Abstract
Purpose
To evaluate the feasibility of further reducing the incidence of occult endometrial cancer in women undergoing hysterectomy for benign gynecological indications.
Methods
Patients who underwent hysterectomies for presumed benign gynecologic conditions at Peking Union Medical College Hospital were retrospectively identified. Patients with occult endometrial cancer, which was defined as endometrial cancer diagnosed on postoperative histopathology with no preoperative confirmed malignancy, were selected.
Results
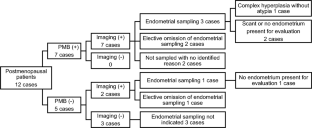
24/7558 (0.32%; 95% CI 0.20–0.47%) patients undergoing hysterectomy for benign indications had occult endometrial cancer. Asymptomatic patients with normal endometrial imaging all tended to have favorable pathology. Heavy menstrual bleeding was the most overlooked AUB pattern in the premenopausal group. In the postmenopausal group, all the patients with serous adenocarcinoma or G3 endometrioid adenocarcinoma histology/stage T1b disease/LVSI space invasion had a history of persistent or recurrent PMB ≥ 6 months and/or an intracavitary lesion > 20 mm in diameter. 3/4 of the samples of the postmenopausal patients did not have adequate endometrium for evaluation.
Conclusion
To further reduce the incidence of occult endometrial cancer, physicians should focus on the patient’s bleeding pattern and actively implement endometrial sampling whenever indicated. Transvaginal ultrasonography is a valuable preoperative evaluation. Hysteroscopy with directed biopsy is the preferred procedure in postmenopausal patients.

Similar content being viewed by others
Data availability
All available data are presented in this paper.
References
American College of, O. and Gynecologists, (2005) ACOG practice bulletin clinical management guidelines for obstetrician gynecologists, number 65, august 2005: management of endometrial cancer. Obstet Gynecol. https://doi.org/10.1097/00006250-200508000-00050
Kimura T et al (2004) Abnormal uterine bleeding and prognosis of endometrial cancer. Int J Gynaecol Obstet 85(2):145–150. https://doi.org/10.1016/j.ijgo.2003.12.001
Seebacher V et al (2009) The presence of postmenopausal bleeding as prognostic parameter in patients with endometrial cancer: a retrospective multi-center study. BMC Cancer 9:460. https://doi.org/10.1186/1471-2407-9-460
Tsakiridis I, Giouleka S, Koutsouki G, Kostakis N, Kalogiannidis I, Kourtis A, Athanasiadis A, Goulis DG, Dagklis T (2022) Investigation and management of abnormal uterine bleeding in reproductive-aged women: a descriptive review of national and international recommendations. Eur J Contracept Reprod Health Care 27(6):504–517. https://doi.org/10.1080/13625187.2022.2112169
Papakonstantinou E, Adonakis G (2022) Management of pre-, peri-, and post-menopausal abnormal uterine bleeding: when to perform endometrial sampling? Int J Gynaecol Obstet 158(2):252–259. https://doi.org/10.1002/ijgo.13988
Vitale SG, Buzzaccarini G, Riemma G, Pacheco LA, Di Spiezio SA, Carugno J, Chiantera V, Török P, Noventa M, Haimovich S, De Franciscis P, Perez-Medina T, Angioni S, Laganà AS (2023) Endometrial biopsy: indications, techniques and recommendations. an evidence-based guideline for clinical practice. J Gynecol Obstet Hum Reprod 52(6):102588. https://doi.org/10.1016/j.jogoh.2023.102588
Brun JL, Plu-Bureau G, Huchon C, Ah-Kit X, Barral M, Chauvet P, Cornelis F, Cortet M, Crochet P, Delporte V, Dubernard G, Giraudet G, Gosset A, Graesslin O, Hugon-Rodin J, Lecointre L, Legendre G, Maitrot-Mantelet L, Marcellin L, Miquel L, Le Mitouard M, Proust C, Roquette A, Rousset P, Sangnier E, Sapoval M, Thubert T, Torre A, Trémollières F, Vernhet-Kovacsik H, Vidal F, Marret H (2023) Management of women with abnormal uterine bleeding: clinical practice guidelines of the French National College of Gynaecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol 288:90–107. https://doi.org/10.1016/j.ejogrb.2023.07.001
Committee on Practice Bulletins—Gynecology (2012) Practice bulletin no: diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet Gynecol 120:197–206. https://doi.org/10.1097/AOG.0b013e318262e320
National Collaborating Centre for Women’s and Children’s Health (2007) Heavy Menstrual Bleeding. RCOG Press, London
