Abstract
Purpose
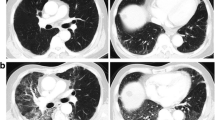
This retrospective study aimed to identify the factors associated with cavity formation after SBRT in peripheral early-stage lung cancer patients. We analyzed the occurrence of cavity changes after SBRT.
Materials and Methods
We examined 99 cases with T1-T2aN0 peripheral non-small cell lung cancer treated with SBRT from 2004 to 2021. Patients underwent respiratory function tests, including diffusing capacity for carbon monoxide (DLco), before treatment. The median observation period was 35 months (IQR 18–47.5 months). Treatment involved fixed multi-portal irradiation in 67% of cases and VMAT in 33%. The total radiation doses ranged from 42 to 55 Gy, delivered over 4 to 5 fractions.
Results
Cavity formation occurred in 14 cases (14.1%), appearing a median of 8 months after SBRT. The cavity disappeared in a median of 4 months after formation. High DLco and total radiation dose were identified as factors significantly associated with cavity formation. There have been no confirmed recurrences to date, but one patient developed a lung abscess.
Conclusion
Although cavity formation after SBRT for peripheral early-stage lung cancer is infrequent, it can occur. This study showed high DLco and total radiation dose to be factors significantly associated with cavity formation. These findings can be applied to optimizing radiation therapy (RT) and improving patient outcomes. Further research is needed to determine the optimal radiation dose for patients with near-normal DLco for whom surgery is an option. This study provides valuable insights into image changes after RT.



Similar content being viewed by others
Abbreviations
- SBRT:
-
Stereotactic body radiation therapy
- DLco:
-
Diffusing capacity for carbon monoxide
- IQR:
-
Interquartile range
- VC:
-
Vital capacity
- FEV1.0:
-
Forced expiratory volume during the first second
- CTV:
-
Clinical target volume
- ITV:
-
Internal target volume
- PTV:
-
Planning target volume
- JCOG:
-
Japan clinical oncology group
- VMAT:
-
Volumetric modulated arc therapy
- BED:
-
Biologically effective dose
- UL:
-
Upper lobe
- LL:
-
Lower lobe
- ML:
-
Middle lobe
- PS:
-
Performance status
References
Nagata Y, Hiraoka M, Shibata T, Onishi H, Kokubo M, Karasawa K, Shioyama Y, Onimaru R, Kozuka T, Kunieda E, Saito T, Nakagawa K, Hareyama M, Takai Y, Hayakawa K, Mitsuhashi N, Ishikura S (2015) Prospective trial of stereotactic body radiation therapy for both operable and inoperable T1N0M0 non-small cell lung cancer: japan clinical oncology group study JCOG0403. Int J Radiat Oncol Biol Phys 93:989–996. https://doi.org/10.1016/j.ijrobp.2015.07.2278
Ricardi U, Filippi AR, Guarneri A, Giglioli FR, Ciammella P, Franco P, Mantovani C, Borasio P, Scagliotti GV, Ragona R (2010) Stereotactic body radiation therapy for early stage non-small cell lung cancer: results of a prospective trial. Lung Cancer 68:72–77. https://doi.org/10.1016/j.lungcan.2009.05.007
Shibamoto Y, Hashizume C, Baba F, Ayakawa S, Manabe Y, Nagai A, Miyakawa A, Murai T, Iwata H, Mori Y, Mimura M, Ishikura S (2012) Stereotactic body radiotherapy using a radiobiology-based regimen for stage I nonsmall cell lung cancer: a multicenter study. Cancer 118:2078–2084. https://doi.org/10.1002/cncr.26470
Timmerman R, McGarry R, Yiannoutsos C, Papiez L, Tudor K, DeLuca J, Ewing M, Abdulrahman R, DesRosiers C, Williams M, Fletcher J (2006) Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol 24:4833–4839. https://doi.org/10.1200/JCO.2006.07.5937
Fakiris AJ, McGarry RC, Yiannoutsos CT, Papiez L, Williams M, Henderson MA, Timmerman R (2009) Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: four-year results of a prospective phase II study. Int J Radiat Oncol Biol Phys 75:677–682. https://doi.org/10.1016/j.ijrobp.2008.11.042
Timmerman RD, Hu C, Michalski JM, Bradley JC, Galvin J, Johnstone DW, Choy H (2018) Long-term results of stereotactic body radiation therapy in medically inoperable stage I non-small cell lung cancer. JAMA Oncol 4:1287–1288. https://doi.org/10.1001/jamaoncol.2018.1258
Videtic GM, Paulus R, Singh AK, Chang JY, Parker W, Olivier KR, Timmerman RD, Komaki RR, Urbanic JJ, Stephans KL, Yom SS, Robinson CG, Belani CP, Iyengar P, Ajlouni MI, Gopaul DD, Gomez Suescun JB, McGarry RC, Choy H, Bradley JD (2019) Long-term follow-up on NRG oncology RTOG 0915 (NCCTG N0927): a randomized phase 2 study comparing 2 stereotactic body radiation therapy schedules for medically inoperable patients with stage I peripheral non-small cell lung cancer. Int J Radiat Oncol Biol Phys 103:1077–1084. https://doi.org/10.1016/j.ijrobp.2018.11.051PMC6454873
