Abstract
Aim
The aim was to compare adult patients’ experiences of public and private dental care in Sweden over time from the ages of 50 and 70 years, between 1992 and 2012.
Materials and methods
Data on visiting patterns, oral health, fees and satisfaction were obtained from a questionnaire study every 5 years in 1992–2012 and analysed by using the Chi-square test and logistic regression. In the present study, the answers given by 6083 respondents in 1992 and 5220 in 2012 were included.
Results
Of the 50-year olds, 73.5% had visited the private sector and 26.5% the public sector. In 1992, patients in the public dental service (PDS) had visited their dentists less frequently and experienced having a slightly poorer dental status compared with private patients. After 20 years (2012), the distribution of patients between the two sectors was almost the same (71.4% and 28.8%) and the differences in visiting pattern and dental health persisted. During the study period, 21.6% of the patients changed treatment sector. A small proportion of patients had high treatment costs. A larger proportion of the private sector visitors than the PDS visitors were consistently satisfied with the dental care they had received.
Conclusions
As a whole, most adult patients in Sweden were satisfied with their dental care at both public and private clinics.
Similar content being viewed by others
Introduction
In Sweden, there are both public and private oral health-care providers. The public dental service (PDS, Folktandvården) is operated by all 21 county councils/regions (20 CCs and one municipality), with approximately 880 dental clinics. Private dental care comprises approximately 2000 care providers (many with more than one dentist) with approximately 3550 dental surgeries. Of the 7528 dentists (in 2013), 4070 (54%) were publicly employed and 3458 (46%) worked in the private sector.1 The number of dentists has been relatively constant since the beginning of the 1990s, with about 7500 professional dentists, and this also applies to the distribution between the sectors. Approximately 60% of adult patients visit private dental care providers, while 40% visit the PDS.2
In 1992, two of the CCs, Örebro (T) and Östergötland (E), started a prospective population study within dentistry. The aim was to ask all 50-year-old residents in these CCs about their opinions of their own teeth and the dental care provided for them. CC politicians initiated the study. The purpose was to study the extent to which the CCs met the legal requirements relating to the availability of dental services when needed by the residents. In addition to providing a basis for planning dental care for groups of elderly people in the CCs, the results were going to be used by the National Board of Health and Welfare in its work on indicators of good dental care.3 The study was repeated every 5 years until 2012 and it has resulted in a number of publications on the respondents’ opinions of their oral health, dental care habits and attitudes to and experiences of dental care.4,5 Most respondents in 1992 felt that their oral health was good (89%) and 64% said they attended a dental clinic at least once a year. Satisfaction with dental care was high (94%).6
To date, the database generated from the surveys in the two counties, T and E, has not been used for a comparison of public and private providers. In other countries, treatment in the public sector is less expensive for the patients than in the private sector and the PDS is more frequently used by people with a lower income and/or lower education than the private sector. Public sector patients may belong to so-called special needs groups and the treatment may differ in comparison with the private sector.7,8,9 We felt it would be interesting to explore whether this was also the case in Sweden in the present study.