Exceptional Surveillance of Heavy Menstrual Bleeding (2021) assessment and management (NICE guideline NG88) [Internet]. National Institute for Health and Care Excellence (NICE), London
Munro MG, Critchley HOD, Fraser IS, Menstrual Disorders Committee FIGO (2018) The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet 143(3):393–408. https://doi.org/10.1002/ijgo.12666
Farquhar CM, Lethaby A, Sowter M, Verry J, Baranyai J (1999) An evaluation of risk factors for endometrial hyperplasia in premenopausal women with abnormal menstrual bleeding. Am J Obstet Gynecol 181(3):525–529. https://doi.org/10.1016/s0002-9378(99)70487-4
Ash SJ, Farrell SA, Flowerdew G (1996) Endometrial biopsy in DUB. J Reprod Med 41(12):892–896
Farquhar CM (1999) An evidence-based guideline for the management of heavy menstrual bleeding. N Z Med J 112:174–177
MacGregor R, Jain V, Hillman S, Lumsden MA (2022) Investigating abnormal uterine bleeding in reproductive aged women. BMJ 16(378):e070906. https://doi.org/10.1136/bmj-2022-070906
Smith-Bindman R et al (1998) Endovaginal ultrasound to exclude endometrial cancer and other endometrial abnormalities. JAMA 280(17):1510–1517. https://doi.org/10.1001/jama.280.17.1510
Trimble CL et al (2006) Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: a gynecologic oncology group study. Cancer 106(4):812–819. https://doi.org/10.1002/cncr.21650
Theben JU et al (2013) Unexpected malignancies after laparoscopic-assisted supracervical hysterectomies (LASH): an analysis of 1584 LASH cases. Arch Gynecol Obstet 287(3):455–462. https://doi.org/10.1007/s00404-012-2559-0
Mahnert N et al (2015) Unexpected gynecologic malignancy diagnosed after hysterectomy performed for benign indications. Obstet Gynecol 125(2):397–405. https://doi.org/10.1097/AOG.0000000000000642
Takamizawa S et al (1999) Risk of complications and uterine malignancies in women undergoing hysterectomy for presumed benign leiomyomas. Gynecol Obstet Invest 48(3):193–196. https://doi.org/10.1159/000010172
Frick AC et al (2010) Risk of unanticipated abnormal gynecologic pathology at the time of hysterectomy for uterovaginal prolapse. Am J Obstet Gynecol 202:507. https://doi.org/10.1016/j.ajog.2010.01.077
Ramm O et al (2012) Utility of preoperative endometrial assessment in asymptomatic women undergoing hysterectomy for pelvic floor dysfunction. Int Urogynecol J 23(7):913–917. https://doi.org/10.1007/s00192-012-1694-2
Soliman PT, Oh JC, Schmeler KM, Sun CC, Slomovitz BM, Gershenson DM, Burke TW, Lu KH (2005) Risk factors for young premenopausal women with endometrial cancer. Obstet Gynecol 105(3):575–580. https://doi.org/10.1097/01.AOG.0000154151.14516.f7
Pennant ME, Mehta R, Moody P, Hackett G, Prentice A, Sharp SJ, Lakshman R (2017) Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 124(3):404–411. https://doi.org/10.1111/1471-0528.14385
Parsons LHP, Pedersen R, Richardson DL, Kho KA (2018) The prevalence of occult endometrial cancer in women undergoing hysterectomy for benign indications. Eur J Obstet Gynecol Reprod Biol 223:108–112. https://doi.org/10.1016/j.ejogrb.2018.02.017
Wagner P, Kommoss FKF, Kommoss S, Hartkopf AD, Pasternak I, Oberlechner E, Greif K, Wallwiener M, Neis F, Abele H, Krämer B, Reisenauer C, Staebler A, Wallwiener D, Brucker SY, Taran FA (2019) Unexpected malignant uterine pathology: Incidence, characteristics and outcome in a large single-center series of hysterectomies for presumed benign uterine disease. Gynecol Oncol 153(1):49–54. https://doi.org/10.1016/j.ygyno.2018.12.026
Funding
This work was supported by a grant from National High Level Hospital Clinical Research Funding (2022-PUMCH-C-031).
Author information
Authors and Affiliations
Contributions
HHS and YC contributed to the study conception and design. Material preparation, data collection and analysis were performed by YC and XPZ. The first draft of the manuscript was written by YC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Peking Union Medical College Hospital (reference no: I-22PJ848).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, Y., Shi, H. & Zhuo, X. Occult endometrial cancer in women undergoing hysterectomy for benign indications: a retrospective cohort study in a tertiary hospital in China. Arch Gynecol Obstet (2024). https://doi.org/10.1007/s00404-024-07532-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-024-07532-z