Abstract
Background
Current data on post-discharge mortality and rehospitalization is still insufficient among in-hospital survivors of cardiogenic shock (CS), including acute myocardial infarction (AMI) and non-AMI survivors.
Methods
Patients with CS who survived after hospital discharge were selected from the Taiwan National Health Insurance Research Database. Each patient was followed up at 3-year intervals. Mortality and rehospitalization were analyzed using Kaplan-Meier curves and Cox regression models.
Results
There were 16,582 eligible patients. Of these, 42.4% and 57.6% were AMI-CS and non-AMI-CS survivors, respectively. The overall mortality and rehospitalization rates were considerably high, with reports of 7.0% and 22.1% at 30 days, 24.5% and 58.2% at 1 year, and 38.9% and 73.0% at 3 years, respectively, among in-hospital CS survivors. Cardiovascular (CV) problems caused approximately 40% mortality and 60% rehospitalization. Overall, the non-AMI-CS group had a higher mortality burden than the AMI-CS group owing to older age and a higher prevalence of comorbidities. In multivariable models, the non-AMI-CS group exhibited a lower risk of all-cause mortality (adjusted hazard ratio [aHR] 0.69, 95% confidence interval [CI] 0.60 to 0.78) and CV mortality (aHR 0.65, 95% CI 0.54 to 0.78) compared to the AMI-CS group. However, these risks diminished and even reversed after one year (aHR 1.13, 95% CI 1.03 to 1.25 for all-cause mortality; aHR 1.27, 95% CI 1.09 to 1.49 for CV mortality).This reversal was not observed in all-cause and CV rehospitalization. For rehospitalization, AMI-CS was associated with the risk of CV rehospitalization in the entire observation period (aHR:0.80, 95% CI:0.76–0.84).
Conclusions
In-hospital AMI-CS survivors had an increased risk of CV rehospitalization and 30-day mortality, whereas those with non-AMI-CS had a greater mortality risk after 1-year follow-up.
Similar content being viewed by others
Introduction
Reports from several countries suggest a rising burden of cardiogenic shock (CS) because of its steadily rising incidence and persistently growing expenditure [1,2,3,4]. Patients with CS develop severe circulatory system derangement and acute organ hypoperfusion. Reversing this critical condition requires multidisciplinary collaboration to provide sufficient circulatory and organ support, relieve myocardial ischemia, and limit complications. Recent CS studies have demonstrated modest improvements in prognosis during hospitalization [2,3,4]. This implies that more patients survive to be discharged and face another challenge in the post-acute period [2]. Indeed, some acute myocardial infarction (AMI) studies have suggested that patients with CS remained in the high-risk population for mortality and rehospitalization in subacute periods of approximately 30 days to 1 year [5,6,7]. This highlights the importance of understanding the features of short- and long-term prognoses in all patients with CS.
Post-acute management should be tailored individually by exploring the clinical and prognostic characteristics of the CS subgroups. For example, the clinical features of CS change depending on the etiology of AMI or non-AMI. In the past, AMI was thought to be the major cause of CS and was associated with a higher risk of in-hospital mortality [8,9,10]. Contemporary trends have demonstrated an increasing proportion of non-AMI-associated CS (non-AMI-CS) versus AMI complicated by CS (AMI-CS), and non-AMI is becoming the leading cause of CS in some regions [2, 11]. More therapeutic innovations with evidence in AMI-CS than in non-AMI-CS in the modern era reflect a more predominant survival improvement in AMI-CS [2]. Consequently, it is important to understand the differences in short- and long-term discharge outcomes between AMI-CS and non-AMI-CS to develop a clinical strategy accordingly.
We performed a nationwide cohort study of AMI and non-AMI in-hospital CS survivors using the National Health Insurance Research Database (NHIRD). We aimed to study short- and long-term mortality and rehospitalization in overall and subgroups of patients with CS based on the etiology.