In 1992, when the study started, all dental treatment (including bridgework and prosthetics) for adults was generously (25–75%) subsidised by the government. The PDS and the private sector had the same fixed fees and a high-cost protection system gave extra support to patients with large-scale treatment needs.10 In 1998, the subsidy system was reformed. In brief, subsidies were restricted to “basic dental care” for all adults (not including examinations, prosthodontics or orthodontics). Subsidies were higher for people with disease and disability. Subsidy for “contract care” was introduced. Establishment control was taken away and free pricing was introduced, enabling the private dentists and the CCs to set the service charges as they chose.11 This resulted in private dental care becoming more expensive than public care.12
The next dental reform was introduced in 2008. The system established then is still in place today in 2019. An annual “general dental allowance” (Allmänna TandvårdsBidraget, ATB) was introduced for all adults; it was 150 or 300 SEK (£14 or 28), depending on age. A “protection against high costs” with a subsidy from the government was also introduced. This cap on private spending was based on reference prices defined by the government, as providers were free to set patient fees.13 This means that, in comparison with 1992 and 1997, adults had to cover a considerably larger share of their dental costs out of pocket in 2002–2012. On the other hand, adults’ oral health has improved during that period. According to a longitudinal study in the City of Jönköping in Southern Sweden: “The proportions of edentulous individuals aged 40–70 years were 16%, 12%, 8%, 1% and 0.3% in 1973, 1983, 1993, 2003 and 2013, respectively. No complete denture wearer younger than 80 years was found in 2013. During the 40-year period, the mean number of teeth in the 30- to 80-year age groups increased. In 2013, the 60-year olds had almost complete dentitions”.14,15
Aim
The aim of this study was to investigate adults’ experiences and opinions of the dental care they have received over time from the age of 50–70 years. Patients’ dental visiting patterns, satisfaction with care, oral health measured as the numbers of teeth and fees paid are compared between the two types of provider, public and private. We also sought to explore possible changes in the use of the two provider groups during the study period and differences between the patients who had visited the public sector and those who had visited the private sector at the start and the end of the study. In addition, a longitudinal follow-up was conducted among those who claimed to have visited only the public sector or the private sector and those who claimed to have used both sectors during the whole study period.
Material and methods
The data in this study emerged from a data collection procedure at the beginning of 1992, when all 50-year-old residents (n = 8888) in the Counties of Örebro (T) and Östergötland (E) were sent a postal questionnaire relating to their “experiences of dental care and oral health”. The questionnaire was validated and then approved by the Ethical Review Board in Uppsala (Dnr 2011/336). Basically the same questionnaire was sent to the cohort born in 1942 every 5 years until 2012. In 1992, the response rate was 71.4% (n = 6343), in 1997, 74.3% (n = 6513), in 2002, 75.0% (n = 6372), in 2007, 73.1% (n = 6078) and, in 2012, 72.2% (n = 5697).6 In the present study, the answers were analysed from 6083 respondents in 1992 and 5220 respondents in 2012, who stated that they had visited the PDS or private clinics.
This study focused on the following variables: (a) frequency of dental visits (How often did you make dental visits during the last 5 years?), (b) treatment sector (Where did you mainly have dental care during the last 5 years?), (c) cost of dental treatment paid by the patients (How much did you pay out of pocket for dental care during the last year?), (d) satisfaction with the treatment (Are you generally satisfied/not satisfied with the dental care you have received?) and (e) the number of their own teeth remaining (How many of your own teeth do you have?). The alternative answers to all the questions are shown in Table 1. Background factors were education, gender, marital status and country of birth. All respondents did not always answer all the questions.
Statistical methods
Chi-square tests were performed on differences between the PDS and private visitor cohorts at baseline and in 2012. The Chi-square test was also used to analyse changes in visiting patterns, number of teeth and satisfaction between 1992 and 2012 for patients who never changed dental care provider sector during the 20-year period. In order to further analyse the factors that might influence the odds of having “all teeth left” after a 20-year follow-up, a logistic regression was performed. p-Values below 0.05 were considered to be significant.
