Abstract
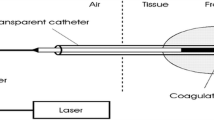
Haemorrhoidal disease is identified by declension of the inflamed and bleeding of vascular tissues of the anal canal. Traditionally, haemorrhoids are associated with chronic constipation and the most common symptoms are irritation in anus region, pain and discomfort, swelling around anus, tender lumps around the anus and rectal bleeding (depending upon the grade of haemorrhoid). Among the several conventional treatment procedures (commonly mentioned as, rubber band litigation, sclerotherapy and electrotherapy), laser haemorrhoidoplasty is an out-patient and less-invasive laparoscopic procedure. From literature survey it has been observed that an exclusive theoretical model depicting the impact of 1064 nm wavelength laser wave on living tissues subjected to haemorrhoid therapy is not available. This research work is a pioneering attempt to develop a theoretical study attributing specifically on laser therapy of haemorrhoid treatment based on Pennes’ biological heat transfer model. The corresponding mathematical model has been solved by analytical method to establish thermal response of tissue during the treatment and also the same has been solved a numerical approach based on finite difference method to validate the feasibility of former method due to unavailability of any theoretical model. Impact of variation of blood perfusion term, laser pulse time and optical penetration depth on temperature response of skin tissue is captured. The tissue temperature decreases along with time of laser exposure with increasing the blood perfusion rate as it carries away large amount of heat. With the increase in laser pulse time, tissue temperature declines due to shorter pulse time resulting in higher energy consumed by electrons. The research outcome is successfully validated with less than 1% of error observed between the appointed analytical and numerical scheme.





Similar content being viewed by others
Data availability
The data presented in this study are available on request to the corresponding author.
Abbreviations
- A:
-
Non-dimensional constant term; refer Eq. (7)
- c:
-
Specific heat (J kg−1 °C−1); refer Eq. (1)
- Ci :
-
Non-dimensional unknown constant of the solution of differential equation; refer Eq. (14)
- \(\overline{{\text{F}} }\) :
-
Non-dimensional time; see Eq. (7)
- Fp :
-
Non-dimensional laser pulse time; refer Eq. (7)
- F:
-
Transformed time function (F) based on Duhamel’s theorem; refer Eq. (9)
- I0 :
-
Laser power input (J m−2); refer Eq. (2)
- I0*:
-
Non-dimensional laser power input; refer Eq. (7)
- i:
-
Non-zero and non-negative integer, refer Eq. (11)
- k:
-
Thermal conductivity (W m−1 °C−1); refer Eq. (1)
- L:
-
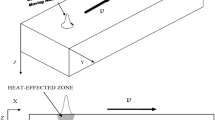
Length of the skin tissue domain (m); refer Fig. 1d
- n:
-
Nodal point representing as space in numerical solution; refer Eq. (20)
- p:
-
Assumed as nodal point representing as time in numerical solution; refer Eq. (20)
- Qmetabolic :
-
Metabolic heat generation term (J m−3), refer Eq. (1)
- Qexternal :
-
External heat generation term (J m−3); refer Eq. (1)
- ra, rf :
-
Absorptivity and reflectivity of skin tissue; refer Eq. (2)
- rd :
-
Laser absorption radius (m), refer Eq. (2)
- Rd :
-
Non-dimensional laser absorption radius; refer Eq. (7)
- t:
-
Time for laser heating (s), refer Eq. (1)
- tp :
-
Pulse laser time (s), refer Eq. (2)
- T:
-
Local temperature (°C); refer Eq. (1)
- x:
-
Spatial direction along the length of the tissue domain (m); refer Eq. (1)
- X:
-
Laser absorption radius spatial direction along the length of the tissue domain; refer Eq. (7)
- ω:
-
Blood perfusion term in Pennes’ bioheat model (s−1); refer Eq. (1)
- ρ:
-
Density (kg m−3); refer Eq. (1)
- δ:
-
Optical penetration depth (m); see Eq. (2)
