Abstract
Purposes
The primary objective of this retrospective study was to assess whether the CT dose delivered to oncologic patients was different in a subspecialty radiology department, compared to a general radiology department. The secondary explorative objective was to assess whether the objective image quality of CT examinations was different in the two settings.
Materials and methods
Chest and abdomen CT scans performed for oncologic indications were selected from a general radiology department and a subspecialty radiology department. By using a radiation dose management platform, we extracted and compared CT dose index (CTDIvol) and dose length product (DLP) both for each phase and for the entire CT exams. For objective image quality evaluation, we calculated the signal-to-noise ratio (SNR) and the contrast-to-noise ratio (CNR) at the level of the liver and of the aorta. A P-value < 0.05 was considered significant.
Results
A total of 7098 CT examinations were included. CTDIvol was evaluated in 12,804 phases; DLP in 10,713 phases and in 6714 examinations. The CTDIvol and DLP overall were significantly lower in the subspecialty radiology department compared to the general radiology department CTDI median (IQR) 5.19 (3.91–7.00) and 5.51 (4.17–7.72), DLP median and IQR of 490.0 (342.4–710.6) and 503.4 (359.9–728.8), p < 0.001 and p = 0.01, respectively. The objective image quality showed no significant difference in the general and subspecialty radiology departments, with median and IQR of 4.03 (2.82–5.51) and 3.84 (3.09–4.94) for SNRLiv (p = 0.58); 4.81 (2.70–7.62) and 4.34 (3.05–6.25) for SNRAo (p = 0.30); 0.83 (0.20–1.89) and 1.00 (0.35–1.57) for CNRLiv (p = 0.99); 2.23 (0.09–3.83) and 1.01 (0.15–2.84) for CNRAo (p = 0.24) with SNRLiv (p = 0.58), SNRAo (p = 0.30), CNRLiv (p = 0.99) and CNRAo (p = 0.24).
Conclusion
In a subspecialty radiology department, CT protocols are optimized compared to a general radiology department leading to lower doses to oncologic patients without significant objective image quality degradation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several radiology departments are changing their organization system from general to subspecialty radiology, because of the recognized importance of dedicated expertise in imaging interpretation and in multidisciplinary discussions [1,2,3]. It has been demonstrated that the second opinion and radiological reports provided by subspecialized radiologists are more effective, clear and appropriate than those provided by general radiologists [4, 5]. Furthermore, subspecialized radiologists’ interpretations lead to a better integration of the imaging reports into the clinical management of the patients, which help the transition from volume-based to value-based imaging care [6].
In clinical practice, radiologists must select the optimal CT imaging protocol to provide the required information with the lowest radiation dose. The imaging protocol selection may vary according to several factors such as the degree of detail of clinical indications, clinical information (e.g., age, weight, availability of previous imaging exams), mode of access, patient preferences, radiologist preference, radiology experience and other factors. In fact, marked variations can be seen in imaging protocols from one institution to another, within the same institution and between different radiologists, especially when the protocol is left to the choice of the radiologist alone [4].
In oncologic imaging, patients undergo multiple computed tomography (CT) examinations from staging to response assessment, follow-up and prognostication [7, 8], and are therefore prone to considerable radiation exposure, the cumulative dose exposure being possibly correlated with the risk of future cancers, especially in children and young adults [9, 10]. For this reason, previous and existing initiatives by scientific societies, such as the American College of Radiologists [11, 12] and the European Society of Radiology, support the adoption of dose management systems to ensure the justification and optimization of radiological procedures and store information on patient exposure for analysis and quality assurance [13].
We hypothesized that radiologists dedicated to oncologic imaging, aware of the imaging characteristics of tumors, are able to select the most appropriate CT imaging protocol compared to general radiologists, taking into account the need to keep the radiation dose as low as reasonably achievable [14].
In 2019, four radiology departments in the same geographical area were merged into one Imaging Institute and the radiologists were divided into subspecialty sections, according to their training, experience and preference. The reason for a specific oncologic imaging group relied on the presence of a dedicated oncologic institute in the same hospital, and in recognition of some particular characteristics in the evaluation of oncologic patients, such as the evaluation of response according to specific criteria (including response evaluation imaging criteria for solid tumors (RECIST), i-(immune)-RECIST, etc.), as well as to the increasing number of specific responses/progression patterns relative to target therapies or complications related to immunotherapies. This organizational change gave us the unique opportunity to compare the CT doses delivered to oncologic patients in the two organizational settings.
