Abstract
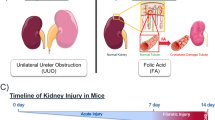
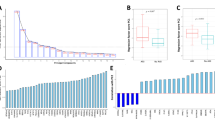
Acute kidney injury (AKI) poses a significant global public health challenge. Current methods for detecting AKI rely on monitoring changes in serum creatinine (Scr), blood urea nitrogen (BUN), urinary output and some commonly employed biomarkers. However, these indicators are usually neither specific nor sensitive to AKI, especially in cases of mild kidney injury. AKI is accompanied by severe inflammatory reactions, resulting in the upregulation of numerous inflammation-associated proteins in the plasma. Plasma biomarkers are a noninvasive method for detecting kidney injury, and to date, plasma inflammation-associated cytokines have not been adequately studied in AKI patients. The objective of our research was to identify novel inflammatory biomarkers for AKI. We utilized Olink proteomics to analyze the alterations in plasma inflammation-related proteins in the serum of healthy mice (n = 2) or mice treated with cisplatin (n = 6). Additionally, transcriptome datasets for the lipopolysaccharide (LPS), cisplatin, and ischemia‒reperfusion injury (IRI) groups were obtained from the National Center of Biotechnology Information (NCBI) Gene Expression Omnibus (GEO) database. We calculated the intersection of differentially expressed proteins (DEPs) and genes (DEGs) from both datasets. In the Olink proteomics analysis, the AKI group had significantly greater levels of 11 DEPs than did the control group. In addition, 56 common upregulated DEGs were obtained from the transcriptome dataset. The expression of CXCL1 and TNFRSF12A overlapped across all the datasets. The transcription and protein expression levels of CXCL1 and TNFRSF12A were detected in vivo. The gene and protein levels of CXCL1 and TNFRSF12A were significantly increased in different AKI mouse models and clinical patients, suggesting that these genes and proteins could be potential specific biomarkers for the identification of AKI.






Similar content being viewed by others
Availability of Data and Materials
The datasets of the current study are available from the corresponding author on reasonable request.
References
Hoste, E.A.J., J.A. Kellum, N.M. Selby, A. Zarbock, P.M. Palevsky, S.M. Bagshaw, et al. 2018. Global epidemiology and outcomes of acute kidney injury. Nature Reviews Nephrology 14 (10): 607–625. https://doi.org/10.1038/s41581-018-0052-0.
Kwiatkowska, E., L. Domanski, V. Dziedziejko, A. Kajdy, K. Stefanska, and S. Kwiatkowski. 2021. The mechanism of drug nephrotoxicity and the methods for preventing kidney damage. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms22116109.
Mesropian, P.D., J. Othersen, D. Mason, J. Wang, A. Asif, and R.O. Mathew. 2016. Community-acquired acute kidney injury: A challenge and opportunity for primary care in kidney health. Nephrology (Carlton, Vic.) 21 (9): 729–735. https://doi.org/10.1111/nep.12751.
Turgut, F., A.S. Awad, and E.M. Abdel-Rahman. 2023. Acute Kidney Injury: Medical Causes and Pathogenesis. Journal of Clinical Medicine. https://doi.org/10.3390/jcm12010375.
Harrill, A.H., H. Lin, J. Tobacyk, and J.C. Seely. 2018. Mouse population-based evaluation of urinary protein and miRNA biomarker performance associated with cisplatin renal injury. Experimental Biology and Medicine (Maywood, N.J.) 243 (3): 237–247. https://doi.org/10.1177/1535370217740854.
Bonavia, A., and K. Singbartl. 2018. A review of the role of immune cells in acute kidney injury. Pediatric Nephrology(Berlin, Germany) 33 (10): 1629–1639. https://doi.org/10.1007/s00467-017-3774-5.