Methods
Data source and study population
The study design was modified and extended from a published study, Cardiogenic Shock in Taiwan (CSiT) [2]. Data were extracted from the NHIRD in Taiwan. The NHIRD includes complete data on outpatient visits, hospital admissions, medication prescriptions, disease diagnoses, medical procedures, and vital statuses of 99% of Taiwan’s population. Diagnoses in the NHIRD have been coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes and ICD-10-CM since 2016. The NHIRD can be linked to the National Death Registry (NDR) by using the unique encrypted identification of each beneficiary. The accuracies of the NHIRD and NDR have been analyzed in previous studies [12, 13]. The study protocol was approved by the Institutional Review Board of MacKay Memorial Hospital (23MMHIS201e).
Our data period was between 2010 and 2020. To ensure patients could complete a three-year follow-up, individuals were selected if they had a diagnostic code for CS (ICD-9-CM of 785.51 and ICD-10-CM of R57.0) based on inpatient claims between January 1, 2011, and December 31, 2017, and survived hospital discharge. The exclusion criteria were the same as those in the previous study, including (1) no age or sex information (n = 60), (2) age < 18 years (n = 332), and (3) length of hospital stay > 365 days (n = 8). The last exclusion criterion remained because the rationale for a long hospital stay was uncertain. Patients who had a death record within two days after the date of hospital discharge were also excluded because of possible impending death discharge. We excluded patients with CS before 2011 to prevent the potential influence of the national AMI accreditation policy implemented in 2009 in the study region on mortality [2].
Mortality and rehospitalization
Death records were obtained from the NDR, a nationwide registry for the causes of death. In addition to all-cause mortality or rehospitalization, we assessed the impact of cardiovascular (CV) disease on outcomes and defined CV mortality and CV rehospitalization. The first ICD code assessed the primary cause of death.
Covariables
Most comorbidities observed in the current study, including hypertension, dyslipidemia, coronary artery disease, prior myocardial infarction (MI), renal failure, congestive heart failure, peripheral arterial disease, and atrial fibrillation, were associated with mortality. Patients were considered to have a specific condition if they had at least two diagnostic claims made during outpatient visits or one during hospital admission before the index date of the CS. Renal failure was identified by the National Catastrophic Illness Patient Registry, which provides substantial benefits regarding medical expenses. Medical procedures performed at CS admission were considered, including percutaneous coronary intervention (PCI); coronary artery bypass graft (CABG) and heart transplantation; and mechanical circulatory support (MCS) devices using intra-aortic balloon pumps (IABPs), extracorporeal membrane oxygenation (ECMO), and ventricular assist devices (VADs). Medications including angiotensin converting enzyme inhibitors/angiotensin II receptor antagonists (ACEI/ARB) and beta-blocker prescribed at the first outpatient clinic visit were evaluated and recorded. According to the medical capabilities, hospitals were divided into three levels (medical center, regional hospital and district hospital) and hospital levels were accredited regularly by the central health authorities, namely the Joint Commission of Taiwan and the Ministry of Health and Welfare [14]. In Taiwan, official regulations adhere to hospice palliative care guidelines established by the “Hospice Palliative Care Act” in 2000. The medical costs for hospice palliative mode have been covered by National Health Insurance since September 2009, and relevant records after discharge were assessed. Details of the disease diagnosis and treatment procedure codes were presented in Additional file 1.
Statistical analysis
We compared demographics, healthcare resource use, comorbidities, hospital level, and year of CS diagnosis between the two study cohorts (AMI vs. non-AMI). Quantitative variables are expressed as mean, and standard deviation, and qualitative variables are presented as absolute frequencies (number of patients) and relative frequencies (percentages). Two-sample t-tests were used to compare continuous variables between groups. The index hospital discharge date was the first day of follow-up. We used landmark analysis to show the time-varying prognosis of mortality and rehospitalization at 30 days and 1-year point since the prognostic impact of AMI-CS (or non-AMI-CS) was inconsistent. Those choices were informed by both data-driven selection, which involved identifying exponential curves that best fit the observed survival curve and including commonly used time points in the literature. Event-free survival was calculated using the Kaplan–Meier method. The hazard ratio (HR) for the Cox proportional hazards regression model was used along with the corresponding standard error, 95% confidence interval (CI), and p value. Baseline demographics, comorbidities, hospital level, index year, medications and cardiopulmonary resuscitation were included in the multivariable adjustment. AMI condition and cardiac procedures, including PCI, CABG, or heart transplantation, were not included for adjustment owing to the different disease pathological nature. We also excluded MCS for adjustment because of the inequalities in MCS use in the study region. As death is a competing event in evaluating the risk of rehospitalization, we performed a competing risk analysis and treated death as a competing risk. Statistical analyses were performed using SAS/STAT version 9.4 (SAS Institute, Cary, NC, USA). A p-value < 0.05 was considered statistically significant.
