Abstract
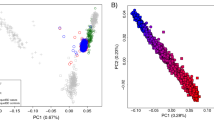
Inflammatory bowel diseases (IBDs) are chronic disorders of the gastrointestinal tract with the following two subtypes: Crohn’s disease (CD) and ulcerative colitis (UC). To date, most IBD genetic associations were derived from individuals of European (EUR) ancestries. Here we report the largest IBD study of individuals of East Asian (EAS) ancestries, including 14,393 cases and 15,456 controls. We found 80 IBD loci in EAS alone and 320 when meta-analyzed with ~370,000 EUR individuals (~30,000 cases), among which 81 are new. EAS-enriched coding variants implicate many new IBD genes, including ADAP1 and GIT2. Although IBD genetic effects are generally consistent across ancestries, genetics underlying CD appears more ancestry dependent than UC, driven by allele frequency (NOD2) and effect (TNFSF15). We extended the IBD polygenic risk score (PRS) by incorporating both ancestries, greatly improving its accuracy and highlighting the importance of diversity for the equitable deployment of PRS.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
CaVEMaN and DAP-G GTEx v8 fine-mapping cis-eQTL data were retrieved from https://gtexportal.org/home/datasets#filesetFilesDiv15. 1000 Genomes Project Phase 3 is available from https://www.internationalgenome.org/category/phase-3/. TOPMed reference panel R2 is available from https://imputation.biodatacatalyst.nhlbi.nih.gov/#!. Human Genome Diversity Project is available from https://www.internationalgenome.org/data-portal/data-collection/hgdp. Simons Genome Diversity Project is available from https://www.simonsfoundation.org/simons-genome-diversity-project/. Korean Personal Genome Diversity Project is available from http://opengenome.net/Main_Page. NBDC human database (accession ID: JGAS000114) is available from https://humandbs.biosciencedbc.jp/en/. STRING functional protein association networks are available from https://string-db.org/. NFE summary statistics are from ftp://ftp.sanger.ac.uk/pub/project/humgen/summary_statistics/human/2016-11-07/. FIN summary statistics are from FinnGen R7, https://www.finngen.fi/en/access_results. PRS weights and genome-wide summary statistics for the meta-analyzed EAS samples and across all study samples (EAS and EUR) can be downloaded from https://www.ibdgenetics.org. Individual-level genotype data for EAS samples are available upon request: SHA1, Z.L. (zhanjuliu@tongji.edu.cn); KOR1, K.S. (kysong@amc.seoul.kr); JPN1, Y. Kakuta (ykakuta@med.tohoku.ac.jp) and ICH1, IIBDGC (ibdgc-dcc@mssm.edu). Access to individual-level genotypes from samples recruited within mainland China is subject to the policies and approvals from the Human Genetic Resource Administration, Ministry of Science and Technology of the People’s Republic of China.
Code availability
Computer code relating to this study includes:
RICOPILI v2019_Jun_25.001: https://sites.google.com/a/broadinstitute.org/ricopili
EIGENSTRAT v6.1.4: PCA, https://github.com/DReichLab/EIG/tree/master/EIGENSTRAT
bcftools v1.11: http://samtools.github.io/bcftools/bcftools.html
LDSC v1.0.1: https://github.com/bulik/ldsc
S-LDXR v0.3-beta: https://huwenboshi.github.io/s-ldxr
HRC-1000G-check-bim v4.3.0: https://www.well.ox.ac.uk/~wrayner/tools/HRC-1000G-check-bim-v4.3.0.zip
VcfCooker v1.1.1: https://genome.sph.umich.edu/wiki/VcfCooker
Eagle2 v2.4.1: https://alkesgroup.broadinstitute.org/Eagle/
Minimac4 v1.0.0: https://genome.sph.umich.edu/wiki/Minimac4
apt software v2.10.2.2: https://www.thermofisher.com/us/en/home/life-science/microarray-analysis/microarray-analysis-partners-programs/affymetrix-developers-network/affymetrix-power-tools.html
SNPolisher v3.0: https://downloads.thermofisher.com/SNPolisher_3.0.zip
BEAGLE v5.1: https://faculty.washington.edu/browning/beagle/b5_1.html
PLINK2 v2.00a3.6: https://www.cog-genomics.org/plink/2.0
METAL v2011-03-25: https://genome.sph.umich.edu/wiki/METAL
MANTRA v1: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3460225/
COJO v1.92.2beta: https://yanglab.westlake.edu.cn/software/gcta/#COJO
PRS-CS v1.0.0: https://github.com/getian107/PRScs
PRS-CSx v1.0.0: https://github.com/getian107/PRScsx
Python implementation for SuSiE: https://github.com/getian107/SuSiEx
FinnGen QC and Association analysis: https://finngen.gitbook.io/documentation/methods/genotype-imputation/genotype-data
FinnGen GWAS: https://finngen.gitbook.io/documentation/methods/phewas
IEU open GWAS project: https://gwas.mrcieu.ac.uk/phewas/
VEP v104.3: https://useast.ensembl.org/info/docs/tools/vep/index.html
Cytoscape v3.9.1: https://cytoscape.org/
References
Chaney, A. Fast Facts About GI and Liver Diseases for Nurses (Springer Publishing Company, 2016).
GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 17–30 (2020).
M’Koma, A. E. Inflammatory bowel disease: an expanding global health problem. Clin. Med. Insights Gastroenterol. 6, 33–47 (2013).
de Lange, K. M. et al. Genome-wide association study implicates immune activation of multiple integrin genes in inflammatory bowel disease. Nat. Genet. 49, 256–261 (2017).
Jostins, L. et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 491, 119–124 (2012).
Liu, J. Z. et al. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat. Genet. 47, 979–986 (2015).
Jung, S. et al. Identification of three novel susceptibility loci for inflammatory bowel disease in Koreans in an extended genome-wide association study. J. Crohns Colitis 15, 1898–1907 (2021).
Yang, S.-K. et al. Identification of loci at 1q21 and 16q23 that affect susceptibility to inflammatory bowel disease in Koreans. Gastroenterology 151, 1096–1099 (2016).
Brant, S. R. et al. Genome-wide association study identifies African-specific susceptibility loci in African Americans with inflammatory bowel disease. Gastroenterology 152, 206–217 (2017).
Goyette, P. et al. High-density mapping of the MHC identifies a shared role for HLA-DRB1*01:03 in inflammatory bowel diseases and heterozygous advantage in ulcerative colitis. Nat. Genet. 47, 172–179 (2015).
Cleynen, I. et al. Inherited determinants of Crohn’s disease and ulcerative colitis phenotypes: a genetic association study. Lancet 387, 156–167 (2016).
Huang, H. et al. Fine-mapping inflammatory bowel disease loci to single-variant resolution. Nature 547, 173–178 (2017).
Lam, M. et al. Comparative genetic architectures of schizophrenia in East Asian and European populations. Nat. Genet. 51, 1670–1678 (2018).
Tang, C. S. et al. Exome-wide association analysis reveals novel coding sequence variants associated with lipid traits in Chinese. Nat. Commun. 6, 10206 (2015).
Hugot, J. P. et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature 411, 599–603 (2001).
Ogura, Y. et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature 411, 603–606 (2001).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51, 584–591 (2019).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Sazonovs, A. et al. Large-scale sequencing identifies multiple genes and rare variants associated with Crohn’s disease susceptibility. Nat. Genet. 54, 1275–1283 (2022).
Kanai, M. et al. Meta-analysis fine-mapping is often miscalibrated at single-variant resolution. Cell Genom. 2, 100210 (2022).
Rivas, M. A. et al. Deep resequencing of GWAS loci identifies independent rare variants associated with inflammatory bowel disease. Nat. Genet. 43, 1066–1073 (2011).
Rivas, M. A. et al. A protein-truncating R179X variant in RNF186 confers protection against ulcerative colitis. Nat. Commun. 7, 12342 (2016).
Lassen, K. G. et al. Genetic coding variant in GPR65 alters lysosomal pH and links lysosomal dysfunction with colitis risk. Immunity 44, 1392–1405 (2016).
Lavoie, S. et al. The Crohn’s disease polymorphism, ATG16L1 T300A, alters the gut microbiota and enhances the local Th1/Th17 response. eLife 8, e39982 (2019).
Varma, M. et al. Cell type- and stimulation-dependent transcriptional programs regulated by Atg16L1 and its Crohn’s disease risk variant T300A. J. Immunol. 205, 414–424 (2020).
Morris, A. P. Transethnic meta-analysis of genomewide association studies. Genet. Epidemiol. 35, 809–822 (2011).
Festen, E. A. M. et al. Genetic variants in the region harbouring IL2/IL21 associated with ulcerative colitis. Gut 58, 799–804 (2009).
Aoki, C. A. et al. Transforming growth factor beta (TGF-beta) and autoimmunity. Autoimmun. Rev. 4, 450–459 (2005).
Ihara, S., Hirata, Y. & Koike, K. TGF-β in inflammatory bowel disease: a key regulator of immune cells, epithelium, and the intestinal microbiota. J. Gastroenterol. 52, 777–787 (2017).
