Abstract
The purpose is to assess the efficacy of rose bengal photodynamic antimicrobial therapy (PDAT) using different irradiation energy levels and photosensitizer concentrations for the inhibition of fungal keratitis isolates. Seven different fungi (Aspergillus fumigatus, Candida albicans, Curvularia lunata, Fusarium keratoplasticum, Fusarium solani, Paecilomyces variotii, and Pseudallescheria boydii) were isolated from patients with confirmed infectious keratitis. Experiments were performed in triplicate with suspensions of each fungus exposed to different PDAT parameters including a control, green light exposure of 5.4 J/cm2, 2.7 J/cm2 (continuous and pulsed), and 1.8 J/cm2 and rose bengal concentrations of 0.1%, 0.05%, and 0.01%. Plates were photographed 72 h after experimentation, and analysis was performed to assess fungal growth inhibition. PDAT using 5.4 J/cm2 of irradiation and 0.1% rose bengal completely inhibited growth of five of the seven fungal species. Candida albicans and Fusarium keratoplasticum were the most susceptible organisms, with growth inhibited with the lowest fluence and minimum rose bengal concentration. Fusarium solani, Pseudallescheria boydii, and Paecilomyces variotii were inhibited by lower light exposures and photosensitizer concentrations. Aspergillus fumigatus and Curvularia lunata were not inhibited by any PDAT parameters tested. Continuous and pulsed irradiation using 2.7 J/cm2 produced similar results. Rose bengal PDAT successfully inhibits the in vitro growth of five fungi known to cause infectious keratitis. Differences in growth inhibition of the various fungi to multiple PDAT parameters suggest that susceptibilities to PDAT are unique among fungal species. These findings support modifying PDAT parameters based on the infectious etiology.



Similar content being viewed by others
References
Jeng BH (2017) Challenges in the management of fungal keratitis. JAMA Ophthalmol 135:525. https://doi.org/10.1001/jamaophthalmol.2017.0722
Miller D (2017) Update on the epidemiology and antibiotic resistance of ocular infections. Middle East Afr J Ophthalmol 24:30–42. https://doi.org/10.4103/meajo.MEAJO_276_16
Lalitha P, Prajna NV, Manoharan G et al (2015) Trends in bacterial and fungal keratitis in South India, 2002–2012. Br J Ophthalmol 99:192–194. https://doi.org/10.1136/bjophthalmol-2014-305000
Austin A, Lietman T, Rose-Nussbaumer J (2017) Update on the management of infectious keratitis. Ophthalmology 124:1678–1689
Gopinathan U, Garg P, Fernandes M et al (2002) The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India. Cornea 21:555–559. https://doi.org/10.1097/00003226-200208000-00004
Prajna NV, Srinivasan M, Mascarenhas J et al (2019) Visual impairment in fungal versus bacterial corneal ulcers 4 years after successful antimicrobial treatment. Am J Ophthalmol 204:124–129. https://doi.org/10.1016/j.ajo.2019.03.010
Bourcier T, Sauer A, Dory A et al (2017) Fungal keratitis. J Fr Ophtalmol 40:e307–e313
Mahmoudi S, Masoomi A, Ahmadikia K et al (2018) Fungal keratitis: an overview of clinical and laboratory aspects. Mycoses. https://doi.org/10.1111/myc.12822
Venkatesh Prajna N, Krishnan T, Mascarenhas J et al (2013) The mycotic ulcer treatment trial: A randomized trial comparing natamycin vs voriconazole. JAMA Ophthalmol 131:422–429. https://doi.org/10.1001/jamaophthalmol.2013.1497
Prajna NV, Krishnan T, Rajaraman R et al (2017) Adjunctive oral voriconazole treatment of fusarium keratitis a secondary analysis from the mycotic ulcer treatment trial II. JAMA Ophthalmol 135:520–525. https://doi.org/10.1001/jamaophthalmol.2017.0616