Results
Baseline characteristics
Between January 1, 2011, and December 31, 2017, 7,037 (42.4%) and 9,545 (57.6%) patients were AMI-CS and non-AMI-CS in-hospital survivors, respectively, and were followed up for 3 years. The prevalence of CS survivors after discharge gradually increased during the observation period (p for trend < 0.001) (Additional File 2). The baseline characteristics of the patients are shown in Table 1. Compared to patients with AMI-CS, those with non-AMI-CS were older and more likely to be female. They had a higher prevalence of congestive heart failure, hypertension, renal failure, stroke, malignancy, and atrial fibrillation, whereas no significant differences were found in diabetes, peripheral arterial disease, or VAD implementation. A higher percentage of non-AMI-CS patients were not treated in medical centers and they received less medications of ACEI/ARB and beta-blocker after hospital discharge. However, non-AMI CS survivors experienced fewer cardiac arrests, coronary interventions (PCI and CABG), and mechanical support (IABP and ECMO). The heart transplantation rate was borderline higher in the non-AMI-CS group than that in the AMI-CS group (0.6% vs. 0.4%; p = 0.054). According to records, there were 19.3% in-hospital survivors had hospice palliative cares during the entire follow up. Of them, 32.5% were AMI-CS and 67.5% were non-AMI-CS (Additional File 3).
Mortality
During the 3-year follow-up period, there were 6,449 deaths, accounting for 38.9% of the entire cohort, and 43.0% were due to CV etiologies (Table 2, Additional File 4). The mortality rates within 30 days, 1 year, and 3 years were 1,162 (7.0%), 4,062 (24.5%), and 6,449 (38.9%), respectively, for all-cause mortality, and 624 (3.8%), 1,863 (11.2%), and 2,774 (16.7%), respectively, for only CV reasons.
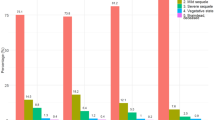
The Kaplan-Meier curves showed that the non-AMI-CS group was likely to have a more significant mortality burden based on total number and percentage than the AMI-CS group (Fig. 1A, B). The crude HRs at the three different follow-up intervals consistently showed a higher mortality risk (all-cause and CV) in the non-AMI-CS group than in the AMI-CS group. Based on landmark analysis, three-time intervals were identified: 1–30 days, 31–365 days, and 1–3 years. The adjusted mortality risks based on the CS etiology (AMI vs. non-AMI) appeared to vary throughout the follow-up time intervals. When considering the AMI-CS group as the reference, the adjusted hazard ratios (HRs) for all-cause mortality in the non-AMI-CS group were 0.69 (95% CI: 0.60–0.78) from 1 to 30 days, 1.00 (95% CI: 0.92–1.09) from 31 to 365 days, and 1.13 (95% CI: 1.03–1.25) from 1 to 3 years, indicating a reversal in risk after one year of follow-up. Similar patterns were observed for CV mortality (Table 3, Central Fig.).
Rehospitalization
Rehospitalization was frequently observed in hospital survivors of CS, ranging from 22% within 30 days to > 70% within 3 years of follow-up. More than 50% of these were due to CV etiologies (Table 2). Rehospitalization cases within 30 days, 1 year, and 3 years were 3,668 (22.1%), 9,651 (58.2%), and 12,101 (73.0%), respectively, for all-cause, and 2,036 (12.3%), 6,453 (38.9%), 8,651 (51.6%), respectively, for only CV reasons (Table 2).