Kiryluk, K. et al. GWAS defines pathogenic signaling pathways and prioritizes drug targets for IgA nephropathy. Preprint at bioRxiv https://doi.org/10.1101/2021.11.19.21265383 (2021).
Ge, T., Chen, C.-Y., Ni, Y., Feng, Y.-C. A. & Smoller, J. W. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat. Commun. 10, 1776 (2019).
Hammer, T. & Langholz, E. The epidemiology of inflammatory bowel disease: balance between East and West? A narrative review. Dig. Med. Res. 3, 48 (2020).
Ruan, Y. et al. Improving polygenic prediction in ancestrally diverse populations. Nat. Genet. 54, 573–580 (2022).
Asano, K. et al. A genome-wide association study identifies three new susceptibility loci for ulcerative colitis in the Japanese population. Nat. Genet. 41, 1325–1329 (2009).
Yamazaki, K. et al. A genome-wide association study identifies 2 susceptibility loci for Crohn’s disease in a Japanese population. Gastroenterology 144, 781–788 (2013).
Yang, S.-K. et al. Genome-wide association study of ulcerative colitis in Koreans suggests extensive overlapping of genetic susceptibility with Caucasians. Inflamm. Bowel Dis. 19, 954–966 (2013).
Yang, S.-K. et al. Genome-wide association study of Crohn’s disease in Koreans revealed three new susceptibility loci and common attributes of genetic susceptibility across ethnic populations. Gut 63, 80–87 (2014).
Fuyuno, Y. et al. Genetic characteristics of inflammatory bowel disease in a Japanese population. J. Gastroenterol. 51, 672–681 (2016).
Yang, S.-K. et al. Immunochip analysis identification of 6 additional susceptibility loci for Crohn’s disease in Koreans. Inflamm. Bowel Dis. 21, 1–7 (2014).
Lee, H.-S. et al. X chromosome-wide association study identifies a susceptibility locus for inflammatory bowel disease in Koreans. J. Crohns Colitis 11, 820–830 (2017).
Kakuta, Y. et al. A genome-wide association study identifying RAP1A as a novel susceptibility gene for Crohn’s disease in Japanese individuals. J. Crohns Colitis 13, 648–658 (2019).
Okamoto, D. et al. Genetic analysis of ulcerative colitis in Japanese individuals using population-specific SNP array. Inflamm. Bowel Dis. 26, 1177–1187 (2020).
Ye, B. D. et al. Identification of ten additional susceptibility loci for ulcerative colitis through Immunochip analysis in Koreans. Inflamm. Bowel Dis. 22, 13–19 (2016).
Kanai, M. et al. Insights from complex trait fine-mapping across diverse populations. Preprint at bioRxiv https://doi.org/10.1101/2021.09.03.21262975 (2021).
Ye, B. D. et al. Association of FUT2 and ABO with Crohn’s disease in Koreans. J. Gastroenterol. Hepatol. 35, 104–109 (2020).
Magro, F. et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J. Crohns Colitis 11, 649–670 (2017).
Gomollón, F. et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1: diagnosis and medical management. J. Crohns Colitis 11, 3–25 (2017).
Sturm, A. et al. ECCO-ESGAR guideline for diagnostic assessment in IBD part 2: IBD scores and general principles and technical aspects. J. Crohns Colitis 13, 273–284 (2019).
Maaser, C. et al. ECCO-ESGAR guideline for diagnostic assessment in IBD part 1: initial diagnosis, monitoring of known IBD, detection of complications. J. Crohns Colitis 13, 144–164 (2019).
Kakuta, Y. et al. NUDT15 codon 139 is the best pharmacogenetic marker for predicting thiopurine-induced severe adverse events in Japanese patients with inflammatory bowel disease: a multicenter study. J. Gastroenterol. 53, 1065–1078 (2018).
Kakuta, Y. et al. Crohn’s disease and early exposure to thiopurines are independent risk factors for mosaic chromosomal alterations in patients with inflammatory bowel diseases. J. Crohns Colitis 16, 643–655 (2022).
Cortes, A. & Brown, M. A. Promise and pitfalls of the Immunochip. Arthritis Res. Ther. 13, 101 (2011).
Taliun, D. et al. Sequencing of 53,831 diverse genomes from the NHLBI TOPMed Program. Nature 590, 290–299 (2021).
Kawai, Y. et al. Japonica array: improved genotype imputation by designing a population-specific SNP array with 1070 Japanese individuals. J. Hum. Genet. 60, 581–587 (2015).