Statistical analyses were conducted using R version 3.4.2 for Windows.16
Results
Adults 50 years of age in 1992
In 1992, most of the then 50-year-old respondents (4471; 73.5%) had visited the private sector and 1612 (26.5%) the public sector. There were no statistically significant differences between the private and public visitors as regards gender or marital status, but PDS visitors had a significantly lower educational level (p < 0.05) and a larger proportion of them were born outside Sweden (p < 0.001; Table 1). Respondents who had made their latest dental visits to the PDS had fewer of their own teeth than those who had visited private dentists; e.g. 17.4% of the former had all their teeth left in comparison to 24.2% of the latter (p < 0.001; Table 1). The public visitors had visited their dental clinic more seldom than the private visitors, they were less satisfied with the care they had received (p < 0.001) and they had paid less for their treatment (p < 0.05; Table 1). Of all the respondents, 76.8% claimed to have paid less than 1000 SEK (£83.4), corresponding to 1422 SEK (£119.2) in today’s monetary value.17 In 1992, the average income for 50-year-old Swedes was 15604 SEK (£1271.4).18
Adults 70 years of age in 2012
In 2012, the total number of respondents had fallen from 6083 in 1992 to 5220 (8.7%). The proportion of respondents who had most recently visited the private sector was 71.4% (3738) and, of those having visited the public sector, 28.8% (1482). These proportions were almost at the same level as 20 years earlier. The proportion of private visitors with a university education (27.6%) was significantly higher (p < 0.001) than that of the public visitors, 22.3% (Table 2). The respondents as a whole had a higher educational level in 2012 than in 1992. According to the answers to the questionnaire, those respondents who had mainly visited the PDS during the past 5 years had, as in 1992, statistically significantly fewer of their own teeth than those who had visited private dentists (p < 0.001; Table 2). The public visitors had visited their dental clinic less frequently than the private visitors and they were less satisfied with the care they had received (p < 0.001). There were statistically significant differences in costs paid, as the PDS visitors had paid less than the private sector visitors. Of all the respondents, 89.7% claimed to have paid less than 8000 SEK (£670.5), corresponding to 8363 SEK (£701.1) in today’s monetary value (Table 2). In 2012, the average income per month for 70-year-old Swedes was 18,167 SEK (£1480.2).19 The general retirement age in Sweden is 65 years.
Private or public dental care only, or both in 1992–2012
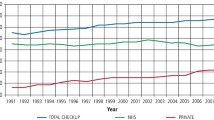
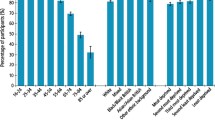
Of the initial 4471 private visitors and, of the initial 1612 PDS visitors, who answered the questionnaire in 1992 and 2012, 2478 private visitors (55.4%) and 649 public visitors (40.2%) claimed to have visited the same treatment sector all the time. Most private patients (64.8%) claimed to have maintained the same visiting frequency as in 1992 in contrast to 51.0% of the PDS visitors (p < 0.001; Table 3, Fig. 1). A statistically significantly larger proportion (25.9%) of the PDS visitors visited their dentist more seldom than before, in contrast to 17.6% of the private visitors (p < 0.001; Table 3).
Over time, the proportion of respondents who claimed to have retained practically all their teeth decreased in both sectors (Fig. 2). Of the PDS visitors, 64.4% and, of the private sector visitors, 62.1% said that they belonged to the same “numbers of teeth category” during the whole study period (p < 0.05). About a quarter (24.3%/26.1%) claimed to have fewer teeth and, interestingly, 7.6%/7.7% had more teeth than initially (Table 3).
A larger proportion of the private sector visitors than PDS visitors were consistently more satisfied with the dental care they had received (Fig. 3, Table 3). At baseline, there was a difference of 10.7% among “very pleased” in favour of private dentistry. Over time, the private sector appeared to retain this position, while the PDS decreased slightly (Fig. 3).
There was also a group we called “mixed”. Individuals belonging to this group changed their care provision sector during the period. A larger proportion of respondents in this group had “fewer teeth in 2012” than respondents in the PDS and private groups (p < 0.05). Their visiting frequency was midway between the PDS and private visitors, as was their satisfaction level (Table 3).
A separate analysis of those who, after the 20-year follow-up period, had “all their teeth left or were only missing a single tooth” (Table 4) showed that university-educated subjects had 45.8% higher odds and private sector visitors 29.6% higher odds of having all their teeth left. Married people had 19.2% higher odds than unmarried people and men had 14.3% higher odds than women of retaining their natural teeth. The results also showed that individuals born outside Sweden had lower odds, 14.8%/16.5%, of retaining all or most of their teeth than native Swedes (Table 4).