The non-AMI-CS group appeared a greater burden of all-cause rehospitalization compared to the AMI-CS group (Fig. 2A). However, after adjusting covariables, the non-AMI-CS group had a lower risk of all-cause rehospitalization from 31 to 365d (HRs:0.86) compared to AMI-CS group (Table 3).
Three-year (A) all-cause and (B) cardiovascular rehospitalization. Kaplan-Meier curves showed that patients of non-AMI-CS had higher all-cause rehospitalization but lower cardiovascular rehospitalization compared with those of AMI-CS. Abbreviation: AMI: acute myocardial infarction, CS: cardiogenic shock
In-hospital survivors of non-AMI-CS were associated with a lower risk of CV rehospitalization throughout the follow-up period (Table 2; Fig. 2B). Considering the AMI-CS as reference, the adjusted HRs for the non-AMI-CS group were 0.87 (95% CI: 0.79–0.97, p = 0.009) from 1 to 30 days, 0.72 (95% CI: 0.67–0.77, p < 0.001) from 31 to 365 days, and 0.90 (95% CI:0.82-1.00, p = 0.046) from 1 to 3 years, respectively (Table 3).
Discussion
In this nationwide population-based study, we identified several clinical and prognostic issues among AMI and non-AMI in-hospital survivors of CS. First, both mortality and rehospitalization rates were high, increasing up to 24.5% and 38.9% within one and three years, respectively, for mortality and 58.2% and 73.0% within one and three years, respectively, for rehospitalization (Central Fig). Second, CV problems caused approximately 40% mortality and 60% rehospitalization. Third, in-hospital survivors with AMI-CS were associated with an increased risk of CV rehospitalization and mortality within 30 days (both all-cause and CV), whereas those with non-AMI-CS were at a higher risk of mortality after 1 year of follow-up (Central Fig).
Demographic changes and comparisons: AMI vs. Non-AMI
Although CS is a life-threatening condition associated with high in-hospital mortality, recent reports have shown declining mortality trends, probably reflecting the current therapeutic advances [2,3,4]. Based on our data, improvements in in-hospital survival were observed in both AMI and non-AMI patients. However, to the best of our knowledge, current studies have mainly focused on in-hospital CS survivors with AMI etiology and provided information limited to long-term outcomes. Our study provides broader features of the local region involving both AMI and non-AMI patients. Owing to the nature of the disease, individuals who had non-AMI-CS and survived to be discharged tended to be older and had more complex comorbidities. Simultaneously, those patients also had a relatively lower percentage of medical center hospitalization and MCS use due to local health policy for AMI [2]. This reflects the gap between the reality and ideal care mode of CS patients despite the guidelines and consensus recommended to centralize all eligible patients in a medical hub to offer comprehensive, collaborative, and multidisciplinary care [15,16,17]. A well-organized regional system can optimize resource allocation and facilitate early treatment. Consequently, the quality of care and prognosis can be improved [15,16,17,18]. Despite potential underestimation, near one fifth in-hospital survivors of CS received palliative programs. This percentage was higher than another study [19]. It is urgent to explore the cost-effectiveness and quality improvement after integrating palliative care in CS patients.
Mortality
Understanding specific reasons for mortality is essential for assessing the lifelong risks among in-hospital survival of CS and for designing a post-acute care model. With using first ICD code as the primary diagnosis, CV and respiratory reasons were the major causes of deaths during 3-year follow up (Additional File 4). However, it is imperative to exercise caution when interpreting these data due to the retrospective nature of the study design and the absence of chart reviews. Developing a well-defined prospective study to investigate the exact reason for death is ideal.