Wang, G., Sarkar, A., Carbonetto, P. & Stephens, M. A simple new approach to variable selection in regression, with application to genetic fine mapping. J. R. Stat. Soc. B 82, 1273–1300 (2020).
Yang, J. et al. Conditional and joint multiple-SNP analysis of GWAS summary statistics identifies additional variants influencing complex traits. Nat. Genet. 44, 369–375 (2012).
Bulik-Sullivan, B. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Lee, S. H., Wray, N. R., Goddard, M. E. & Visscher, P. M. Estimating missing heritability for disease from genome-wide association studies. Am. J. Hum. Genet. 88, 294–305 (2011).
Shi, H. et al. Population-specific causal disease effect sizes in functionally important regions impacted by selection. Nat. Commun. 12, 1098 (2021).
Park, S. H. et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong district of Seoul, Korea in 1986–2015. J. Crohns Colitis 13, 1410–1417 (2019).
Szklarczyk, D. et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 47, D607–D613 (2019).
Acknowledgements
Z.L. acknowledges support from the National Natural Science Foundation of China (91942312, 81630017). H.H. acknowledges support from NIDDK K01DK114379, NIDDK R01DK129364 and the Stanley Center for Psychiatric Research. M.L. acknowledges support from the National Natural Science Foundation of China (81870389, 82070565). Y. Kakuta and Y. Kinouchi acknowledge support from JSPS KAKENHI (21K07884, 21K07955), the Japan Agency for Medical Research and Development (AMED) (JP18kk0305002) and Labour Sciences Research Grants for Research on Intractable Diseases from the Ministry of Health, Labour and Welfare of Japan. Y. Kakuta, Y. Kawai, K.T. and M.N. acknowledge support from AMED (JP19km0405501). K.S. acknowledges support from the National Research Foundation of Korea (2017R1A2A1A05001119, 2020R1A2C2003275). J.C. acknowledges support from NIDDK U24DK062429 and NIDDK U01DK062422. D.P.B.M. acknowledges the Leona M. and Harry B. Helmsley Charitable Trust and NIDDK U01DK062413. K.T. and M.N. acknowledge support from AMED (JP19km0405205). Part of the computations on JPN1 was performed on the NIG supercomputer at the ROIS National Institute of Genetics. Computations on SHA1 were performed in a supercomputing environment at the Digital Health China Technologies Corp. Ltd. We want to acknowledge the participants and investigators of the FinnGen study. The FinnGen project is funded by two grants from Business Finland (HUS 4685/31/2016 and UH 4386/31/2016) and the following industry partners: AbbVie Inc., AstraZeneca UK Ltd., Biogen MA Inc., Bristol Myers Squibb (and Celgene Corporation & Celgene International II Sàrl), Genentech Inc., Merck Sharp & Dohme Corp, Pfizer Inc., GlaxoSmithKline Intellectual Property Development Ltd., Sanofi US Services Inc., Maze Therapeutics Inc., Janssen Biotech Inc., Novartis AG and Boehringer Ingelheim. The following biobanks are acknowledged for delivering biobank samples to FinnGen: Auria Biobank (www.auria.fi/biopankki), THL Biobank (www.thl.fi/biobank), Helsinki Biobank (www.helsinginbiopankki.fi), Biobank Borealis of Northern Finland (https://www.ppshp.fi/Tutkimus-ja-opetus/Biopankki/Pages/Biobank-Borealis-briefly-in-English.aspx), Finnish Clinical Biobank Tampere (www.tays.fi/en-US/Research_and_development/Finnish_Clinical_Biobank_Tampere), Biobank of Eastern Finland (www.ita-suomenbiopankki.fi/en), Central Finland Biobank (www.ksshp.fi/fi-FI/Potilaalle/Biopankki), Finnish Red Cross Blood Service Biobank (www.veripalvelu.fi/verenluovutus/biopankkitoiminta) and Terveystalo Biobank (www.terveystalo.com/fi/Yritystietoa/Terveystalo-Biopankki/Biopankki/). All Finnish Biobanks are members of BBMRI.fi infrastructure (www.bbmri.fi). Finnish Biobank Cooperative-FINBB (https://finbb.fi/) is the coordinator of BBMRI-ERIC operations in Finland. The Finnish biobank data can be accessed through the Fingenious services (https://site.fingenious.fi/en/) managed by FINBB.
