Abstract
Purpose
Hemorrhagic stroke (HS) is a devastating complication during extracorporeal membrane oxygenation (ECMO) but markers of risk stratification during COVID-19 are unknown. Lactate dehydrogenase (LDH) is a readily available biomarker of cell injury and permeability. We sought to determine whether an elevated LDH before ECMO placement is related to the occurrence of HS during ECMO for COVID-19.
Methods
Adult patients with COVID-19 requiring ECMO between March 2020 and February 2022 were included. LDH values prior to ECMO placement were captured. Patients were categorized into high (> 750 U/L) or low (≤ 750 U/L) LDH groups. Multivariable regression modeling was used to determine the association between LDH and HS during ECMO.
Results
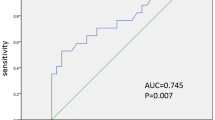
There were 520 patients that underwent ECMO placement in 17 centers and 384 had an available LDH. Of whom, 122 (32%) had a high LDH. The overall incidence of HS was 10.9%, and patients with high LDH had a higher incidence of HS than those with low LDH level (17% vs 8%, p = 0.007). At 100 days, the probability of a HS was 40% in the high LDH group and 23% in those with a low LDH, p = 0.002. After adjustment for clinical covariates, high LDH remained associated with subsequent HS (aHR: 2.64, 95% CI 1.39–4.92). Findings were similar when restricting to patients supported by venovenous ECMO only.
Conclusion
Elevated LDH prior to ECMO cannulation is associated with a higher incidence of HS during device support. LDH can risk stratify cases for impending cerebral bleeding during ECMO.




Similar content being viewed by others
Abbreviations
- ECMO:
-
Extracorporeal membrane oxygenation
- ARDS:
-
Acute respiratory distress syndrome
- HS:
-
Hemorrhagic stroke
- LDH:
-
Lactate dehydrogenase
References
Saeed O, Tatooles AJ, Farooq M et al (2022) Characteristics and outcomes of patients with COVID-19 supported by extracorporeal membrane oxygenation: a retrospective multicenter study. J Thorac Cardiovasc Surg 163:2107-2116.e6. https://doi.org/10.1016/j.jtcvs.2021.04.089
Badulak J, Antonini MV, Stead CM et al (2021) Extracorporeal membrane oxygenation for COVID-19: updated 2021 guidelines from the extracorporeal life support organization. ASAIO J 67:485–495. https://doi.org/10.1097/MAT.0000000000001422
Shaefi S, Brenner SK, Gupta S et al (2021) Extracorporeal membrane oxygenation in patients with severe respiratory failure from COVID-19. Intensive Care Med 47:208–221. https://doi.org/10.1007/s00134-020-06331-9
Ling RR, Ramanathan K, Sim JJL et al (2022) Evolving outcomes of extracorporeal membrane oxygenation during the first 2 years of the COVID-19 pandemic: a systematic review and meta-analysis. Crit Care 26:147. https://doi.org/10.1186/s13054-022-04011-2
Ramanathan K, Shekar K, Ling RR et al (2021) Extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Crit Care 25:211. https://doi.org/10.1186/s13054-021-03634-1
Schmidt M, Langouet E, Hajage D et al (2021) Evolving outcomes of extracorporeal membrane oxygenation support for severe COVID-19 ARDS in sorbonne hospitals. Paris Crit Care 25:355. https://doi.org/10.1186/s13054-021-03780-6
Lebreton G, Schmidt M, Ponnaiah M et al (2021) Extracorporeal membrane oxygenation network organisation and clinical outcomes during the COVID-19 pandemic in Greater Paris, France: a multicentre cohort study. Lancet Respir Med 9:851–862. https://doi.org/10.1016/S2213-2600(21)00096-5
Bertini P, Guarracino F, Falcone M et al (2022) ECMO in COVID-19 patients: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 36:2700–2706. https://doi.org/10.1053/j.jvca.2021.11.006
Chung M, Cabezas FR, Nunez JI et al (2020) Hemocompatibility-related adverse events and survival on venoarterial extracorporeal life support: an ELSO registry analysis. JACC Heart Fail. https://doi.org/10.1016/j.jchf.2020.09.004