Overall, the non-AMI-CS group had a higher burden of mortality throughout the 3 years of follow-up. Our data are consistent with previous studies that showed that patients with AMI-CS were associated with a higher risk of 30-day mortality than those without AMI-CS after adjusting for baseline factors [9, 10]. The difference between crude and adjusted mortality could be partly explained by the increase in the percentage of “young patients with AMI” and the decline in the severity of AMI in recent years [20,21,22]. The lower severity of AMI was reflected in the lower overall mortality since individuals with non-AMI-CS were usually more fragile with complicated comorbidities, as shown in our data. Once the baseline differences were adjusted for, the AMI-CS group presented a higher risk of 30-day mortality than the non-AMI-CS group. Notably, the early mortality risk of AMI-CS attenuated gradually and was reversed after 1 year of follow-up. Landmark analysis showed that non-AMI-CS was an independent risk factor for all-cause and CV mortality in the time interval of 1–3 years. This finding supports the “AMI-CS storm” concept, which was once reported to last around half to 1 year [5, 6, 23]. Shah et al. investigated 112,668 AMI in-hospital survivors and found that those with AMI-CS (5%) were associated with higher all-cause mortality and rehospitalization in the first 60 days (adjusted HR:1.28; 95% CI:1.21 to 1.35) and the risk was similar thereafter (adjusted HR:0.95 for days 61 to 365; 95% CI:0.89 to 1.01) [5]. Aissaoui et al. also investigated an AMI registry comprising 99 shock and 3,312 non-shock patients. They found that patients with AMI-CS had a 2.8-times higher risk of mortality within 1 year than those without shock. However, the long-term (1–5 years) mortality risk did not differ between the two groups [6]. Hence, aggressive monitoring and intervention could be crucial and cost-effective for in-hospital survivors of AMI-CS during the subacute phase.
Rehospitalization
Shah et al. and Mahmoud et al. have showed an exceptionally high risk of 30-day rehospitalization among in-hospital survivors of CS for the AMI subgroup based on the data from the US [7, 24]. Approximately one-fifth of our data are consistent with their reports. Moreover, we demonstrated similar and high rehospitalization rates that persistently increased to 58% within 1 year and 73% within 3 years in the non-AMI subgroup. CV causes contribute to 50–60% of all rehospitalizations, which is close to but higher than reports from the US readmission dataset. Current guidelines suggest that multidisciplinary and patient-centered care after hospital discharge helps lower rehospitalization rates among high-risk populations such as those with AMI and heart failure [15, 25]. Considering the similar or even higher risk among patients with CS, initiating a post-acute care program to protect this fragile population is worthy and critical. For instance, most patients who recover from an acute illness experience predominant muscle weakness and polyneuropathy, known as intensive care unit-acquired weakness [26]. Active implementation of a rehabilitation program significantly improves patients’ activities and quality of life [27]. Indeed, a Danish survey of survivors of out-of-hospital cardiac arrest demonstrated that a considerable number of individuals had chronic physical health impairments, as assessed by the SF-12, until 20 years of follow up [28]. Moreover, respiratory, infection, and gastrointestinal factors are considered other important etiologies for rehospitalization, accounting for approximately 10% each [7, 24]. This implies persistently impaired organ function and self-care abilities when patients with CS return home. Comprehensive organ function assessment and tailored treatment should be individualized during the outpatient periods [16].
Clinical implication
Current risk scores for CS, such as CardShock, SAVE, modified SAVE, and ENCOURAGE, have mainly been proposed for short-term or in-hospital mortality and cannot be applied for long-term mortality [9, 29,30,31]. Some prognostic surrogates, such as AMI, seem to lose their ability to predict long-term mortality, as demonstrated in the present study. Moreover, valid prognostic scores for predicting rehospitalization remain lacking. Therefore, targeting different outcomes and follow-up periods is the next important task for improving risk discrimination.
During the recovery phase, in-hospital CS survivors frequently experience heart failure symptoms. Although several pharmacotherapies have shown clinical benefits in patients with heart failure, patients with CS have been excluded because of hemodynamic instability during index hospitalization [32, 33]. It is urgent to determine whether these promising medications are effective for both heart failure and post-acute care of CS.