Therefore, the primary objective of this study was to assess whether the CT dose delivered to oncologic patients by chest and abdomen CT is different in a subspecialty radiology department, compared to a general radiology department. The secondary explorative objective was to assess whether the objective image quality of CT examinations was different in the two organizational settings.
Methods
This retrospective study, relying on merged anonymized data, was considered a quality care control study by our Ethics Committee and did not fall under the Swiss law of human research. As such, the need for specific approval and informed consent was waived.
CT examination selection
A business intelligence and visualization tool (Microsoft Power BI Desktop) extracted chest and abdomen CT scans performed for oncologic indications over a 12-month period when the organization was a general radiology department (01.01.2018–31.12.2018), and over a 12-month period when the organization was a subspecialty radiology department (01.01.2022–31.12.2022). The CT scans were randomly performed on 6 CT scanners available at our institution that were not changed during the two study periods (Somatom Definition Flash, Siemens Healthineers, Erlangen, Germany; 4 Somatom Definition Edge, Siemens Healthineers, Erlangen, Germany; 1 Brilliance ICT, Philips Healthcare, Eindhoven, Netherlands).
Exclusion criteria were: CT scans performed to study vascular pathologies (such as aortic aneurysms and pulmonary embolism); examinations present in the local picture archiving and communication system but performed at other institutions; and examinations including metallic prostheses. Further exclusion criterion for the whole exam DLP was the presence of a cerebral acquisition in the same exam.
Dose report data extraction
By using a commercially available dose management platform (Radimetrics, Bayer HealthCare, Leverkusen, Germany), we extracted the radiation output for each CT phase acquisition (pre-contrast, arterial, venous and delayed phases), recorded as CT dose index (CTDIvol, measured in mGy), and as dose length product (DLP, measured in mGy x cm), and for the entire single- or multiphase exam, recorded as exam DLP. Since CTDIvol is a measure of one slice, whereas DLP is a measure of a series including lots of slices, the number of records for each CT examination will be higher for CTDIvol than for DLP. CTDIvol and DLP from CT localizers and from series of few images, such as bolus triggering, were furtherly excluded.
Objective image quality evaluation
Group of CT scans (n = 100) was randomly selected from the general radiology ones (n = 50) and from the subspecialty radiology ones (n = 50). The CT datasets were selected by choosing the first 4 CT exams for each month of the period selected, and the first 5 for the months of March and July (randomly chosen because of the 31 days in these months). The images were anonymized, divided into two groups and used for the objective image quality assessment. Three circular regions of interest (ROIs) measuring 15 mm2 were drawn by a 3rd year resident in radiology [LB], supervised by a radiologist with 19 years of experience in oncologic imaging [SR] on a single CT slice at the level of the first lumbar vertebra within the following structures: the abdominal aorta, without touching the lumen walls, to cover at least two-thirds of its lumen; the right lobe of the liver, covering a homogeneous area; and the paraspinal right muscles (Fig. 1). Mean and standard deviation (image noise) of density, measured by Hounsfield units (HU), were recorded and then used to calculate the signal-to-noise ratio (SNR) and the contrast-to-noise ratio (CNR) at the level of the liver and of the aorta, according to the following formulas [15]:
-
(1)
SNRliv = HUliv/SDliv, where HUliv is the mean attenuation value and SDliv is the standard deviation in the liver ROI.
-
(2)
SNRao = HUao/SDao, where HUao is the mean attenuation value and SDao is the standard deviation in the aorta ROI.
-
(3)
CNRliv = (HUliv-HUm)/√(SD2liv + SD2m), where HUm is the mean attenuation value and SDm is the standard deviation in the muscle ROI
-
(4)
CNRao = (HUao-HUm)/√(SD2ao + SD2m)
Statistical analysis
Kolmogorov–Smirnov test, Shapiro test and QQplot were used to test the normality of CTDIvol, DLP, SNR and CNR distributions. For descriptors not normally distributed, the nonparametric Wilcoxon–Mann–Whitney (WMW) test was used. Data were summarized through median and interquartile range (IQR). Quantile regression was used to assess whether radiation dose in each phase and in the entire exam were associated with general radiology and subspecialty radiology.