Singbartl, K., C.L. Formeck, and J.A. Kellum. 2019. Kidney-Immune system crosstalk in AKI. Seminars in Nephrology 39 (1): 96–106. https://doi.org/10.1016/j.semnephrol.2018.10.007.
Kuo, P.Y., K.F. Tsai, P.J. Wu, P.C. Hsu, C.H. Wu, W.C. Lee, et al. 2023. Interleukin-18 and gelsolin are associated with acute kidney disease after cardiac catheterization. Biomolecules. https://doi.org/10.3390/biom13030487.
Farooqui, N., M. Zaidi, L. Vaughan, T.D. McKee, E. Ahsan, K.D. Pavelko, et al. 2023. Cytokines and immune cell phenotype in acute kidney injury associated with immune checkpoint inhibitors. Kidney International Reports 8 (3): 628–641. https://doi.org/10.1016/j.ekir.2022.11.020.
Kurts, C., U. Panzer, H.J. Anders, and A.J. Rees. 2013. The immune system and kidney disease: basic concepts and clinical implications. Nature Reviews Immunology 13 (10): 738–753. https://doi.org/10.1038/nri3523.
Bolisetty, S., and A. Agarwal. 2009. Neutrophils in acute kidney injury: not neutral any more. Kidney International 75 (7): 674–676. https://doi.org/10.1038/ki.2008.689.
Wang, X., K.C. Yip, A. He, J. Tang, S. Liu, R. Yan, et al. 2022. Plasma olink proteomics identifies CCL20 as a novel predictive and diagnostic inflammatory marker for preeclampsia. Journal of Proteome Research 21 (12): 2998–3006. https://doi.org/10.1021/acs.jproteome.2c00544.
Bao, X.H., B.F. Chen, J. Liu, Y.H. Tan, S. Chen, F. Zhang, et al. 2023. Olink proteomics profiling platform reveals non-invasive inflammatory related protein biomarkers in autism spectrum disorder. Frontiers in Molecular Neuroscience. https://doi.org/10.3389/fnmol.2023.1185021.
Gradin, A., H. Andersson, T. Luther, S.B. Anderberg, S. Rubertsson, M. Lipcsey, et al. 2021. Urinary cytokines correlate with acute kidney injury in critically ill COVID-19 patients. Cytokine. https://doi.org/10.1016/j.cyto.2021.155589.
Sun, B.B., J.C. Maranville, J.E. Peters, D. Stacey, J.R. Staley, J. Blackshaw, et al. 2018. Genomic atlas of the human plasma proteome. Nature 558 (7708): 73–79. https://doi.org/10.1038/s41586-018-0175-2.
Haslam, D.E., J. Li, S.T. Dillon, X. Gu, Y. Cao, O.A. Zeleznik, et al. 2022. Stability and reproducibility of proteomic profiles in epidemiological studies: comparing the Olink and SOMAscan platforms. Proteomics. https://doi.org/10.1002/pmic.202100170.
Wei, Q., and Z. Dong. 2012. Mouse model of ischemic acute kidney injury: technical notes and tricks. American Journal of Physiology. Renal Physiology 303 (11): F1487–F1494. https://doi.org/10.1152/ajprenal.00352.2012.
Xu, Y., H. Ma, J. Shao, J. Wu, L. Zhou, Z. Zhang, et al. 2015. A role for tubular necroptosis in cisplatin-induced AKI. Journal of the American Society of Nephrology 26 (11): 2647–2658. https://doi.org/10.1681/ASN.2014080741.
Chen, G.Y., and G. Nunez. 2010. Sterile inflammation: sensing and reacting to damage. Nature Reviews Immunology 10 (12): 826–837. https://doi.org/10.1038/nri2873.
Kaltenmeier, C., R. Wang, B. Popp, D. Geller, S. Tohme, and H.O. Yazdani. 2022. Role of immuno-inflammatory signals in liver ischemia-reperfusion injury. Cells. https://doi.org/10.3390/cells11142222.