Study limitations
Our study has several limitations. First, it was a nationwide claims-based cohort study conducted in real-world settings. The accuracy of disease diagnosis was based on discharge claims, as a review article reported that the positive predictive value of most diseases was in the 80–99% range [34]. Clinically relevant imaging and laboratory data were unavailable. Second, the study was conducted in Taiwan and may not be generalizable to other populations due to various factors such as differences in resource allocation, policy frameworks, and ethnic considerations [35]. Certain policies and treatment patterns in different countries may have influenced these results. Thus, replication of study designs is warranted. Third, we acknowledged the inability to adjust for disease heterogeneity (e.g., disease severity). Indeed, attempting to classify diverse etiologies encompassing the entire non-AMI CS patient cohort solely based on disease codes (ICD-9 or 10) presents considerable challenges and may introduce biases. Fourth, because terminal discharge (going home to die) is a well-adopted tradition in Taiwan, we excluded patients who died within 3 days after the index discharge date, which might have underestimated short-term (1–30 day) mortality. Finally, we did not differentiate the exact etiology of mortality or rehospitalization because some overlaps and uncertainty of the major diagnostic coding existed in the claims database, which biased the categorization.
Conclusions
The trend of in-hospital survivors with a diagnosis of CS is persistently increasing in Taiwan; non-AMI-CS plays an important role and accounts for nearly three-fifths of all cases. Compared with other high-risk diseases, mortality and rehospitalization among in-hospital survivors of CS are considerably high, with reports of 38.9% and 73.0% in 3 years, respectively, and CV problems remain a major cause. AMI-CS has time-varying prognostic effects. Patients with AMI-CS were associated with higher 30-day mortality, while such associations were attenuated and even reversed after a 1-year follow-up, suggesting that non-AMI-CS is a risk factor for long-term mortality. AMI-CS was an independent risk factor predicting CV rehospitalization. Risk stratification targeting different outcomes and timings is warranted, and requires further investigation.
Mortality and rehospitalization among in-hospital survivors of CS are considerably high, with reports of 39% and 73% in 3 years. AMI-CS has time-varying prognostic effects. Patients with AMI-CS were associated with higher 30-day mortality, while such associations were attenuated and even reversed after a 1-year follow-up, suggesting that non-AMI-CS is a risk factor for long-term mortality. Abbreviation: AMI: acute myocardial infarction, CS: cardiogenic shock
Data availability
This study used the National Health Insurance Research Database (NHIRD), a healthcare administrative claims data source provided by the Health and Welfare Data Center (HWDC) of Taiwan’s Ministry of Health and Welfare. The HWDC is a third-party organization to which researchers can submit applications for access to health-related databases. Owing to legal restrictions imposed by the government of Taiwan under the Personal Information Protection Act, data cannot be made publicly available. All HWDC data were fully anonymized before access was acquired. In addition, these data can only be accessed and analyzed in an independent operating area in the HWDC, and only statistical results can be released from that operational area. Therefore, the original data cannot be shared publicly, owing to legal restrictions.
Abbreviations
- CS:
-
Cardiogenic shock
- AMI:
-
Acute myocardial infarction
- AMI-CS:
-
Acute myocardial infarction-associated cardiogenic shock
- IABP:
-
Intra-aortic balloon pump
- VAD:
-
Ventricular assist device
- MCS:
-
Mechanical circulatory support
- NHI:
-
National Health Insurance
- NHIRD:
-
National Health Insurance Research Database
- ICD-9-CM:
-
International Classification of Diseases
- Ninth Revision:
-
Clinical Modification
- NDR:
-
National Death Registry
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- PCI:
-
Percutaneous coronary intervention
- CABG:
-
Coronary artery bypass graft
- ECMO:
-
Extracorporeal membrane oxygenation
References
Hunziker L, Radovanovic D, Jeger R, Pedrazzini G, Cuculi F, Urban P, et al. Twenty-year trends in the incidence and outcome of cardiogenic shock in AMIS Plus Registry. Circ Cardiovasc Interv. 2019;12(4):e007293.
Chien SC, Hsu CY, Liu HY, Lin CF, Hung CL, Huang CY, et al. Cardiogenic shock in Taiwan from 2003 to 2017 (CSiT-15 study). Crit Care. 2021;25(1):402.