Discussion
Self-report surveys have been frequently used in Sweden when studying the use of various public services by adults, as the method has been regarded as feasible and reliable, with a response rate that is sufficiently high to generate results with good validity.20 The material used in the present study has been found to be representative of the birth cohort born in 1942. It thus provides information on the dental care of 50- to 70-year-old individuals in the two counties surveyed.21 The respondents in longitudinal surveys are exposed to a changing societal environment over time and, in this study, also changes in the care provision and financing systems, which may influence their opinions. They also became older, another circumstance that may influence their perspectives.3 This must be considered when interpreting the results.
The study showed that most (4471, 73.5%) of the 6083 50-year olds participating in the study in 1992 had made their latest dental visit to the private sector. Was this because of old habits or social segregation? Because the patient fees at that time were fixed and the same in both sectors, one of the most usual reasons in other countries for using the public sector, namely lower fees, did not apply here. Moreover, because there were no formal restrictions for adults to use the PDS, an explanation of the low use of the PDS might be that it was regarded as a care-giver primarily for children and young people. Further, in 2012, 71.6% of the respondents said that their latest visit had been to the private sector, although the free pricing, introduced in 1998, had made treatment in the PDS less expensive than in the private sector.12 The private sector is known to be efficient in recalling its patients and regular attenders are more comfortable with dental visits.22,23 Our earlier study showed that the Chief Dental Officers (CDOs), who were PDS leaders in the CCs, felt that keeping their former child patients in the PDS when they become adults was an important strategy.24 This is supported by the new contract care payment system in Sweden (so-called “Frisktandvård”), allowing a certain annual fee to be paid by the patient irrespective of treatment needed and provided, being most suitable for young adults.25
At the beginning of the study, patients who visited the PDS had a slightly poorer dental status, compared with private patients. This is in accordance with studies from other countries.7,8 This difference also persisted over the entire examination period (1992–2012). For example, both examined groups experienced a decrease in the group answering “all teeth left”, but the decrease was larger in the PDS, from 17.1% to 9.5%, than in the private sector, from 24.2% to 14.2%. On the other hand, when looking at the variables “lower number of teeth” and “same number of teeth”, the figures showed that the tooth losses are on the same level in both sectors (p > 0.05) (Table 3). Because the formulation of the questions did not make it possible to follow the exact numbers of teeth during the study period, differences of this kind are difficult to explain. However, it was obvious that, during the 20-year study period, many of the “ageing” patients lost teeth independent of treatment sector. Those who did not lose teeth were highly educated, visited the private sector and were more often men and married than women or unmarried, which is in accordance with findings in other studies.26 Well-educated people are usually able to manage good oral self-care. Private dental clients are able to visit a dentist or a dental hygienist frequently and presumably have frequent opportunities to obtain professional preventive treatment and advice. One explanation of why married people have higher odds than singles of retaining all their teeth might be that married people live a more stable life with fixed routines. It is more difficult to explain why men had higher odds. The difference between men and women was fairly small (14.3%).
One interesting finding in the present study was that about 10% of the respondents claimed that the number of teeth increased during the 20-year period. It may be difficult for patients to differentiate between natural teeth and bridgework and implants and so they may answer that they have more teeth. In Sweden, having decent-looking teeth, your own or artificial, has long been regarded as politically important and prosthetic treatment has been easily available and highly subsidised.9,11
An analysis of the visiting frequency revealed that, in the PDS, the pattern of rare visits increased over time and frequent visitors also increased. In the private sector, the visiting frequencies hardly changed at all. This might be due to the practice in private dental care with “a yearly visit to the dentist”, while the PDS has differentiated the recall intervals by risk assessments based on differences in patients’ oral health but probably also influenced by the availability of staff. In Sweden, the PDS has had access problems, depending on a lack of dentists, all over the country and especially in rural areas since 2007.27 This may explain the increase in the number of rare visitors. The increase in frequent visitors may be explained by the increase in the number of dental hygienists in the PDS. Dental hygienists have been seen to make an important contribution to dental care and hence the ratio of dental hygienists to dentists (2 per 5 dentists) is by international standards relatively high in Sweden.