Eltzschig, H.K., and T. Eckle. 2011. Ischemia and reperfusion–from mechanism to translation. Nature Medicine 17 (11): 1391–1401. https://doi.org/10.1038/nm.2507.
Stasi, A., A. Intini, C. Divella, R. Franzin, E. Montemurno, G. Grandaliano, et al. 2017. Emerging role of Lipopolysaccharide binding protein in sepsis-induced acute kidney injury. Nephrology, Dialysis, Transplantation 32 (1): 24–31. https://doi.org/10.1093/ndt/gfw250.
Peerapornratana, S., C.L. Manrique-Caballero, H. Gomez, and J.A. Kellum. 2019. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney International 96 (5): 1083–1099. https://doi.org/10.1016/j.kint.2019.05.026.
Vidya, M.K., V.G. Kumar, V. Sejian, M. Bagath, G. Krishnan, and R. Bhatta. 2018. Toll-like receptors: Significance, ligands, signaling pathways, and functions in mammals. International Reviews of Immunology 37 (1): 20–36. https://doi.org/10.1080/08830185.2017.1380200.
Chen, J.J., T.H. Lee, C.C. Lee, and C.H. Chang. 2021. Using lipocalin as a prognostic biomarker in acute kidney injury. Expert Review of Molecular Diagnostics 21 (5): 455–464. https://doi.org/10.1080/14737159.2021.1917384.
Hughes, C.E., and R.J.B. Nibbs. 2018. A guide to chemokines and their receptors. FEBS Journal 285 (16): 2944–2971. https://doi.org/10.1111/febs.14466.
Akcay, A., Q. Nguyen, Z. He, K. Turkmen, D. Won Lee, A.A. Hernando, et al. 2011. IL-33 exacerbates acute kidney injury. Journal of the American Society of Nephrology 22 (11): 2057–2067. https://doi.org/10.1681/ASN.2010091011.
Liu, P., X. Li, W. Lv, and Z. Xu. 2020. Inhibition of CXCL1-CXCR2 axis ameliorates cisplatin-induced acute kidney injury by mediating inflammatory response. Biomedicine & Pharmacotherapy. https://doi.org/10.1016/j.biopha.2019.109693.
Ciesielska, A., M. Matyjek, and K. Kwiatkowska. 2021. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cellular and Molecular Life Sciences 78 (4): 1233–1261. https://doi.org/10.1007/s00018-020-03656-y.
Akcay, A., Q. Nguyen, and C.L. Edelstein. 2009. Mediators of inflammation in acute kidney injury. Mediators of Inflammation. https://doi.org/10.1155/2009/137072.
Su, L., N. Li, H. Tang, Z. Lou, X. Chong, C. Zhang, et al. 2018. Kupffer cell-derived TNF-alpha promotes hepatocytes to produce CXCL1 and mobilize neutrophils in response to necrotic cells. Cell Death & Disease 9 (3): 323. https://doi.org/10.1038/s41419-018-0377-4.
Wiley, S.R., L. Cassiano, T. Lofton, T. Davis-Smith, J.A. Winkles, V. Lindner, et al. 2001. A novel TNF receptor family member binds TWEAK and is implicated in angiogenesis. Immunity 15 (5): 837–846. https://doi.org/10.1016/s1074-7613(01)00232-1.
Wiley, S.R., and J.A. Winkles. 2003. TWEAK, a member of the TNF superfamily, is a multifunctional cytokine that binds the TweakR/Fn14 receptor. Cytokine & Growth Factor Reviews 14 (3–4): 241–249. https://doi.org/10.1016/s1359-6101(03)00019-4.
Sanz, A.B., M.D. Sanchez-Nino, and A. Ortiz. 2011. TWEAK, a multifunctional cytokine in kidney injury. Kidney International 80 (7): 708–718. https://doi.org/10.1038/ki.2011.180.