Osman M, Syed M, Patibandla S, Sulaiman S, Kheiri B, Shah MK, et al. Fifteen-year trends in incidence of cardiogenic shock hospitalization and In-Hospital mortality in the United States. J Am Heart Assoc. 2021;10(15):e021061.
Lang CN, Kaier K, Zotzmann V, Stachon P, Pottgiesser T, von Zur Muehlen C, et al. Cardiogenic shock: incidence, survival and mechanical circulatory support usage 2007-2017-insights from a national registry. Clin Res Cardiol. 2021;110(9):1421–30.
Shah RU, de Lemos JA, Wang TY, Chen AY, Thomas L, Sutton NR, et al. Post-hospital outcomes of patients with Acute Myocardial Infarction with cardiogenic shock: findings from the NCDR. J Am Coll Cardiol. 2016;67(7):739–47.
Aissaoui N, Puymirat E, Simon T, Bonnefoy-Cudraz E, Angoulvant D, Schiele F, et al. Long-term outcome in early survivors of cardiogenic shock at the acute stage of myocardial infarction: a landmark analysis from the French registry of Acute ST-elevation and non-ST-elevation myocardial infarction (FAST-MI) Registry. Crit Care. 2014;18(5):516.
Shah M, Patil S, Patel B, Agarwal M, Davila CD, Garg L, et al. Causes and predictors of 30-Day readmission in patients with Acute myocardial infarction and cardiogenic shock. Circ Heart Fail. 2018;11(4):e004310.
Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving outcomes. Circulation. 2008;117(5):686–97.
Harjola VP, Lassus J, Sionis A, Køber L, Tarvasmäki T, Spinar J, et al. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail. 2015;17(5):501–9.
Schupp T, Rusnak J, Egner-Walter S, Ruka M, Dudda J, Bertsch T, et al. Prognosis of cardiogenic shock with and without acute myocardial infarction: results from a prospective, monocentric registry. Clin Res Cardiol. 2023. https://doi.org/10.1007/s00392-023-02196-2.
Shah M, Patnaik S, Patel B, Ram P, Garg L, Agarwal M, et al. Trends in mechanical circulatory support use and hospital mortality among patients with acute myocardial infarction and non-infarction related cardiogenic shock in the United States. Clin Res Cardiol. 2018;107(4):287–303.
Hsing AW, Ioannidis JP. Nationwide Population Science: lessons from the Taiwan National Health Insurance Research Database. JAMA Intern Med. 2015;175(9):1527–9.
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, et al. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349–58.
Ministry of Health and Welfare ROC. Taiwan Health and Welfare Report (2010–2017). https://www.mohw.gov.tw/lp-137-2.html.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720–826.
Tehrani BN, Truesdell AG, Psotka MA, Rosner C, Singh R, Sinha SS, et al. A standardized and Comprehensive Approach to the management of cardiogenic shock. JACC Heart Fail. 2020;8(11):879–91.
van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, et al. Contemporary Management of cardiogenic shock: a Scientific Statement from the American Heart Association. Circulation. 2017;136(16):e232–68.
Basir MB, Schreiber T, Dixon S, Alaswad K, Patel K, Almany S, et al. Feasibility of early mechanical circulatory support in acute myocardial infarction complicated by cardiogenic shock: the Detroit cardiogenic shock initiative. Catheter Cardiovasc Interv. 2018;91(3):454–61.
Feng Z, Fonarow GC, Ziaeian B. Palliative care services in patients admitted with cardiogenic shock in the United States: frequency and predictors of 30-day readmission. J Card Fail. 2021;27(5):560–720.
Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A, et al. Twenty Year trends and Sex differences in young adults hospitalized with Acute myocardial infarction. Circulation. 2019;139(8):1047–56.
Lee CH, Fang CC, Tsai LM, Gan ST, Lin SH, Li YH. Patterns of Acute myocardial infarction in Taiwan from 2009 to 2015. Am J Cardiol. 2018;122(12):1996–2004.
Myerson M, Coady S, Taylor H, Rosamond WD, Goff DC. Jr. Declining severity of myocardial infarction from 1987 to 2002: the atherosclerosis risk in communities (ARIC) Study. Circulation. 2009;119(4):503–14.