For all analyses, a two-tailed p-value < 0.05 was considered statistically significant. The statistical analyses were performed with R software, version 4.2.3.
Results
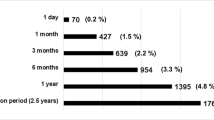
According to inclusion and exclusion criteria, 7098 CT exams were included in this study (Table 1): 3073 from the general radiology department and 4025 from the subspecialty radiology department.
The analysis of CTDIvol was performed on a cohort of 12,804 phases of acquisition (n = 5090 acquired in the general radiology department; n = 7714 in the subspecialty radiology department); the analysis of DLP was performed on a cohort of 10,713 phases of acquisition (n = 4176 acquired in the general radiology department; n = 6537 in the subspecialty radiology department). The DLP of each entire exam was evaluated in 6714 CT exams (n = 3003 acquired in the general radiology department; n = 3711 in the subspecialty radiology department).
As shown in Fig. 2, the analysis dedicated to the overall DLP showed values significantly (p < 0.001) lower in CT scans performed in the subspecialty radiology department as compared to the general radiology department, with median and IQR of 265.0 (160.2–393.1) and 304.2 (197.2–434.8), respectively.
The overall CTDIvol was significantly (p-value < 0.001) lower in CT scans performed in the subspecialty radiology department as compared to the general radiology department [median (IQR) 5.19 (3.91–7.00) and 5.51 (4.17–7.72), respectively (Fig. 3)]. A further analysis dedicated to the single acquisition phases confirmed significantly lower values of CTDIvol in the pre-contrast, arterial and portal venous phases in CT scans performed in the subspecialty radiology department, as compared to the general radiology department (Fig. 4).
As shown in Table 2, the multivariate quantile regression performed on 12,804 CTDIvol records, adjusted by phase acquisition, confirmed the results of the univariate analysis, showing significantly lower values of CTDIvol delivered by CT scans in the subspecialty radiology department compared to the general radiology department (p-value < 0.001). The same analysis, performed on all the scans according to the acquisition phase, showed a significantly higher CTDIvol for pre-contrast acquisitions compared to portal venous phase acquisitions (p < 0.001).
A further analysis dedicated to the single acquisition phases confirmed significantly lower values of DLP in the pre-contrast, arterial and portal venous phases in the subspecialty radiology department, as compared to the general radiology department (Fig. 5).
The multivariate quantile regression performed on 10,713 DLP records, adjusted by the phase acquisition, confirmed the significantly lower values of DLP delivered by CT scans in the subspecialty radiology department compared to the general radiology department (p-value < 0.001 Table 3).
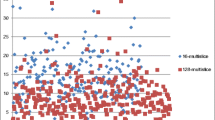
The exploratory analysis dedicated to the objective image quality showed no significant difference in SNRLiv (p-value = 0.58) and SNRAo (p-value = 0.30) of CT scans acquired in the general and subspecialty radiology departments, with median and IQR of 4.03 (2.82–5.51) and 3.84 (3.09–4.94) for SNRLiv, and of 4.81 (2.70–7.62) and 4.34 (3.05–6.25) for SNRAo, respectively (Fig. 6). Similarly, there was no significant difference in CNRLiv (p-value = 0.99) and CNRAo (p-value = 0.24) of CT scans acquired in the general and subspecialty radiology departments, with median and IQR of 0.83 (0.20–1.89) and 1.00 (0.35–1.57) for CNRLiv and of 2.23 (0.09–3.83) and 1.01 (0.15–2.84) for CNRAo, respectively (Fig. 6).
Discussion
In our study, which included 7098 chest and abdomen CT examinations, we demonstrated that after the introduction of a subspecialty based radiology department, the CT dose for patients with oncologic indications was significantly lower compared to a general radiology department, without impairment of objective image quality.