Singh AK, Gomez-Suescun JA, Stephans KL, Bogart JA, Hermann GM, Tian L, Groman A, Videtic GM (2019) One versus three fractions of stereotactic body radiation therapy for peripheral stage I to II non-small cell lung cancer: a randomized, multi-institution, phase 2 trial. Int J Radiat Oncol Biol Phys 105:752–759. https://doi.org/10.1016/j.ijrobp.2019.08.019
Lee K, Le T, Hau E, Hanna GG, Gee H, Vinod S, Dammak S, Palma D, Ong A, Yeghiaian-Alvandi R, Buck J, Lim R (2022) A systematic review into the radiologic features predicting local recurrence after stereotactic ablative body radiotherapy (SABR) in patients with non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys 113:40–59. https://doi.org/10.1016/j.ijrobp.2021.11.027
Matsumoto Y (2022) A pictorial essay on radiological changes after stereotactic body radiation therapy for lung tumors. Jpn J Radiol 4:647–663. https://doi.org/10.1007/s11604-022-01252-7
Maebayashi T, Ishibashi N, Aizawa T, Sakaguchi M, Sato T, Kawamori J, Tanaka Y (2016) Radiation pneumonitis changes over time after stereotactic body radiation therapy for lung tumors: post-treatment cavity (Sunny-side-up Egg-like) changes. Anticancer Res 36:5563–5570. https://doi.org/10.21873/anticanres.11141
Al-Umairi R, Tarique U, Moineddin R, Jimenez-Juan L, Kha LC, Cheung P, Oikonomou A (2022) CT patterns and serial CT changes in lung Cancer patients post stereotactic body radiotherapy (SBRT). Cancer Imaging 22:51. https://doi.org/10.1186/s40644-022-00491-1
Chang JY, Bezjak A, Mornex F (2015) Stereotactic ablative radiotherapy for centrally located early stage non-small-cell lung cancer: what we have learned. J Thorac Oncol 10:577–585. https://doi.org/10.1097/JTO.0000000000000453
Kimura T, Nagata Y, Eba J, Ozawa S, Ishikura S, Shibata T, Ito Y, Hiraoka M, Nishimura Y (2017) A randomized Phase III trial of comparing two dose-fractionations stereotactic body radiotherapy (SBRT) for medically inoperable stage IA non-small cell lung cancer or small lung lesions clinically diagnosed as primary lung cancer: Japan clinical oncology group study JCOG1408 (J-SBRT trial). Jpn J Clin Oncol 47:277–281. https://doi.org/10.1093/jjco/hyw198
Park HJ, Kim KJ, Park SH, Kay CS, Oh JS (2009) Early CT findings of tomotherapy-induced radiation pneumonitis after treatment of lung malignancy. AJR Am J Roentgenol 193:W209–W213. https://doi.org/10.2214/AJR.08.2298
Pagani JJ, Libshitz HI (1982) CT manifestations of radiation-induced change in chest tissue. J Comput Assist Tomogr 6:243–248
Ronden MI, Palma D, Slotman BJ, Senan S (2018) Brief report on radiological changes following stereotactic ablative radiotherapy (SABR) for early-stage lung tumors: a pictorial essay. J Thorac Oncol 13:855–862. https://doi.org/10.1016/j.jtho.2018.02.023
Dahele M, Palma D, Lagerwaard F, Slotman B, Senan S (2011) Radiological changes after stereotactic radiotherapy for stage I lung cancer. J Thorac Oncol 6:1221–1228. https://doi.org/10.1097/JTO.0b013e318219aac5
Faruqi S, Giuliani ME, Raziee H, Yap ML, Roberts H, Le LW, Brade A, Cho J, Sun A, Bezjak A, Hope AJ (2014) Interrater reliability of the categorization of late radiographic changes after lung stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys 89:1076–1083. https://doi.org/10.1016/j.ijrobp.2014.04.042
Li Q, Liu Y, Su B, Zhao H, Lin Q, Zhu Y, Zhang L, Weng D, Gong X, Sun X, Xu Y (2020) The CT appearance pattern of radiation-induced lung injury and tumor recurrence after stereotactic body radiation therapy in early stage non-small cell lung cancer. Transl Lung Cancer Res 9:713–721. https://doi.org/10.21037/tlcr-20-609
Hayashi S, Tanaka H, Hoshi H (2015) Imaging characteristics of local recurrences after stereotactic body radiation therapy for stage I non-small cell lung cancer: evaluation of mass-like fibrosis. Thorac Cancer 6:1861–1893. https://doi.org/10.1111/1759-7714.12162
Palma DA, de Koste JVS, Verbakel WF, Vincent A, Senan S (2011) Lung density changes after stereotactic radiotherapy: a quantitative analysis in 50 patients. Int J Radiat Oncol Biol Phys 81:974–978. https://doi.org/10.1016/j.ijrobp.2010.07.025
Aoki T, Nagata Y, Negoro Y, Takayama K, Mizowaki T, Kokubo M, Oya N, Mitsumori M, Hiraoka M (2004) Evaluation of lung injury after three-dimensional conformal stereotactic radiation therapy for solitary lung tumors: CT appearance. Radiology 230:101–108. https://doi.org/10.1148/radiol.2301021226