Kastrati A, Colleran R, Ndrepepa G. Cardiogenic shock: how long does the storm last? J Am Coll Cardiol. 2016;67(7):748–50.
Mahmoud AN, Elgendy IY, Mojadidi MK, Wayangankar SA, Bavry AA, Anderson RD et al. Prevalence, causes, and predictors of 30-Day readmissions following hospitalization with Acute Myocardial Infarction Complicated by cardiogenic shock: findings from the 2013–2014 National readmissions Database. J Am Heart Assoc. 2018;7(6).
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Hermans G, Van den Berghe G. Clinical review: intensive care unit acquired weakness. Crit Care. 2015;19(1):274.
Zorowitz RD, ICU-Acquired Weakness. A Rehabilitation perspective of diagnosis, treatment, and Functional Management. Chest. 2016;150(4):966–71.
Yonis H, Sørensen KK, Bøggild H, Ringgren KB, Malta Hansen C, Granger CB, et al. Long-term quality of Life after out-of-hospital cardiac arrest. JAMA Cardiol. 2023;8(11):1022–30.
Schmidt M, Burrell A, Roberts L, Bailey M, Sheldrake J, Rycus PT, et al. Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015;36(33):2246–56.
Chien SC, Lan WR, Wu SH, Chien CY, Chien YS, Lo CI, et al. Application and comparison of different prognostic Scoring systems in patients who underwent cardiologist-managed percutaneous cardiopulmonary support. Acta Cardiol Sin. 2020;36(4):326–34.
Muller G, Flecher E, Lebreton G, Luyt CE, Trouillet JL, Bréchot N, et al. The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive care med. 2016;42(3):370–8.
Pascual-Figal D, Wachter R, Senni M, Belohlavek J, Noè A, Carr D, et al. Rationale and design of TRANSITION: a randomized trial of pre-discharge vs. post-discharge initiation of sacubitril/valsartan. ESC Heart Fail. 2018;5(2):327–36.
Tromp J, Ponikowski P, Salsali A, Angermann CE, Biegus J, Blatchford J, et al. Sodium-glucose co-transporter 2 inhibition in patients hospitalized for acute decompensated heart failure: rationale for and design of the EMPULSE trial. Eur J Heart Fail. 2021;23(5):826–34.
Huang YT, Wei T, Huang YL, Wu YP, Chan KA. Validation of diagnosis codes in healthcare databases in Taiwan, a literature review. Pharmacoepidemiol Drug Saf. 2023;32(7):795–811.
Kim HK, Tantry US, Smith SC Jr., Jeong MH, Park SJ, Kim MH, et al. The east Asian paradox: an updated position statement on the challenges to the current antithrombotic strategy in patients with cardiovascular disease. Thromb Haemost. 2021;121(4):422–32.
Acknowledgements
The authors thank the Health and Clinical Research Data Center, Office of Data, Taipei Medical University and MacKay Memorial Hospital for their support. We are grateful to Professor Wei-Chun Huang for his help in the central figure. This manuscript was edited by Editage.
Funding
This study was funded by MacKay Memorial Hospital (MMH-109-100) and Clinical Research Data Center, Office of Data, Taipei Medical University.
Author information
Authors and Affiliations
Contributions
SCC and LNC conceived the study. CAW, HYL, CFL, and CYH acquired the data and HYL, CAW, and LNC performed the statistical analyses. SCC, CAW, and HYL edited the tables and figures. The first draft was written by SCC and CAW. All the authors participated in reviewing and revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved with a waiver of informed consent by the Institutional Review Board of MacKay Memorial Hospital (23MMHIS201e).
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was performed at the Health and Welfare Data Science Center (HWDC), Taipei Medical University Branch.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chien, SC., Wang, CA., Liu, HY. et al. Comparison of the prognosis among in-hospital survivors of cardiogenic shock based on etiology: AMI and Non-AMI. Ann. Intensive Care 14, 74 (2024). https://doi.org/10.1186/s13613-024-01305-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01305-2