Current CT scanners produce radiation dose sheets as a separate series in each examination. Although format and content vary between manufacturers and scanner models, all include at least the CTDIvol and DLP. CTDIvol indicates the average radiation output per slice, depends on the type of scanner and acquisition parameters and is independent of patient and scan length [16, 17]. DLP is the product of the CTDIvol and scan length, and thus reflects the total amount of radiation to which the patient is exposed [16]. CTDIvol and DLP may be helpful in assisting radiologists to comply with regulatory requirements, as well as to monitor the CT doses over time [16,17,18,19,20].
Some of the available current strategies to optimize radiation exposure include the use of size-dependent protocols, the use of automated exposure control, a reduction of the number of phases and a reduction of duplicated coverage [21,22,23]. In this study, the former two were kept constant in the two cohorts, because the CT machines and technologies were not replaced during the study periods, nor did they undergo significant software updates, whereas the CT protocols in the subspecialized radiology department were adapted taking into account the latter two.
As mentioned, automated exposure control was present in the general radiology as well as in the subspecialty department, and is demonstrated by the higher CTDIvol of the native phase (usually focused on the upper abdomen) compared to the portal venous phase (including the chest and the abdomen), because, as known in the literature, the latter includes anatomical structures (e.g., the lungs) that need a lower radiation dose for optimal visualization [24, 25] Since the effect on radiation dose of multiphase CT examinations can be similar to multiple examinations, special attention should be paid to optimizing CT protocols in oncologic patients, e.g., by eliminating one or more phases [21, 22]. In a tertiary care medical center, Guite et al. demonstrated that over a 4-month period one-third of all abdominal phases resulted in an excess of effective radiation in many multiphase abdominal CT examinations [26, 27].
Previous studies demonstrated that CT dose reduction strategies also include the imaging skills of the radiologist [27,28,29,30]. Indeed, low expertise may lead to the choice of an unnecessary multiphase protocol, due to the fear of missing something. Furthermore, in a heterogeneous group of radiologists there can be a wide variability in protocol selection according to personal preferences and experience. In this regard, the inclusion of the DLP in radiological reports is a helpful way of paying constant attention to the radiation dose delivered by a CT scan examination.
In our study, the lower radiation dose of the subspecialized radiologists is likely because the subspecialized radiologists agreed on choosing protocols according to the clinical indication, the setting (staging, response to therapy assessment, follow-up) and the tumoral characteristics [16], in order to keep the dose as low as possible [14], possibly choosing different examinations if the indication was not appropriate [31]. For instance, at the first staging CT exam, the subspecialized radiologists agreed to acquire a protocol including three phases on the liver (one pre-contrast, one arterial and one portal venous phase), with the portal venous phase extending to the thorax and pelvis [32]. At the subsequent CT scans, they agreed to acquire just the portal venous phase, unless the tumor under evaluation was hypervascular (e.g., neuroendocrine tumors, renal clear cell carcinomas, breast cancers, hepatocellular cancers, melanomas) or lesions visible only in the delayed phase (e.g., urothelial tumors). This protocol strategy helped with an overall reduction of radiation exposure to the patients, as reflected by the lower DLP per exam in the subspecialty radiology, reflecting the overall exposure of the CT exam. However, this dose reduction was not strictly related to a lower number of phases acquired, as shown by 4176 acquisitions among the 3073 examinations performed by the general radiology staff, and 6537 acquisitions among the 4025 examinations performed by the subspecialty radiology staff. Indeed, since the collection of data was retrospective here, no single a priori action, such as the sole reduction of the number of acquisitions, was taken in order to see its effect on radiation dose. The dose reduction was therefore likely an integral result of the strategies altogether, rather than one alone.
Furthermore, by frequently acquiring only one phase (the portal venous phase), duplicated coverage was avoided. Indeed, scan length may not be given due attention in a busy clinical setting, although its effect on patient dose can be significant [19, 33]. Accordingly, Campbell et al. found that nearly 100% of chest CT examinations performed over a 2-week period at a large medical institution included additional images over the lung apices and below the lungs, which led to excessive radiation exposure that may even be double what is really necessary [34].
Surprisingly, aside from a lower number of delayed phases acquired, we did not find any significant difference in CT dose of the delayed phase. This result may be explained by the abovementioned adherence of the CT protocols to the clinical indication. Indeed, the delayed phase was not acquired by default in each exam, but only according to specific indications, such as in the presence of urothelial tumors, where relatively high doses are needed to detect small urothelial lesions, requiring a high spatial resolution and adequate signal- and contrast-to-noise ratios, and coverage may be limited from top of the kidneys to just below the bladder (mid pubic symphysis) [32].