Costs paid by the patients were difficult to compare over time, because of the many changes in the state subsidies during the 20-year period and changes to the question of patient costs in the questionnaire. At the start, in 1992, 76.8% of the respondents claimed to have paid very little, less than 1422 in current SEKs (£120) for all their dental treatment during the period of a year. Dental care was generously remunerated by the national dental insurance, as explained in the “Introduction”. Only 18.3% of PDS and 21.2% of private patients paid more than 1422 SEK (£119.2) (p < 0.001). In 2012, free pricing had been introduced and the subsidy for dental costs started at 3000 SEK. The price level was much higher, too. In 2012, 89.7% of all patients paid below the high-level limit, which was set at 8363 SEK (£701.0) in today’s monetary value. The number of patients paying more than 8363 SEK was 5.3% in the PDS and 6.1% in the private sector (p < 0.001). This indicates that there were very few patients paying high costs, but there were significantly more private patients doing so.
Ståhlnacke et al.28,29 noted in their studies that adults’ satisfaction with dental services was high both in general and with the most recent dental visit, where non-visitors within the last year were more dissatisfied than those who had paid a visit during the last year. Having a high cost for care also increased dissatisfaction but to a smaller degree. The authors were not able to document any correlation between socioeconomic factors and service satisfaction.
Hancock et al.30 in the UK investigated private or NHS general dental service care and patients’ satisfaction in certain respects. They noted that satisfaction was greater in private dental care due to perceived access and availability and not because of technical skills.
In our study, the satisfaction rate among the private patients stayed high over the years (55% were very satisfied) but decreased for the PDS patients from 45% to 35% (Fig. 3). One possible explanation is that access and availability were greater in private dentistry. Moreover, the treatment profile of the private dentists differs from that of the PDS, which is shown in other investigations.9 More advanced and expensive care is provided in the private sector and simpler, less expensive care, like extractions and fillings, in the PDS.31 In the above-mentioned study in Finland, adult patients in the PDS were shown to have more examinations and emergency care, while private patients received more comprehensive care.9
Finally, there was a group of respondents using both sectors. This mixed group represented 21.6% of the cohort, showing that many people wanted or needed to change their dental treatment supplier over time. People belonging to this mixed group were shown to lose more teeth than the PDS and private sector attenders and to make more frequent dental visits than the PDS visitors but less often than the private sector visitors. They did not change their degree of satisfaction during this period. These sector users appeared to be more irregular attenders and probably visited dentists when needed, due to pain or lost fillings, and want to choose their visits on their own, not via a recall system. Some private and mixed sector visitors may also have needed specialist care, which is predominantly provided in the public sector in Sweden. According to the Swedish National Board of Health and Welfare, 66% of men and 73% of women made dental visits to obtain a basic examination during the 3-year period, from 2015 to 2017. Older people used dental services more often than younger ones.11
Conclusions
There are some differences between PDS and private dentistry in a longitudinal study spanning 20 years. The differences mainly relate to satisfaction, access and availability of dental care. Most private patients appear to visit their dental clinic with the same frequency, once a year or more often, over time, while the PDS has a more uneven visiting pattern. Over 20% of the patients changed provider between the two sectors during a 20-year period. This is an interesting observation, but the reason is not explained in this study.
In Sweden, the regular use of dental services throughout life is regarded as important and is believed to contribute to a good dental appearance and functioning dentition. The two treatment sectors, the PDS and the private sector, play slightly different roles and, as competitors, for example, it is hoped that they will drive quality development forward and display the best possible ability to meet the demands of patients and politicians. It seems apparent from the present study that the two sectors also complement one another.
References
Socialstyrelsen (Swedish Agency of Health and Welfare). In Swedish: Nationella PlaneringsStödet 2013—tillgång och efterfrågan på vissa personalgrupper inom hälso-och sjukvård samt tandvård (National Planning Support 2013—Supply and Demand for Certain Personnel Groups Within Healthcare and Dental Care). Available online at: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18961/2013-1-18.pdf. Accessed Feb 2019.
TLV (The Dental and Pharmaceutical Benefits Agency). In Swedish: Tandvårdsmarknaden (The Dental Market). Available online at: https://www.tlv.se/tandvard/Tandvardsmarknaden/. Accessed Feb 2019.