Sav H, Ozdemir HG, Altınbas R et al (2016) Virulence attributes and antifungal susceptibility profile of opportunistic fungi isolated from ophthalmic infections. Mycopathologia 181:653–661. https://doi.org/10.1007/s11046-016-0018-3
Jackson BE, Wilhelmus KR, Hube B (2007) The role of secreted aspartyl proteinases in Candida albicans keratitis. Invest Ophthalmol Vis Sci 48:3559–3565. https://doi.org/10.1167/iovs.07-0114
Zhu WS, Wojdyla K, Donlon K et al (1990) Extracellular proteases of Aspergillus flavus: fungal keratitis, proteases, and pathogenesis. Diagn Microbiol Infect Dis 13:491–497. https://doi.org/10.1016/0732-8893(90)90081-6
Wilhelmus KR, Jones DB (2001) Curvularia keratitis. Trans Am Ophthalmol Soc 99:111–30 discussion 130-2
Halili F, Arboleda A, Durkee H et al (2016) Rose bengal- and riboflavin-mediated photodynamic therapy to inhibit methicillin-resistant Staphylococcus aureus keratitis isolates. Am J Ophthalmol 166:194–202. https://doi.org/10.1016/j.ajo.2016.03.014
Durkee H, Arboleda A, Aguilar MC et al (2019) Rose bengal photodynamic antimicrobial therapy to inhibit Pseudomonas aeruginosa keratitis isolates. Lasers Med Sci. https://doi.org/10.1007/s10103-019-02871-9
Adre E, Durkee H, Arboleda A et al (2022) Rose bengal and riboflavin mediated photodynamic antimicrobial therapy against selected South Florida Nocardia keratitis isolates. Transl Vis Sci Technol 11. https://doi.org/10.1167/TVST.11.1.29
Arboleda A, Miller D, Cabot F et al (2014) Assessment of rose bengal versus riboflavin photodynamic therapy for inhibition of fungal keratitis isolates. Am J Ophthalmol 158:64-70.e2. https://doi.org/10.1016/j.ajo.2014.04.007
Amescua G, Arboleda A, Nikpoor N et al (2017) Rose bengal photodynamic antimicrobial therapy: a novel treatment for resistant fusarium keratitis. Cornea 36:1141–1144. https://doi.org/10.1097/ICO.0000000000001265
Atalay HT, Dogruman-Al F, Sarzhanov F et al (2018) Effect of riboflavin/rose bengal-mediated PACK-CXL on Acanthamoeba trophozoites and cysts in vitro. Curr Eye Res 43:1322–1325. https://doi.org/10.1080/02713683.2018.1501074
Zhu H, Alt C, Webb RH et al (2016) Corneal crosslinking with rose bengal and green light: efficacy and safety evaluation. Cornea 35:1234–1241. https://doi.org/10.1097/ICO.0000000000000916
Gallego-Muñoz P, Ibares-Frías L, Lorenzo E et al (2017) Corneal wound repair after rose bengal and green light crosslinking: clinical and histologic study. Invest Ophthalmol Vis Sci 58:3471–3480. https://doi.org/10.1167/iovs.16-21365
Naranjo A, Pelaez D, Arrieta E et al (2019) Cellular and molecular assessment of rose bengal photodynamic antimicrobial therapy on keratocytes, corneal endothelium and limbal stem cell niche. Exp Eye Res 188. https://doi.org/10.1016/j.exer.2019.107808
Naranjo A, Arboleda A, Martinez JD et al (2019) Rose bengal photodynamic antimicrobial therapy for patients with progressive infectious keratitis: a pilot clinical study. Am J Ophthalmol 208:387–396. https://doi.org/10.1016/j.ajo.2019.08.027
Sepulveda-Beltran PA, Levine H, Altamirano DS et al (2022) Rose bengal photodynamic antimicrobial therapy: a review of the intermediate-term clinical and surgical outcomes. Am J Ophthalmol 243:125–134. https://doi.org/10.1016/J.AJO.2022.08.004
Peterson JC, Arrieta E, Ruggeri M et al (2020) Detection of singlet oxygen luminescence for experimental corneal rose bengal photodynamic antimicrobial therapy. Research Article 12. https://doi.org/10.1364/BOE.405601
Bagga B, Sharma S, Ahirwar LK et al (2022) Clinical outcomes of rose bengal mediated photodynamic antimicrobial therapy on fungal keratitis with their microbiological and pathological correlation. Curr Eye Res 47:987–994. https://doi.org/10.1080/02713683.2022.2058019