Radiation staff education is another very efficient way to reinforce good practice in radiological institutes and to reduce the radiation dose to patients [35]. In a study aiming to evaluate the role of staff training events specifically designed for radiologists and technologists to achieve optimization of CT protocols, the authors demonstrated that staff training led to a significant reduction of the radiation dose associated with CT procedures (− 39.2% in unenhanced chest CT examinations and − 32.1% in contrast-enhanced whole-body CT examinations, respectively) [36]. In this study we could not perform a similar analysis, because the staff training on radiation dose was performed by radiologists and technicians regularly, according to local rules that recommend participating in one refresher teaching course, divided into four progressive modules, every 4 years, and the last one was completed in 2018–2022. Therefore, in the two periods under evaluation (2018 and 2022), all the people involved received the same teaching modules and the same training materials.
The objective of a CT scan is to obtain diagnostic images which can help to answer a clinical question in the most dose-efficient manner. Image noise is approximately inversely proportional to the square root of the radiation dose, meaning that the radiation dose must change in inverse proportion to the slice thickness to maintain constant image noise for varying reconstructed slice thicknesses [16]. With this in mind, in a subgroup of examinations we assessed whether the lower radiation dose demonstrated in the subspecialty radiology was associated with a lower image quality. This analysis did not show any significant difference in objective image noise, thus confirming that the CT protocols were correctly chosen to reduce the dose, without impairing the image quality.
This study has some limitations. One is that we did not evaluate the patients’ exposure through the effective dose, which is currently used to quantify the overall risk of fatal and non-fatal cancers, induced by ionizing radiation [14]. However, the ICRP 147 clearly states that effective dose is not the most appropriate quantity for making comparisons between doses for the same technique, where modality-specific dose quantities displayed on equipment (e.g., CTDIvol and DLP) should be used to simplify the process and to avoid unnecessary approximations [37]. For this reason, we did compare CTDIvol and DLP. Another limitation is that we cannot exclude the possibility that other factors, not evaluated here, may have influenced the difference in radiation dose. In this regard, the main other factor that could lead to such a difference would have been a replacement or an in-depth software update of one or more CT machines. However, the CT machines were not replaced in the period selected, and we can therefore exclude this as a confounding factor. Another potential confounding factor not evaluated in this series is the distribution of examinations over the 6 CT machines that might obscure a non-uniformity of the distribution. However, the patients are sent to one site or another of our multisite hospital according to their preference, mainly due to the proximity to their home, and this did not change either in the general radiology department or in the subspecialty department; the distribution therefore corresponded to a real-life scenario. Furthermore, although we evaluated a high number of CT scans (n = 7098) from the same subspecialty (oncologic imaging), we cannot confidently extend our conclusions to other subspecialties, but we may hopefully encourage similar evaluations in other subspecialties. Last but not least, we did not evaluate the effects of the reduction of radiation dose [38] and we did not consider the effects of the choice of a different imaging technique, such as magnetic resonance [39], because it was beyond the scope of our objectives and deserves dedicated prospective trials.
In conclusion, chest and abdomen CT protocols are optimized in a subspecialty radiology department compared to a general radiology department, leading to a lower radiation dose to oncologic patients without significant objective image quality degradation. This result further supports the benefit for patients of a subspecialty-based organization of radiology.