Feng, S.L., Y. Guo, V.M. Factor, S.S. Thorgeirsson, D.W. Bell, J.R. Testa, et al. 2000. The Fn14 immediate-early response gene is induced during liver regeneration and highly expressed in both human and murine hepatocellular carcinomas. American Journal of Pathology 156 (4): 1253–1261. https://doi.org/10.1016/S0002-9440(10)64996-6.
Justo, P., A.B. Sanz, M.D. Sanchez-Nino, J.A. Winkles, C. Lorz, J. Egido, et al. 2006. Cytokine cooperation in renal tubular cell injury: the role of TWEAK. Kidney International 70 (10): 1750–1758. https://doi.org/10.1038/sj.ki.5001866.
Tirnitz-Parker, J.E., C.S. Viebahn, A. Jakubowski, B.R. Klopcic, J.K. Olynyk, G.C. Yeoh, et al. 2010. Tumor necrosis factor-like weak inducer of apoptosis is a mitogen for liver progenitor cells. Hepatology 52 (1): 291–302. https://doi.org/10.1002/hep.23663.
Hotta, K., M. Sho, I. Yamato, K. Shimada, H. Harada, T. Akahori, et al. 2011. Direct targeting of fibroblast growth factor-inducible 14 protein protects against renal ischemia reperfusion injury. Kidney International 79 (2): 179–188. https://doi.org/10.1038/ki.2010.379.
Meighan-Mantha, R.L., D.K. Hsu, Y. Guo, S.A. Brown, S.L. Feng, K.A. Peifley, et al. 1999. The mitogen-inducible Fn14 gene encodes a type I transmembrane protein that modulates fibroblast adhesion and migration. Journal of Biological Chemistry 274 (46): 33166–33176. https://doi.org/10.1074/jbc.274.46.33166.
Munoz-Garcia, B., J.L. Martin-Ventura, E. Martinez, S. Sanchez, G. Hernandez, L. Ortega, et al. 2006. Fn14 is upregulated in cytokine-stimulated vascular smooth muscle cells and is expressed in human carotid atherosclerotic plaques: modulation by atorvastatin. Stroke 37 (8): 2044–2053. https://doi.org/10.1161/01.STR.0000230648.00027.00.
Sanz, A.B., M.D. Sanchez-Nino, M.C. Izquierdo, A. Jakubowski, P. Justo, L.M. Blanco-Colio, et al. 2009. Tweak induces proliferation in renal tubular epithelium: a role in uninephrectomy induced renal hyperplasia. Journal of Cellular and Molecular Medicine 13 (9B): 3329–3342. https://doi.org/10.1111/j.1582-4934.2009.00766.x.
Donohue, P.J., C.M. Richards, S.A. Brown, H.N. Hanscom, J. Buschman, S. Thangada, et al. 2003. TWEAK is an endothelial cell growth and chemotactic factor that also potentiates FGF-2 and VEGF-A mitogenic activity. Arteriosclerosis, Thrombosis, and Vascular Biology 23 (4): 594–600. https://doi.org/10.1161/01.ATV.0000062883.93715.37.
Sanz, A.B., P. Justo, M.D. Sanchez-Nino, L.M. Blanco-Colio, J.A. Winkles, M. Kreztler, et al. 2008. The cytokine TWEAK modulates renal tubulointerstitial inflammation. Journal of the American Society of Nephrology 19 (4): 695–703. https://doi.org/10.1681/ASN.2007050577.
Gao, H.X., S.R. Campbell, L.C. Burkly, A. Jakubowski, I. Jarchum, B. Banas, et al. 2009. TNF-like weak inducer of apoptosis (TWEAK) induces inflammatory and proliferative effects in human kidney cells. Cytokine 46 (1): 24–35. https://doi.org/10.1016/j.cyto.2008.12.001.