Ekbäck, G. & Ordell, S. In Swedish: Munhälsa och tandvård, TE-studierna—befolkningsenkäter i Örebro och Östergötlands län (Oral Health and Dental Care, TE Studies—Population Surveys in Örebro and Östergötland County). Available Online at: https://www.regionorebrolan.se/Files-sv/Örebro%20läns%20landsting/Tandvard/Tandvårdsenheten/Rapporter/TE-studierna%20-%20Munhälsa%20och%20tandvård.pdf. Accessed Feb 2019.
Unell, L., Söderfeldt, B., Halling, A. & Birkhed, D. Explanatory models for oral health expressed as number of remaining teeth in an adult population. Community Dent. Health 15, 155–161 (1998).
Unell, L., Söderfeldt, B., Halling, A., Paulander, J. & Birkhed, D. Oral diseaese, impairment and illness; congruence between clinical and questionnaire findings. Acta Odontol. Scand. 55, 127–132 (1997).
Unell, L., Söderfeldt, B., Halling, A. & Birkhed, D. Attitudes to and experience of dental care among 50-year-olds in two Swedish counties. Swed. Dent. J. 23, 87–96 (1999).
Brennan, D. S., Do, L. G. & Slade, G. D. Caries experience of adults attending private and public dental clinics in Australia. J. Pub. Health Dent. 71, 2–37 (2011).
Pinto, R., de Abreu, M. & Vargas, A. Comparing adult users of public and private dental services in the state of Minas Gerais, Brazil. BMC Oral Health 14, 100 (2014).
Widström, E. & Linden, J. Treatment provided in the public dental service and by private dentists in Finland. Oral Health Dent. Manag. 17, 1024 (2018).
Koch, B. In Swedish: Tandvårdsförsäkringens tillkomst och förändring (The origin and change of the Swedish Dental Care Insurance System). Sven. Med. Tidskr. 18, 86–88 (2014).
Socialstyrelsen (Swedish Agency of Health and Welfare). In Swedish: Statistik om tandhälsa 2017 (Statistics on Dental Health 2017). Available online at: https://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/20972/2018-5-16.pdf. Accessed May 2019.
Försäkringskassan (Swedish Social Insurance Agency). In Swedish: Antal åtgärder per år och dess medianpriser, 2009—Tabell 4 (Number of measures per year and their median prices, 2009—Table 4). Available online at: https://www.forsakringskassan.se/statistik/ovrigaersatt/tandvard. Accessed Feb 2019.
Sveriges Riksdag (The Swedish Parliament). In Swedish: Lag (2008: 145)om statligt tandvårdsstöd. svensk författningssamling 2008: 145 (The Act (2008: 145) Governing State Dental Care. Swedish Constitution Collection 2008) Available Online at: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-2008145-om-statligt-tandvardsstod_sfs-2008-145. Accessed June 2017.
Norderyd, O. et al. Oral health of individuals aged 3–80 years in Jönköping, Sweden during 40 years (1973–2013). II. Review of clinical and radiographic findings. Swed. Dent. J. 39, 69–86 (2015).
Jansson, H., Norderyd, O., Papias, A. & Wahlin, Å. Secular trends over 40 years of periodontal health and disease in individuals aged 20-80 years in Jönköping, Sweden: repeated cross-sectional studies. J. Clin. Peridontol. 45, 1016–1024 (2018).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria, 2017).
Valutakurser (Currency Exchange Rates). Available online at: http://www.valutaomvandlare.com. Accessed May 2019.
SCB (Statistics Sweden). In Swedish: Lönestatistik årsbok 1992 (Wage Statistics Yearbook 1992). Available online: https://www.scb.se/Grupp/Hitta_statistik/Historisk_statistik/_Dokument/SOS/Loner/Lonestatistisk-arsbok-1992.pdf. Acessed May 2019.