Nunez JI, Gosling AF, O’Gara B et al (2022) Bleeding and thrombotic events in adults supported with venovenous extracorporeal membrane oxygenation: an ELSO registry analysis. Intensive Care Med. https://doi.org/10.1007/s00134-021-06593-x
Schmidt M, Hajage D, Lebreton G et al (2020) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med 8:1121–1131. https://doi.org/10.1016/S2213-2600(20)30328-3
Mansour A, Flecher E, Schmidt M et al (2022) Bleeding and thrombotic events in patients with severe COVID-19 supported with extracorporeal membrane oxygenation: a nationwide cohort study. Intensive Care Med 48:1039–1052. https://doi.org/10.1007/s00134-022-06794-y
Kannapadi N, v, Jami M, Premraj L, et al (2022) Neurological complications in COVID-19 patients With ECMO support: a systematic review and meta-analysis. Heart Lung Circ 31:292–298. https://doi.org/10.1016/j.hlc.2021.10.007
Lang CN, Dettinger JS, Berchtold-Herz M et al (2021) Intracerebral hemorrhage in COVID-19 patients with pulmonary failure: a propensity score-matched registry study. Neurocrit Care 34:739–747. https://doi.org/10.1007/s12028-021-01202-7
Luyt C-E, Bréchot N, Demondion P et al (2016) Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med 42:897–907. https://doi.org/10.1007/s00134-016-4318-3
Ippolito A, Urban H, Ghoroghi K et al (2022) Prevalence of acute neurological complications and pathological neuroimaging findings in critically ill COVID-19 patients with and without VV-ECMO treatment. Sci Rep 12:17423. https://doi.org/10.1038/s41598-022-21475-y
Arachchillage DRJ, Passariello M, Laffan M et al (2018) Intracranial hemorrhage and early mortality in patients receiving extracorporeal membrane oxygenation for severe respiratory failure. Semin Thromb Hemost 44:276–286. https://doi.org/10.1055/s-0038-1636840
Cho S-M, Canner J, Caturegli G et al (2021) Risk factors of ischemic and hemorrhagic strokes during venovenous extracorporeal membrane oxygenation: analysis of data from the extracorporeal life support organization registry. Crit Care Med 49:91–101. https://doi.org/10.1097/CCM.0000000000004707
Seeliger B, Doebler M, Hofmaenner DA et al (2022) Intracranial hemorrhages on extracorporeal membrane oxygenation: differences between COVID-19 and other viral acute respiratory distress syndrome. Crit Care Med 50:e526–e538. https://doi.org/10.1097/CCM.0000000000005441
Ghahramani S, Tabrizi R, Lankarani KB et al (2020) Laboratory features of severe vs. Non-severe COVID-19 patients in Asian populations: a systematic review and meta-analysis. Eur J Med Res. https://doi.org/10.1186/s40001-020-00432-3
Motawea KR, Varney J, Talat NE et al (2022) Lactate dehydrogenase can be considered a predictive marker of severity and mortality of Covid-19 in diabetic and non-diabetic patients. A Case Series Am Heart J 254:246–247. https://doi.org/10.1016/J.AHJ.2022.10.040
Martha JW, Wibowo A, Pranata R (2022) Prognostic value of elevated lactate dehydrogenase in patients with COVID-19: a systematic review and meta-analysis. Postgrad Med J 98:422–427. https://doi.org/10.1136/postgradmedj-2020-139542
Silina E, v, Rumyantceva SA, Stupin VA, et al (2021) Early predictive blood markers of hemorrhagic stroke - influence of cytoflavin therapy. Can J Physiol Pharmacol 99:72–79. https://doi.org/10.1139/cjpp-2020-0277
Wang A, Tian X, Zuo Y et al (2021) High lactate dehydrogenase was associated with adverse outcomes in patients with acute ischemic stroke or transient ischemic attack. Ann Palliat Med 10:10185–10195. https://doi.org/10.21037/apm-21-2195
Jin H, Bi R, Hu J et al (2022) Elevated serum lactate dehydrogenase predicts unfavorable outcomes after rt-PA thrombolysis in ischemic stroke patients. Front Neurol 13:816216. https://doi.org/10.3389/fneur.2022.816216
Chu H, Huang C, Dong J et al (2019) Lactate dehydrogenase predicts early hematoma expansion and poor outcomes in intracerebral hemorrhage patients. Transl Stroke Res 10:620–629. https://doi.org/10.1007/s12975-019-0686-7
