Abstract
Objectives
To assess whether Medicare expenditures for men with incident prostate cancer, treated in Accountable Care Organizations (ACOs) differ from those of men treated in non-ACOs.
Methods
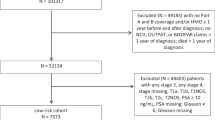
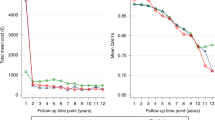
Using the 20% Medicare sample, total charges for 1 year following an initial diagnosis of prostate cancer were abstracted from Medicare claims. Prostate cancer expenditures were calculated by subtracting total charges from the year prior to diagnosis. Propensity score weighting was used to balance baseline characteristics of men treated in ACOs and non-ACOs, and between treatment modalities (radiation, prostatectomy, and expectant management). A propensity score weighted regression model was then used to estimate mean expenditures for men with prostate cancer treated in ACOs and non ACOs and to test the association between ACO status and costs.
Results
We identified 3297 men treated in ACOs for localized prostate cancer versus 24,088 in the non-ACO cohort. The weighted total charges for each treatment modality were $32,358 (radiation), $27,662 (prostatectomy), and $11,134 (expectant management). In our propensity score weighted regression model, the association between charges and ACO status was not significant, nor was the interaction between treatment type and costs. This was true both overall, and in a stratified analysis by treatment type.
Conclusions
There was no significant difference in Medicare spending on prostate cancer care based on provider ACO affiliation, regardless of treatment type. Although the effects of ACOs on clinical care are complex, this study adds to a growing body of evidence suggesting that ACOs fail to achieve significantly lower charges in certain clinical settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fisher ES, McClellan MB, Bertko J, Lieberman SM, Lee JJ, Lewis JL, et al. Fostering accountable health care: moving forward in medicare. Health Aff (Millwood). 2009;28:w219–31.
Devore S, Champion RW. Driving population health through accountable care organizations. Health Aff (Millwood). 2011;30:41–50.
MSSP ACO Fact Sheet: Centers for Medicare and Medicaid Services; 2017. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/All-Starts-MSSP-ACO.pdf.
Federal Register: Medicare Shared Savings Program: accountable care organizations: Centers for Medicare and Medicaid Services; 2015. p. 32691-845.
McWilliams JM, Chernew ME, Landon BE. Medicare ACO program savings not tied to preventable hospitalizations or concentrated among high-risk patients. Health Aff (Millwood). 2017;36:2085–93.
McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early performance of accountable care organizations in medicare. N Engl J Med. 2016;374:2357–66.
Schwartz AL, Chernew ME, Landon BE, McWilliams JM. Changes in low-value services in year 1 of the medicare pioneer accountable care organization program. JAMA Intern Med. 2015;175:1815–25.
Leow JJ, Cole AP, Seisen T, Bellmunt J, Mossanen M, Menon M, et al. Variations in the costs of radical cystectomy for bladder cancer in the USA. Eur Urol. 2018;73:374–82.
Brooks GA, Li L, Sharma DB, Weeks JC, Hassett MJ, Yabroff KR, et al. Regional variation in spending and survival for older adults with advanced cancer. J Natl Cancer Inst. 2013;105:634–42.
Ellimoottil C, Miller DC. Anticipating the effect of the Patient Protection and Affordable Care Act for patients with urologic cancer. Urol Oncol. 2014;32:55–8.
Nguyen PL, Gu X, Lipsitz SR, Choueiri TK, Choi WW, Lei Y, et al. Cost implications of the rapid adoption of newer technologies for treating prostate cancer. J Clin Oncol. 2011;29:1517–24.
Cole AP, Leow JJ, Chang SL, Chung BI, Meyer CP, Kibel AS, et al. Surgeon and hospital level variation in the costs of robot-assisted radical prostatectomy. J Urol. 2016;196:1090–5.
Aizer AA, Gu X, Chen MH, Choueiri TK, Martin NE, Efstathiou JA, et al. Cost implications and complications of overtreatment of low-risk prostate cancer in the United States. J Natl Compr Canc Netw. 2015;13:61–8.
Hollenbeck BK, Kaufman SR, Borza T, Yan P, Herrel LA, Miller DC, et al. Accountable care organizations and prostate cancer care. Urol Pract. 2017;4:454–61.