Abbreviations
- ACR:
-
American college of radiology
- ALARA:
-
As low as reasonably achievable
- CNR:
-
Contrast-to-noise ratio
- CTDIvol :
-
Computed tomography dose index volume
- DLP:
-
Dose length product
- HU:
-
Hounsfield unit
- ROI:
-
Region of interest
- SNR:
-
Signal-to-noise ratio
References
Aletti GD, Garbi A, Messori P et al (2017) Multidisciplinary approach in the management of advanced ovarian cancer patients: a personalized approach. Results from a specialized ovarian cancer unit. Gynecol Oncol 144:468–473
Petrella F, Radice D, Guarize J et al (2021) The impact of multidisciplinary team meetings on patient management in oncologic thoracic surgery: a single-center experience. Cancers (Basel) 13:228
Baker SR (1982) The operation of a radiology consultation service in an acute care hospital. JAMA 248:2152–2154
Rizzo S, Del Grande M, Espeli V, Stathis A, Nicolino GM, Del Grande F (2021) Do oncologists prefer subspecialty radiology reports? A quality care study. Insights Imaging 12:64
Chalian M, Del Grande F, Thakkar RS, Jalali SF, Chhabra A, Carrino JA (2016) Second-opinion subspecialty consultations in musculoskeletal radiology. AJR Am J Roentgenol 206:1217–1221
https://www.acr.org/Practice-Management-Quality-Informatics/Imaging-3/Imaging-Value-Chain/Appropriateness. Accessed 9 Jun 2023
Chianca V, Albano D, Messina C et al (2021) An update in musculoskeletal tumors: from quantitative imaging to radiomics. Radiol Med 126:1095–1105
Nougaret S, McCague C, Tibermacine H, Vargas HA, Rizzo S, Sala E (2021) Radiomics and radiogenomics in ovarian cancer: a literature review. Abdom Radiol (NY) 46:2308–2322
Hauptmann M, Byrnes G, Cardis E, Bernier MO, Blettner M, Dabin J, Engels H, Istad TS, Johansen C, Kaijser M, Kjaerheim K, Journy N, Meulepas JM, Moissonnier M, Ronckers C, Thierry-Chef I, Le Cornet L, Jahnen A, Pokora R, Bosch de Basea M, Figuerola J, Maccia C, Nordenskjold A, Harbron RW, Lee C, Simon SL, Berrington de Gonzalez A, Schüz J, Kesminiene A (2023) Brain cancer after radiation exposure from CT examinations of children and young adults: results from the EPI-CT cohort study. Lancet Oncol 24(1):45–53. https://doi.org/10.1016/S1470-2045(22)00655-6
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW, Parker L, Berrington de González A (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380(9840):499–505. https://doi.org/10.1016/S0140-6736(12)60815-0
Amis ES Jr, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, Mettler FA, Morin RL, Pentecost MJ, Smith GG, Strauss KJ, Zeman RK, American College of Radiology (2007) American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol 4(5):272–284
Rawat U, Cohen SL, Levsky JM, Haramati LB (2015) ACR white paper-based comprehensive dose reduction initiative is associated with a reversal of the upward trend in radiation dose for chest CT. J Am Coll Radiol 12(12):1251–6
Loose RW, Vano E, Mildenberger P, Tsapaki V, Caramella D, Sjöberg J, Paulo G, Torresin A, Schindera S, Frija G, Damilakis J, European Society of Radiology (ESR) (2021) Radiation dose management systems-requirements and recommendations for users from the ESR EuroSafe imaging initiative. Eur Radiol 31(4):2106–2114
ICRP (2007) The 2007 Recommendations of the International commission on radiological protection. ICRP publication 103. Ann ICRP 37:1–332
Arapakis I, Efstathopoulos E, Tsitsia V et al (2014) Using “iDose4” iterative reconstruction algorithm in adults’ chest–abdomen–pelvis CT examinations: effect on image quality in relation to patient radiation exposure. Br J Radiol 87:20130613
Maldjian PD, Goldman AR (2013) Reducing radiation dose in body CT: a primer on dose metrics and key CT technical parameters. AJR Am J Roentgenol 200:741–747
Tamm EP, Rong XJ, Cody DD, Ernst RD, Fitzgerald NE, Kundra V (2011) Quality initiatives: CT radiation dose reduction: how to implement change without sacrificing diagnostic quality. Radiographics 31:1823–1832
McCollough C, Branham T, Herlihy V et al (2011) Diagnostic reference levels from the ACR CT accreditation program. J Am Coll Radiol 8:795–803
Zhao A, Fopma S, Agrawal R (2022) Demystifying the CT radiation dose sheet. Radiographics 42:1239–1250
Kalra MK, Rizzo S, Maher MM et al (2005) Chest CT performed with z-axis modulation: scanning protocol and radiation dose. Radiology 237:303–308