- θ:
-
Non-dimensional local temperature; see Eq. (5)
- α:
-
Thermal diffusivity (m2 s−1); refer Eq. (1)
- \(\overline{\uptheta }\) :
-
Transformed non-dimensional local temperature based on Duhamel’s theorem; refer Eq. (8)
- μa :
-
Absorption coefficient (m−1) of optically cleared tissue; refer Eq. (2)
- μs :
-
Scattering coefficient (m−1) of optically cleared tissue; refer Eq. (2)
- t:
-
Tissue
- b:
-
Blood
References
Lohsiriwat V, Sheikh P, Bandolon R et al (2023) Recurrence Rates and Pharmacological Treatment for Hemorrhoidal Disease: A Systematic Review. Adv Ther 40:117–132
Hoef DVD (2023) Hogan A (2023) Haemorrhoidal artery ligation compared to alternative surgical techniques for the treatment of grade II-IV haemorrhoids: A systematic review. J Mind Med Sci 10(1):15–33
Lie H, Caesarini EF, Purnama AA et al (2022) Laser hemorrhoidoplasty for hemorrhoidal disease: a systematic review and meta-analysis. Laser Med Sci 37:3621–3630
Wee LJY, Koo CH, Seow-En I et al (2023) Laser hemorrhoidoplasty versus conventional hemorrhoidectomy for grade II/III aemorrhoids: a systematic review and meta-analysis. Annal Coloproct 39(1):15–33
Oostendorp JYV, Sluckin TC, Han-Geurts IJM et al (2023) Treatment of haemorrhoids: rubber band ligation or sclerotherapy (THROS)? Study protocol for a multicentre, non-inferiority, randomised controlled trial. Tri 24(374):1–8
Drissi F, Jean M-H, Abet E (2021) Evaluation of the efficacy and morbidity of radiofrequency thermocoagulation in the treatment of hemorrhoidal disease. J Visc Surge 158(5):385–389
Gupta PJ, Heda PS, Kalaskar S (2006) Radiofrequency Ablation and Plication – A New Technique For Prolapsing Hemorrhoidal Disease. Cur Surge 63(1):44–50
Aibuedefe B, Kling SM, Philp MM, Ross HM, Poggio JL (2021) An update on surgical treatment of hemorrhoidal disease: a systematic review and meta-analysis. Int J Colorectal Dis 36:2041–2059
De Nardi P, Maggi G, Pagnanelli M et al (2023) Hemorrhoid laser dearterialization: systematic review and meta-analysis. Laser Med Sci 38:54
Wang JY, Chang-Chien CR, Chen JS, Lai CR, Tang RP (1991) The role of lasers in hemorrhoidectomy. Dis Colon Rectum 34:78–82
Kim DY, Boushey RP (2007) The Use of Alternative Energy Sources and New Techniques for the Treatment of Hemorrhoidal Disease. Seminar Col Rect Surge 18(3):181–186
De FMOS, Dias SJA, Santos FMF, Sampaio CA (2016) Analysis of the main surgical techniques for haemorrhoids. J Coloproctol 36(2):104–114
Faes S, Pratsinis M, Hasler-Gehrer S, Keerl A, Nocito A (2019) Short- and long-term outcomes of laser haemorrhoidoplasty for grade II–III haemorrhoidal disease. Colorect Dis 21(6):689–696
Danys D, Pacevicius J, Makunaite G et al (2020) Tissue coagulation in laser hemorrhoidoplasty – an experimental study. Open Med 15:185–189
Longchamp G, Liot E, Meyer J et al (2021) Non-excisional laser therapies for hemorrhoidal disease: a systematic review of the literature. Laser Med Sci 36:485–496
Sofii I, Darmawan H, Kurniawan F et al (2022) A new technique for surgical haemorrhoidectomy without post-operative complication: A case series. Anal Med Surge 76:103467-1–103474
Tang C-Y, Roslani AC (2022) Laser ablation of anal fistulae: a 6-year experience in a tertiary teaching hospital in Malaysia. Laser Med Sci 37:3291–3296
Ram E, Kayzer M, Zager Y, Anteby R et al (2022) Laser hemorrhoidoplasty for II–IV grade aemorrhoids: should we treat them the same? Update Surg 75:635–642
Decker M, Sels T, Van Hoof S, Smets Q, Hendricks T, Dessel EV, Komen N (2023) Does minimally invasive laser-assisted treatment of pilonidal sinus disease live up to its expectations: a multi-center study with 226 patients. Int J Colorectal Dis 38:1–14
Romic I, Augustin G, Bogdanic B et al (2022) Laser treatment of pilonidal disease: a systematic review. Laser Med Sci 37:723–732