Al Feghali KA, Wu QC, Devpura S, Liu C, Ghanem AI, Wen NW, Ajlouni M, Simoff MJ, Movsas B, Chetty IJ (2020) Correlation of normal lung density changes with dose after stereotactic body radiotherapy (SBRT) for early stage lung cancer. Clin Transl Radiat Oncol 22:1–8. https://doi.org/10.1016/j.ctro.2020.02.004
Itonaga T, Sugahara S, Mikami R, Saito T, Yamada T, Kurooka M, Shiraishi S, Okubo M, Saito K (2021) Evaluation of the relationship between the range of radiation-induced lung injury on CT images after IMRT for stage I lung cancer and dosimetric parameters. Ann Med 53:267–273. https://doi.org/10.1080/07853890.2020.1869297
Stephans KL, Woody NM, Reddy CA, Varley M, Magnelli A, Zhuang T, Qi P, Videtic GMM (2018) Tumor control and toxicity for common stereotactic body radiation therapy dose-fractionation regimens in stage I non-small cell lung cancer. Int J Radiat Oncol Biol Phys 100:462–469. https://doi.org/10.1016/j.ijrobp.2017.10.037
Badellino S, Muzio JD, Schivazappa G, Guarneri A, Ragona R, Bartoncini S, Trino E, Filippi AR, Fonio P, Ricardi U (2017) No differences in radiological changes after 3D conformal vs VMAT-based stereotactic radiotherapy for early stage non-small cell lung cancer. Br J Radiol 90:20170143. https://doi.org/10.1259/bjr.20170143
Senthi S, Dahele M, van de Ven PM, Slotman BJ, Senan S (2013) Late radiologic changes after stereotactic ablative radiotherapy for early stage lung cancer: a comparison of fixed-beam versus arc delivery techniques. Radiother Oncol 109:77–81. https://doi.org/10.1016/j.radonc.2013.08.034
Stanic S, Paulus R, Timmerman RD, Michalski JM, Barriger RB, Bezjak A, Videtic GM, Bradley J (2014) No clinically significant changes in pulmonary function following stereotactic body radiation therapy for early–stage peripheral non-small cell lung cancer: an analysis of RTOG 0236. Int J Radiat Oncol Biol Phys 88:1092–1099. https://doi.org/10.1016/j.ijrobp.2013.12.050
Navarro-Martin A, Aso S, Cacicedo J, Arnaiz M, Navarro V, Rosales S, de Blas R, Ramos R, Guedea F (2016) Phase II trial of SBRT for stage I NSCLC: survival, local control, and lung function at 36 months. J Thorac Oncol 11:1101–1111. https://doi.org/10.1016/j.jtho.2016.03.021
Berg J, Ramberg C, Haugstvedt JOS, Bengtson MB, Gabrielsen AM, Brustugun OT, Halvorsen AR, Helland A (2021) Lung function after stereotactic body radiation therapy for early-stage non-small cell lung cancer, changes and predictive markers. Front Oncol 11:674731. https://doi.org/10.3389/fonc.2021.674731.eCollection2021
Käsmann L, Dietrich A, Staab-Weijnitz CA, Manapov F, Behr J, Rimner A, Jeremic B, Senan S, De Ruysscher D, Lauber K, Belka C (2020) Radiation-induced lung toxicity–cellular and molecular mechanisms of pathogenesis, management, and literature review. Radiat Oncol 15:214. https://doi.org/10.1186/s13014-020-01654-9
Stenton CG, Boland J (1967) Experimental radiation pneumonitis: radiographic and pathologic correlation. Cancer 20:2170–2183
Takahashi M, Balazs G, Pipman Y, Moskowitz GW, Palestro CJ, Eacobacci T, Khan A, Herman PG (1995) Radiation-induced lung injury using a pig model. Evaluation by high-resolution computed tomography. Invest Radiol 30:79–86. https://doi.org/10.1097/00004424-199502000-00003
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Toshiaya Maebayashi, Akahiko Sato, Takuya Aizawa, Masakuni Sakaguchi and Naoya Ishibashi. The first draft of the manuscript was written by Toshiya Maebayashi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of Nihon University School of Medicine, and informed consent was obtained from all participating patients (Trial registration number: Nihon University Itabashi Hospital Clinical Research Center RK-190611–3).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Written informed consent was obtained from each patient for all diagnostic tests and treatments, as well as for publication of this report and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of the journal.
Patient consent for publication
Written informed consent was obtained from each patient for all diagnostic tests and treatments, as well as for publication of this report and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maebayashi, T., Ishibashi, N., Sakaguchi, M. et al. Factors associated with cavity formation after stereotactic body radiation therapy for peripheral early-stage lung cancer. Radiol med 129, 507–514 (2024). https://doi.org/10.1007/s11547-024-01766-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01766-2