Campbell, S., L.C. Burkly, H.X. Gao, J.W. Berman, L. Su, B. Browning, et al. 2006. Proinflammatory effects of TWEAK/Fn14 interactions in glomerular mesangial cells. The Journal of Immunology 176 (3): 1889–1898. https://doi.org/10.4049/jimmunol.176.3.1889.
Mesleh, A.G., S.A. Abdulla, and O. El-Agnaf. 2021. Paving the way toward personalized medicine: Current advances and challenges in Multi-OMICS approach in autism spectrum disorder for biomarkers discovery and patient stratification. Journal of Personalized Medicine. https://doi.org/10.3390/jpm11010041.
Cameron, G.J.M., K.M. Cautivo, S. Loering, S.H. Jiang, A.V. Deshpande, P.S. Foster, et al. 2019. Group 2 innate lymphoid cells are redundant in experimental renal ischemia-reperfusion injury. Frontiers in Immunology 10: 826. https://doi.org/10.3389/fimmu.2019.00826.
Lin, F., L. Xu, R. Yuan, S. Han, J. Xie, K. Jiang, et al. 2022. Identification of inflammatory response and alternative splicing in acute kidney injury and experimental verification of the involvement of RNA-binding protein RBFOX1 in this disease. International Journal of Molecular Medicine. https://doi.org/10.3892/ijmm.2022.5087.
Poveda, J., L.C. Tabara, B. Fernandez-Fernandez, C. Martin-Cleary, A.B. Sanz, R. Selgas, et al. 2013. TWEAK/Fn14 and non-canonical NF-kappaB signaling in kidney disease. Frontiers in Immunology 4: 447. https://doi.org/10.3389/fimmu.2013.00447.
Sanz, A.B., O. Ruiz-Andres, M.D. Sanchez-Nino, M. Ruiz-Ortega, A.M. Ramos, and A. Ortiz. 2016. Out of the TWEAKlight: elucidating the role of Fn14 and TWEAK in acute kidney injury. Seminars in Nephrology 36 (3): 189–198. https://doi.org/10.1016/j.semnephrol.2016.03.006.
Wik, L., N. Nordberg, J. Broberg, J. Bjorkesten, E. Assarsson, S. Henriksson, et al. 2021. Proximity extension assay in combination with next-generation sequencing for high-throughput proteome-wide analysis. Molecular and Cellular Proteomics. https://doi.org/10.1016/j.mcpro.2021.100168.
Acknowledgements
We thank the Laboratory Animal Center, Fifth Hospital of Shanxi Medical University (Shanxi Provincial People’s Hospital) for providing the experimental mice and their housing conditions.
Funding
This work was supported by the Key Laboratory Construction Plan Project of Shanxi Provincial Health Commission (2023035), Natural Science Foundation of Shanxi Province (202203021222359), Key Medical Research Project of Shanxi Province (2022XM30) and Shanxi Administration of Traditional Chinese Medicine Scientific research project (2023ZYYC2031).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: LL G. Analyzed the data: XY L and XY Z. Drafted the manuscript: XY L. Performed the experiments: XY L, XY Z, X Z, HX K, HJ G, LL L and YH M. Collection of serum from AKI patients: XB P. Contributed reagents/materials: RS L and LL G. Reviewed and edited the manuscript: LL G. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study protocol was approved by the Ethics Committee of Shanxi Provincial People's Hospital, and informed consent was obtained from all patients and their families in strict compliance with the Declaration of Helsinki (approved no. 2023–438). This experimental procedure and animal use protocol were approved by the Ethics Committee of Shanxi Provincial People's Hospital (approved no. 2023–439).
Competing Interests
The authors declare no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X., Zhou, X., Ping, X. et al. Combined Plasma Olink Proteomics and Transcriptomics Identifies CXCL1 and TNFRSF12A as Potential Predictive and Diagnostic Inflammatory Markers for Acute Kidney Injury. Inflammation (2024). https://doi.org/10.1007/s10753-024-01993-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10753-024-01993-9