Sodickson A (2012) Strategies for reducing radiation exposure in multi-detector row CT. Radiol Clin North Am 50:1–14
Rizzo SM, Kalra MK, Schmidt B et al (2005) CT images of abdomen and pelvis: effect of nonlinear three-dimensional optimized reconstruction algorithm on image quality and lesion characteristics. Radiology 237:309–315
Dalal T, Kalra MK, Rizzo SM et al (2005) Metallic prosthesis: technique to avoid increase in CT radiation dose with automatic tube current modulation in a phantom and patients. Radiology 236:671–675
Greffier J, Larbi A, Macri F, Beregi JP, Pereira F (2017) Effect of patients size, anatomical location and modulation strength on dose delivered and image-quality on CT examination. Radiat Prot Dosimetry 177(4):373–381
MacDougall RD, Kleinman PL, Callahan MJ (2016) Size-based protocol optimization using automatic tube current modulation and automatic kV selection in computed tomography. J Appl Clin Med Phys 17(1):328–341
Guite KM, Hinshaw JL, Ranallo FN, Lindstrom MJ, Lee FT (2011) Ionizing radiation in abdominal CT: unindicated multiphase scans are an important source of medically unnecessary exposure. J Am Coll Radiol 8:756–761
Costello JE, Cecava ND, Tucker JE, Bau JL (2013) CT radiation dose: current controversies and dose reduction strategies. AJR Am J Roentgenol 201:1283–1290
Rizzo S, Kalra M, Schmidt B et al (2006) Comparison of angular and combined automatic tube current modulation techniques with constant tube current CT of the abdomen and pelvis. AJR 186:673–679
Amis ES Jr, Butler PF, American College of Radiology (2010) ACR white paper on radiation dose in medicine: three years later. J Am Coll Radiol 7:865–870
Kalra MK, Maher MM, Toth TL et al (2004) Strategies for CT radiation dose optimization. Radiology 230:619–628
Rietjens M, Villa G, Toesca A et al (2014) Appropriate use of magnetic resonance imaging and ultrasound to detect early silicone gel breast implant rupture in postmastectomy reconstruction. Plast Reconstr Surg 134:13e–20e
Goldman AR, Maldjian PD (2013) Reducing radiation dose in body CT: a practical approach to optimizing CT protocols. AJR Am J Roentgenol 200:748–754
Kubo T (2019) Vendor free basics of radiation dose reduction techniques for CT. Eur J Radiol 110:14–21
Campbell J, Kalra MK, Rizzo S, Maher MM, Shepard J (2005) Scanning beyond anatomic limits of the thorax in chest CT: findings, radiation dose, and automatic current modulation. AJR 185:1525–1530
Hojreh A, Weber M, Homolka P (2015) Effect of staff training on radiation dose in pediatric CT. Eur J Radiol 84(8):1574–1578
Paolicchi F, Faggioni L, Bastiani L, Molinaro S, Caramella D, Bartolozzi C (2013) Real practice radiation dose and dosimetric impact of radiological staff training in body CT examinations. Insights Imaging 4(2):239–244
Harrison JD, Balonov M, Bochud F et al (2021) ICRP Publication 147: use of dose quantities in radiological protection. Ann ICRP 50:9–82
Sullivan CJ, Murphy KP, McLaughlin PD, Twomey M, O’Regan KN, Power DG, Maher MM, O’Connor OJ (2015) Radiation exposure from diagnostic imaging in young patients with testicular cancer. Eur Radiol 25(4):1005–1013. https://doi.org/10.1007/s00330-014-3507-0
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K, Horwich A, Laguna MP, Nicolai N, Oldenburg J (2015) Guidelines on testicular cancer: 2015 update. Eur Urol 68(6):1054–68. https://doi.org/10.1016/j.eururo.2015.07.044
Acknowledgements
The English text was revised by Susan West.
Funding
Open access funding provided by Università della Svizzera italiana. The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SR, LB, AD, OD and FM. The first draft of the manuscript was written by SR, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The present study was considered a quality care control study by our Ethical Committee and did not fall under the Swiss law of the human research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rizzo, S., Bellesi, L., D’Ermo, A. et al. Body CT examinations in oncologic patients: the impact of subspecialty radiology on radiation exposure in the clinical practice. A quality care study. Radiol med 129, 429–438 (2024). https://doi.org/10.1007/s11547-024-01790-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01790-2