Abstract
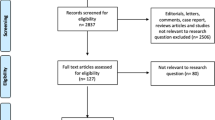
Ischaemic priapism (IP) is characterised by a persistent, painful penile erection lasting for >4 h. Many causes of IP have been identified including haematological dyscrasias (particularly, sickle cell disease), drugs and rarely malignancy. There are also a large proportion of men, in which no aetiology is identified. Identification of men at risk for malignancy provides a diagnostic challenge to the clinicians looking after these patients. All cases of IP between 2007 and 2017 at a single tertiary andrology unit were identified. The case notes and electronic records of these patients were reviewed to identify cases of malignant priapism. Men with idiopathic IP were used as a control group for comparative statistics. In total, 412 men with IP were identified, 202 of which had idiopathic IP. Within this group, the prevalence of malignant priapism was 3.5% (n = 11). MP secondary to local invasion or penile metastases occurred in seven of the 11 men (bladder × 3, prostate, lung, urethral and chondrosarcoma of the pelvis). MP secondary to haematological malignancy occurred in the remaining four (chronic myeloid leukaemia × 2, chronic lymphocytic leukaemia, and myelodysplasia). IP was the initial presentation of malignancy in seven of the patients (64%). An abnormally low haemoglobin value (reference range 130–180 g/dl) was found in 82% (n = 9) of the men with MP. The mean haemoglobin value in men with MP was 109.64 ± 20.30 g/dl compared to the control of 131.87 ± g/dl. This difference was considered highly significant p = 0.0046. Men with MP also appear to have a very poor prognosis with an 18-month mortality of 64% (n = 7). Malignancy is a rare and important cause of IP. A low haemoglobin is a predictor of malignancy and warrants further investigation in IP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Salonia A, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Vardi Y, et al. European Association of Urology guidelines on priapism. Eur Urol. 2014;65:480–9.
Shigehara K, Namiki M. Clinical management of priapism: a review. World J Mens Health. 2016;34:1–8.
Hudnall M, Reed-Maldonado AB, Lue TF. Advances in the understanding of priapism. Transl Androl Urol. 2017;6:199–206.
Champion HC, Bivalacqua TJ, Takimoto E, Kass DA, Burnett AL. Phosphodiesterase-5A dysregulation in penile erectile tissue is a mechanism of priapism. Proc Natl Acad Sci USA. 2005;102:1661–6.
Bivalacqua TJ, Musicki B, Hsu LL, Berkowitz DE, Champion HC, Burnett AL. Sildenafil citrate-restored eNOS and PDE5 regulation in sickle cell mouse penis prevents priapism via control of oxidative/nitrosative stress. PLoS ONE. 2013;8:e68028.
Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, et al. American Urological Association guideline on the management of priapism. J Urol. 2003;170(4 Pt 1):1318–24.
Becerra-Pedraza LC, Jimenez-Martinez LE, Pena-Morfin I, Nava-Esquivel R, Villegas-Martinez JA. Priapism as the initial sign in hematologic disease: case report and literature review. Int J Surg Case Rep. 2018;43:13–7.
da Silva Gaspar SR, Nunes A, Dias JS, Lopes T. Malignant priapism: Penile metastasis originating on a primary prostate adenocarcinoma. Urol Ann. 2015;7:391–5.
Wickham H. ggplot2: elegant graphics for data analysis. New York; London: Springer; 2009.
Cherian J, Rao AR, Thwaini A, Kapasi F, Shergill IS, Samman R. Medical and surgical management of priapism. Post Med J. 2006;82:89–94.
Zacharakis E, Garaffa G, Raheem AA, Christopher AN, Muneer A, Ralph DJ. Penile prosthesis insertion in patients with refractory ischaemic priapism: early vs delayed implantation. BJU Int. 2014;114:576–81.
Broderick GA, Gordon D, Hypolite J, Levin RM. Anoxia and corporal smooth muscle dysfunction: a model for ischemic priapism. J Urol. 1994;151:259–62.
Dubocq FM, Tefilli MV, Grignon DJ, Pontes JE, Dhabuwala CB. High flow malignant priapism with isolated metastasis to the corpora cavernosa. Urology. 1998;51:324–6.
van de Wiel A. Anemia in critically ill patients. Eur J Intern Med. 2004;15:481–6.
Rodgers R, Latif Z, Copland M. How I manage priapism in chronic myeloid leukaemia patients. Br J Haematol. 2012;158:155–64.
Shaeer OK, Shaeer KZ, AbdelRahman IF, El-Haddad MS, Selim OM. Priapism as a result of chronic myeloid leukemia: case report, pathology, and review of the literature. J Sex Med. 2015;12:827–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
James Johnson, M., Hallerstrom, M., Alnajjar, H.M. et al. Which patients with ischaemic priapism require further investigation for malignancy?. Int J Impot Res 32, 195–200 (2020). https://doi.org/10.1038/s41443-019-0141-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0141-z
This article is cited by
-
A population-based analysis of predictors of penile surgical intervention among inpatients with acute priapism
International Journal of Impotence Research (2023)
-
Le priapisme, une urgence urologique: définition et prise en charge
Urologie in der Praxis (2023)