Gómez BL, Nosanchuk JD (2003) Melanin and fungi. Curr Opin Infect Dis 16:91–96
Kang MJ, Hwang J, Chung SH (2021) Comparison of pulsed and continuous accelerated corneal crosslinking for keratoconus: 1-year results at a single center. J Cataract Refract Surg 47:641–648. https://doi.org/10.1097/J.JCRS.0000000000000488
Bogdanov A, Klimenko V, Verlov N et al (2019) Pulse mode irradiation regimen of PDT results in high progression free and overall survival in mice with model tumour. Ann Oncol 30:v21. https://doi.org/10.1093/ANNONC/MDZ238.073
Wiegell SR, Petersen B, Wulf HC (2016) Pulse photodynamic therapy reduces inflammation without compromising efficacy in the treatment of multiple mild actinic keratoses of the face and scalp: a randomized clinical trial. Br J Dermatol 174:979–984. https://doi.org/10.1111/bjd.14465
Kato IT, Prates RA, Sabino CP et al (2013) Antimicrobial photodynamic inactivation inhibits Candida albicans virulence factors and reduces in vivo pathogenicity. Antimicrob Agents Chemother 57:445–451. https://doi.org/10.1128/AAC.01451-12
Pereira CA, Domingues N, Silva MP et al (2015) Photodynamic inactivation of virulence factors of Candida strains isolated from patients with denture stomatitis. J Photochem Photobiol B 153:82–89. https://doi.org/10.1016/J.JPHOTOBIOL.2015.08.029
Cherfan D, Verter EE, Melki S et al (2013) Collagen cross-linking using rose bengal and green light to increase corneal stiffness. Investig Opthalmol Vis Sci 54:3426. https://doi.org/10.1167/iovs.12-11509
Kashef N, Hamblin MR (2017) Can microbial cells develop resistance to oxidative stress in antimicrobial photodynamic inactivation? Drug Resist Updat 31:31–42. https://doi.org/10.1016/j.drup.2017.07.003
Acknowledgements
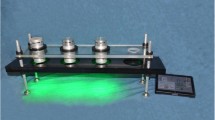
The authors are grateful to the following members of the Ophthalmic Biophysics Center team: Cornelis Rowaan, BS; Alex Gonzalez, BA; Andres Bernal, MS; and Juan Silgado, MS, for their contribution in the development and fabrication of the irradiation sources. Nicholas Nolan, MS, and Mercury Sawatari, MS, for their assistance in performing the in vitro experiments and data analysis.
Funding
This research was supported by the Edward D. and Janet K. Robson Foundation (Tulsa, OK, USA), the Florida Lions Eye Bank and the Beauty of Sight Foundation (Miami, FL, USA), Drs. K. R. Olsen and M. E. Hildebrandt, Drs. Raksha Urs and Aaron Furtado, NIH Center Core Grant P30EY14801, Research to Prevent Blindness Unrestricted Grant (GR004596-1), and the Henri and Flore Lesieur Foundation (Chicago, IL, USA) (J.-M. Parel).
Author information
Authors and Affiliations
Contributions
AA—study design, experimentation, data analysis, manuscript writing/editing.
HD—study design, experimentation, data analysis, manuscript writing/editing.
DM—study design, data analysis, manuscript editing.
MCA—study design, experimentation, data analysis, manuscript editing.
KA—study design, data analysis, manuscript editing.
NR—experimentation, manuscript editing.
GA—manuscript editing, funding acquisition.
JMP—study design, manuscript editing, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
AA, HD, MCA, DM, GA and JMP are named in a patent application on the PDAT instrument submitted by the University of Miami.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arboleda, A., Durkee, H., Miller, D. et al. Variations in irradiation energy and rose bengal concentration for photodynamic antimicrobial therapy of fungal keratitis isolates. Lasers Med Sci 39, 72 (2024). https://doi.org/10.1007/s10103-024-04014-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-04014-1