Luckenbaugh AN, Hollenbeck BK, Kaufman SR, Yan P, Herrel LA, Skolarus TA, et al. Impact of accountable care organizations on diagnostic testing for prostate cancer. Urology. 2018;116:68–75.
Trinh QD, Sun M, Krasnova A, Ramaswamy A, Cole AP, Fletcher S, et al. Impact of accountable care organizations on prostate cancer screening & biopsies in the United States. Urol Pract. 2018. https://doi.org/10.1016/j.urpr.2018.07.003. [Epub ahead of print].
Borza T, Kaufman SR, Yan P, Herrel LA, Luckenbaugh AN, Miller DC, et al. Early effect of Medicare Shared Savings Program accountable care organization participation on prostate cancer care. Cancer . 2018;124:563–70.
Cole AP, Friedlander DF, Trinh QD Secondary data sources for health services research in urologic oncology. Urol Oncol. 2018;36:165.
Brown ML, Riley GF, Schussler N, Etzioni R. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care. 2002;40:IV104–IV117.
Trinh QD, Bianchi M, Sun M, Sammon J, Schmitges J, Shariat SF, et al. Discharge patterns after radical prostatectomy in the United States of America. Urol Oncol. 2013;31:1022–32.
Lustig A, Ogden M, Brenner RW, Penso J, Westrich KD, Dubois RW. The central role of physician leadership for driving change in value-based care environments. J Manag Care Spec Pharm. 2016;22:1116–22.
Cole AP, Trinh QD. Secondary data analysis: techniques for comparing interventions and their limitations. Curr Opin Urol. 2017;27:354–9.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34:3661–79.
Hawken SR, Herrel LA, Ellimoottil C, Montgomery ZA, Ye Z, Miller DC. Understanding pre-enrollment surgical outcomes for hospitals participating in Medicare Accountable Care Organizations. Am J Surg. 2016;211:998–1004.
Borza T, Oerline MK, Skolarus TA, Norton EC, Dimick JB, Jacobs BL, et al. Association between hospital participation in medicare shared savings program accountable care organizations and readmission following major surgery. Ann Surg. 2018. https://doi.org/10.1097/SLA.0000000000002737. [Epub ahead of print].
Hawken SR, Herrel LA, Ellimoottil C, Ye Z, Hollenbeck BK, Miller DC. Urologist participation in medicare shared savings program accountable care organizations (ACOs). Urology. 2016;90:76–81.
Busch AB, Huskamp HA, McWilliams JM. Early efforts by medicare accountable care organizations have limited effect on mental illness care and management. Health Aff (Millwood). 2016;35:1247–56.
McWilliams JM, Najafzadeh M, Shrank WH, Polinski JM. Association of changes in medication use and adherence with accountable care organization exposure in patients with cardiovascular disease or diabetes. JAMA Cardiol. 2017;2:1019–23.
Miller HD. From volume to value: better ways to pay for health care. Health Aff (Millwood). 2009;28:1418–28.
Porter ME, Kaplan RS. How to pay for health care. Harv Bus Rev. 2016;94:18.
James BC, Poulsen GP. The Case for Capitation. (cover story). Harv Bus Rev. 2016;94:102–11.
Acknowledgements
Q.-D.T. is supported by the Brigham Research Institute Fund to Sustain Research Excellence, the Bruce A. Beal and Robert L. Beal Surgical Fellowship, the Genentech Bio-Oncology Career Development Award from the Conquer Cancer Foundation of the American Society of Clinical Oncology (grant # 10202), a Health Services Research pilot test grant from the Defense Health Agency, the Clay Hamlin Young Investigator Award from the Prostate Cancer Foundation (grant # 16YOUN20), and an unrestricted educational grant from the Vattikuti Urology Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Q.-D.T. reports honoraria from Astellas, Bayer, and Jannseen and research funding from Bayer and Intuitive Surgical. A.S.K. reports consulting fees from Profound, Janssen, and ConfirmMDX. T.K.C. has received research funding from Pfizer and has an advisory role at Pfizer, Novartis, GlaxoSmithKline, Genentech, and Bayer. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cole, A.P., Krasnova, A., Ramaswamy, A. et al. Prostate cancer in the medicare shared savings program: are Accountable Care Organizations associated with reduced expenditures for men with prostate cancer?. Prostate Cancer Prostatic Dis 22, 593–599 (2019). https://doi.org/10.1038/s41391-019-0138-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0138-1