pediatr Res. 2005;58:685–8.
Guilherme R, Patrier S, Gubler MC, Lemercier D, Guimiot F, Dommergues M. Very early twin-to-twin transfusion syndrome and discordant activation of the renin-angiotensin system. Placenta. 2009;30:731–4.
Galea P, Barigye O, Wee L, Jain V, Sullivan M, Fisk NM. The placenta contributes to activation of the renin angiotensin system in twin-twin transfusion syndrome. Placenta. 2008;29:734–42.
Verbeek L, Joemmanbaks FA, Quak JME, Sukhai RN, Middeldorp JM, Oepkes D, et al. Renal function in neonates with twin-twin transfusion syndrome treated with or without fetoscopic laser surgery. Eur J Pediatr. 2017;176:1209–15.
Luyckx VA. Preterm birth and its impact on renal health. Semin Nephrol. 2017;37:311–9.
Rodriguez MM, Gomez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol. 2004;7:17–25.
Luyckx VA, Bertram JF, Brenner BM, Fall C, Hoy WE, Ozanne SE, et al. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet. 2013;382:273–83.
White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, et al. Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis. 2009;54:248–61.
Paquette K, Fernandes RO, Xie LF, Cloutier A, Fallaha C, Girard-Bock C, et al. Kidney size, renal function, Ang (angiotensin) peptides, and blood pressure in young adults born preterm. Hypertension. 2018;72:918–28.
Nuyt AM, Lavoie JC, Mohamed I, Paquette K, Luu TM. Adult consequences of extremely preterm birth: cardiovascular and metabolic diseases risk factors, mechanisms, and prevention avenues. Clin Perinatol. 2017;44:315–32.
Sutherland MR, Gubhaju L, Moore L, Kent AL, Dahlstrom JE, Horne RS, et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J Am Soc Nephrol. 2011;22:1365–74.
Toth-Heyn P, Drukker A, Guignard JP. The stressed neonatal kidney: from pathophysiology to clinical management of neonatal vasomotor nephropathy. Pediatr Nephrol. 2000;14:227–39.
Hinchliffe SA, Lynch MR, Sargent PH, Howard CV, Van Velzen D. The effect of intrauterine growth retardation on the development of renal nephrons. Br J Obstet Gynaecol. 1992;99:296–301.
Bertram JF, Douglas-Denton RN, Diouf B, Hughson MD, Hoy WE. Human nephron number: implications for health and disease. Pediatr Nephrol. 2011;26:1529–33.
Luyckx VA, Brenner BM. Birth weight, malnutrition and kidney-associated outcomes–a global concern. Nat Rev Nephrol. 2015;11:135–49.
Luyckx VA, Perico N, Somaschini M, Manfellotto D, Valensise H, Cetin I, et al. A developmental approach to the prevention of hypertension and kidney disease: a report from the Low Birth Weight and Nephron Number Working Group. Lancet. 2017;390:424–8.
Lewi L, Gucciardo L, Huber A, Jani J, Van Mieghem T, Done E, et al. Clinical outcome and placental characteristics of monochorionic diamniotic twin pairs with early- and late-onset discordant growth. Am J Obstet Gynecol. 2008;199:511 e511–517.
Van Winden KR, Quintero RA, Kontopoulos EV, Korst LM, Llanes A, Chmait RH. Perinatal survival in cases of twin-twin transfusion syndrome complicated by selective intrauterine growth restriction. J Matern Fetal Neonatal Med. 2015;28:1549–53.
Melhem NZ, Ledermann S, Rees L. Chronic kidney disease following twin-to-twin transfusion syndrome-long-term outcomes. Pediatr Nephrol. 2019;34:883–8.
Beck M, Graf C, Ellenrieder B, Bokenkamp A, Huber A, Hecher K, et al. Long-term outcome of kidney function after twin-twin transfusion syndrome treated by intrauterine laser coagulation. Pediatr Nephrol. 2005;20:1657–9.
Liborio AB, Branco KM, Torres de Melo Bezerra C. Acute kidney injury in neonates: from urine output to new biomarkers. BioMed Res Int. 2014;2014:601568.
Kalhan SC, Wilson-Costello D. Prematurity and programming: contribution of neonatal Intensive Care Unit interventions. J Dev Orig Health Dis. 2013;4:121–33.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sommer, J., Nuyt, AM., Audibert, F. et al. Renal functional markers in extremely premature infants with and without twin–twin transfusion syndrome. J Perinatol 40, 256–262 (2020). https://doi.org/10.1038/s41372-019-0524-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0524-5