Wang C-Y, Zhang Y-B, Wang J-Q et al (2022) Association between serum lactate dehydrogenase level and hematoma expansion in patients with primary intracerebral hemorrhage: a propensity-matched analysis. World Neurosurg 160:e579–e590. https://doi.org/10.1016/j.wneu.2022.01.080
Jin XX, Fang MD, Hu LL et al (2022) Elevated lactate dehydrogenase predicts poor prognosis of acute ischemic stroke. PLoS One 17:e0275651. https://doi.org/10.1371/journal.pone.0275651
Saeed O, Silvestry S (2021) Extracorporeal membrane oxygenation support during the coronavirus disease 2019 pandemic: outcomes and technical considerations. JTCVS open 8:77–82. https://doi.org/10.1016/j.xjon.2021.09.022
Jin Y, Zhang Y, Liu J (2022) Ischemic stroke and intracranial hemorrhage in extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Perfusion. https://doi.org/10.1177/02676591221130886
Cavayas YA, Munshi L, del Sorbo L, Fan E (2020) The early change in PaCO2 after extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J Respir Crit Care Med 201:1525–1535. https://doi.org/10.1164/rccm.202001-0023OC
Lüsebrink E, Zimmer S, Schrage B et al (2022) Intracranial haemorrhage in adult patients on venoarterial extracorporeal membrane oxygenation. Eur Heart J Acute Cardiovasc Care 11:303–311. https://doi.org/10.1093/ehjacc/zuac018
Bermea RS, Raz Y, Sertic F et al (2021) Increased intracranial hemorrhage amid elevated inflammatory markers in those with COVID-19 supported with extracorporeal membrane oxygenation. Shock 56:206–214. https://doi.org/10.1097/SHK.0000000000001730
Cho S-M, Premraj L, Fanning J et al (2021) Ischemic and hemorrhagic stroke among critically Ill patients with coronavirus disease 2019: an international multicenter coronavirus disease 2019 critical care consortium study. Crit Care Med 49:e1223–e1233. https://doi.org/10.1097/CCM.0000000000005209
Henry BM, Aggarwal G, Wong J et al (2020) Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: a pooled analysis. Am J Emerg Med 38:1722–1726. https://doi.org/10.1016/j.ajem.2020.05.073
Zhang D, Shi L (2021) Serum lactate dehydrogenase level is associated with in-hospital mortality in critically Ill patients with acute kidney injury. Int Urol Nephrol 53:2341–2348. https://doi.org/10.1007/s11255-021-02792-z
Erez A, Shental O, Tchebiner JZ et al (2014) Diagnostic and prognostic value of very high serum lactate dehydrogenase in admitted medical patients. Isr Med Assoc J 16:439–443
Lampl Y, Paniri Y, Eshel Y, Sarova-Pinhas I (1990) Cerebrospinal fluid lactate dehydrogenase levels in early stroke and transient ischemic attacks. Stroke 21:854–857. https://doi.org/10.1161/01.STR.21.6.854
Zan X, Deng H, Zhang Y et al (2022) Lactate dehydrogenase predicting mortality in patients with aneurysmal subarachnoid hemorrhage. Ann Clin Transl Neurol 9:1565–1573. https://doi.org/10.1002/acn3.51650
McAlpine LS, Zubair AS, Maran I et al (2021) Ischemic stroke, inflammation, and endotheliopathy in COVID-19 patients. Stroke 52:e233–e238. https://doi.org/10.1161/STROKEAHA.120.031971
Merad M, Subramanian A, Wang TT (2021) An aberrant inflammatory response in severe COVID-19. Cell Host Microbe 29:1043–1047. https://doi.org/10.1016/j.chom.2021.06.018
Fajgenbaum DC, June CH (2020) Cytokine storm. N Engl J Med 383:2255–2273. https://doi.org/10.1056/NEJMra2026131
Acknowledgements
Not applicable
Funding
The production of this manuscript was made without any source of funding.
Author information
Authors and Affiliations
Contributions
OS, UJ created the study protocol. JN and OS wrote the manuscript and created the figures. All authors reviewed the manuscript
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nunez, J.I., Uehara, M., Mohamed, A. et al. Lactate Dehydrogenase and Hemorrhagic Stroke During Extracorporeal Membrane Oxygenation for COVID-19. Lung 201, 397–406 (2023). https://doi.org/10.1007/s00408-023-00630-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-023-00630-w