SCB (Statistics Sweden). In Swedish: Statistikdatabasen (Statistical Database). Available online at: http://www.statistikdatabasen.scb.se/pxweb/sv/ssd/START__HE__HE0110__HE0110A/SamForvInk1/table/tableViewLayout1/?rxid=3333c1a8-d99d-4a76-94ee-07e3f60908d7. Accessed May 2019.
Landfeldt, E., Zethraeus, N. & Lindgren, P. Standardized questionnaire for the measurement, valuation, and estimation of costs of informal care based on the opportunity cost and proxy good method. Health Econ. Health Policy 17, 15–24 (2019).
Ekbäck, G. & Ordell, S. Self-perceived taste disturbance: a 20-year prospective study of a Swedish 1942 birth cohort. Gerodontology 34, 180–186 (2017).
Widström, E., Komu, M. & Mikkola, H. Longitudinal register study of attendance frequencies in public and private dental services in Finland. Community Dent. Health 30, 143–148 (2013).
Ståhlnacke, K. Self-perceived oral health, dental care utilization and satisfaction with dental care. Swed. Dent. J. Suppl. 190, 1–155 (2007).
Pälvärinne, R., Birkhed, D. & Widström, E. The Public Dental Service in Sweden: an interview study of chief dental officers. J. Int. Soc. Prev. Community Dent. 8, 205–211 (2018).
Andrén Andås, C. A New Payment Model in Swedish Dental Care. Available online at: https://www.gupea.ub.gu.se/handle/2077/39557. Accessed June 2017.
Mundt, T. et al. Gender-dependent associations between socioeconomic status and tooth loss in working age people in the Study of Health Pomerania (SHIP), Germany. Community Dent. Oral. Epidemiol. 39, 398–408 (2011).
Socialstyrelsen (Swedish Agency of Health and Welfare). In Swedish: Årsrapport NPS 2008. En analys av barnmorskors, sjuksköterskors, läkares, tandhygienisters och tandläkares arbetsmarknad (Annual Report NPS 2008. An Analysis of Midwives’, Nurses’, Doctors’, Dental Hygienists’ and Dentists’ Labour Market). Available online at: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8840/2008-131-10_200813110_rev1.pdf. Accessed Feb 2019.
Ståhlnacke, K., Söderfeldt, B., Unell, L., Halling, A. & Axtelius, B. Patient satisfaction with dental care in one Swedish age cohort. Part 1—descriptions and dimensions. Swed. Dent. J. 31, 103–111 (2007).
Ståhlnacke, K., Söderfeldt, B., Unell, L., Halling, A. & Axtelius, B. Patient satisfaction with dental care in one Swedish age cohort. Part II—What affects satisfaction? Swed. Dent. J. 31, 137–146 (2007).
Hancock, M., Calnan, M. & Manley, G. Private or NHS general dental service care in the United Kingdom? A study of public perceptions and experiences. J. Public Health Med. 21, 415–420 (1999).
Tuominen, R., Eriksson, A.-L. & Vahlberg, T. Private dentists assess treatment required as more extensive, demanding and costly, than public sector dentists. Community Dent. Oral. Epidemiol. 40, 362–368 (2012).
Acknowledgements
The authors thank Jeanette Kliger, for English revision, and Eva Hagel, Karolinska Institute, for conducting the statistical analyses. The authors are also grateful to Tommy Johansson, County Council of Örebro, and Maria Johansson, County Council of Östergötland, for letting them utilise the database of the original questionnaire study. This study was supported for publication by “The authors’ foundation” at Malmö University.
Author information
Authors and Affiliations
Contributions
R.P.: main author, responsible for planning the study and statistical analysis, together with the statistician. E.W.: main supervisor, conducted the main revision of the manuscript. D.B. and B.F.: contributed valuable comments. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pälvärinne, R., Birkhed, D., Forsberg, B. et al. Visitors’ experiences of public and private dental care in Sweden in 1992–2012. BDJ Open 5, 12 (2019). https://doi.org/10.1038/s41405-019-0020-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41405-019-0020-1
This article is cited by
-
BDJ Open (2019-2020) and the advantages of open access publishing
British Dental Journal (2021)