Elfallal AH, Fathy M, Elbaz SA, Emile SH (2022) Comprehensive literature review of the applications of surgical laser in benign anal conditions. Laser Med Sci 37:2775–2789
Pennes HH (1984) Analysis of tissue and arterial blood temperature in the resting forearm. J Appl Physiol 1(2):1–30
Majchrzak E, Mochnacki B (2023) Modelling of thin metal film heating using the dual-phase lag equation with temperature-dependent parameters. Int J Heat Mass Transf 209:124088-1–124111
Kabiri A, Talaee MR (2021) Thermal field and tissue damage analysis of moving laser in cancer thermal therapy. Laser Med Sci 36:583–597
Umarov SR, Saidamatov EM (2007) A generalization of Duhamel’s principle for differential equations of fractional order. Dokl Math 75:94–96
Dutta J, Biswas R, Kundu B (2020) Analytical solution of dual-phase-lag based heat transfer model in ultrashort pulse laser heating of A6061 and Cu3Zn2 nano film. Opt Laser Tech 128:106207-1–106210
Patankar SV (1980) Numerical Heat Transfer and Fluid Flow, 1st edn. CRC Press, Boca Raton, p 9781315275130
He A, Chen M (2022) Sclerotherapy in hemorrhoids. Indian J Surg 20:1–5
Gupta K (2022) Laser Hemorrhoidoplasty. Laser in Proctology, Springer Singapore. 978-981-19-5825-0.
Boakye Y D, Mensah D O, Agyei EK et al (2023) Role of Medicinal Plants in the Treatment of Hemorrhoids. 1st Edn. Apple Academic Press: 9781003189749.
Eltejaei I, Balavand M, Mojra A (2021) Numerical analysis of non-Fourier thermal response of lung tissue based on experimental data with application in laser therapy. Comput Methods Progr Biomed 199:105905-1–105911
Becker S M, Kuznetsov A V (2015) Heat Transfer and Fluid Flow in Biological Processes. 1st Edn. Academic Press, 978–0–12–408077–5
Youn JI (2021) The Effect of an Optical Clearing Agent on Tissue Prior to 1064-nm Laser Therapy. Med Lasers. 10(3):146–152
Miyamoto H (2023) Minimally Invasive Treatment for Advanced Hemorrhoids. J Anus Rectum Colon 7(1):8–16
Acknowledgements
Not applicable.
Funding
No research funding or financial assistance is available for conducting this research work.
Author information
Authors and Affiliations
Contributions
This research work is carried out by Dr. Jaideep Dutta as the sole author. The details of author’s contribution (segment-wise) are as follows:
Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing original draft, Investigation, Methodology, Graphical analysis, Review & Editing, Resources, Supervision: Jaideep Dutta.
Corresponding author
Ethics declarations
I, the undersigned declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere.
I wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
I confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. I further confirm that the order of authors listed in the manuscript has been approved by me.
I confirm that I have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing I confirm that I have followed the regulations of our institutions concerning intellectual property.
I understand that the Corresponding Author is the sole contact for the Editorial process (including Editorial Manager and direct communications with the office). He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs. I confirm that I have provided a current, correct email address which is accessible by the Corresponding Author.
Competing interests
The author declares that he has no conflicts of interest in this work. The author declares that they he doesn’t have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dutta, J. Bio-thermal response during laser haemorrhoidoplasty: an exclusive analytical and numerical approach for theoretical investigation. Lasers Med Sci 39, 108 (2024). https://doi.org/10.1007/s10103-024-04046-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-04046-7