Author information
Authors and Affiliations
Consortia
Contributions
Z.L., J.L., K.S., Y. Kakuta, M.L. and H.H. designed the study and supervised the work. Z.L., R.L., H.G., S.J., W.S., C.S., Z.G., K.Y., D.L., T.G., J.C., M.J.D., D.P.B.M., K.S., Y. Kakuta, M.L. and H.H. analyzed the data and helped in study management. Z.L., H.G., S.J., X.G., R.S., X.L., Y. Kim, H.-S.L., Y. Kawai, M.N., J.U., K.T., Y. Kinouchi, A.M., B.D.Y., K.S., Y. Kakuta and M.L. helped in recruitment, clinical phenotyping, analysis and/or leadership on study contribution. Z.L., R.L., H.G., S.Z., D.L., T.G., M.J.D., D.P.B.M., B.D.Y., K.S., Y. Kakuta, M.L. and H.H. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
W.S. and C.S. are employees of Digital Health China Technologies Corp. Ltd. M.J.D. is a founder of Maze Therapeutics. D.P.B.M. has received consultancy fees from Prometheus Biosciences, Prometheus Laboratories, Takeda, Gilead, Pfizer. Stock—Prometheus Biosciences. B.D.Y. has served on advisory boards for AbbVie Korea, Celltrion, Daewoong Pharma, Ferring Korea, Janssen Korea, Pfizer Korea and Takeda Korea; has received research grants from Celltrion and Pfizer Korea; has received consulting fees from Chong Kun Dang Pharm., CJ Red BIO, Cornerstones Health, Daewoong Pharma, IQVIA, Kangstem Biotech, Korea United Pharm. Inc., Medtronic Korea, NanoEntek and Takeda; and has received speaking fees from AbbVie Korea, Celltrion, Ferring Korea, IQVIA, Janssen Korea, Pfizer Korea, Takeda and Takeda Korea. H.H. received consultancy fees from Ono Pharmaceutical and an honorarium from Xian Janssen Pharmaceutical. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Genetics thanks the anonymous reviewers for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Quantile-Quantile plots for IBD genetic associations.
λ, genomic inflation factor; λ1000, scaled inflation factor for an equivalent study of 1,000 cases and 1,000 controls. The dots indicate variants. Shaded area indicates the 95% confidence interval under the null distribution. a-c, SHA1. d-f, ICH1 (only the designated null variants in ImmunoChip were used). g-i, KOR1. j-l, JPN1. m-o, Meta-analysis including all EAS samples (SHA1, ICH1, KOR1, and JPN1). p-r, FIN. a, d, g, j, m, and p are for CD. b, e, h, k, n, and q are for UC. c, f, i, l, o, and r are for IBD.
Extended Data Fig. 2 Index variants in the 16 new IBD loci in EAS.
a, Minor allele frequency (MAF) taken from 1000 Genomes EAS and EUR reference panels, respectively. b, P-value in respective studies.
Extended Data Fig. 3 Comparison between the fixed-effect (FE) meta-analysis and MANTRA.
Index variants in loci identified by either FE or MANTRA were plotted. For FE, we used genome-wide significance threshold of 5 × 10−8, and for MANTRA, we used the Bayes Factor threshold of 106, plotted as the vertical and horizontal lines respectively. P, P-value from FE. BF, Bayes factor from MANTRA.
Extended Data Fig. 4 IBD gene network.
IBD gene network was created using the STRING functional protein association networks and clustered using Community Clustering Glay (Methods). For clusters with more than two genes or with new IBD genes, the top three significantly enriched pathways were shown if false-discovery rate (FDR) < 0.05. New, nearest genes to the index variants in new IBD loci or new genes in Table 2 (boldfaced). Known, nearest genes to the index variants in known IBD loci. Index, nearest genes to the index variants in IBD loci except for those in Table 2. Tier, genes in Table 2.
Extended Data Fig. 5 Comparative genetic architecture within EAS.
a, SNP-based heritability in the liability scale with the prevalence in its respective population or the European population. b, Genetic correlation (rg). For a and b, the sample size used to derive SHA1, KOR1 and JPN1 h2 and their rg were 8,831, 6,038 and 2,624 for CD, and 8,679, 5,988 and 2,803 for UC, respectively. Results are plotted as mean value ± 95% confidence interval (error bar).
Extended Data Fig. 6 Quantile-Quantile plots for the heterogeneity test within EAS.
a, b, CD. c, d, UC. e, f, IBD. a, c, e, Genome-wide variants including the MHC locus. b, d, f, Genome-wide variants excluding the MHC locus. Cochran’s Q-test, two-sided, was used for the heterogeneity test. The dots indicate variants. Shaded area indicates the 95% confidence interval under the null distribution.
Extended Data Fig. 7 Enrichment of squared genetic correlation stratified across genomic annotations.
No significant enrichment or depletion (deviation from 1) was observed after Bonferroni corrections. Results are plotted as mean value ± 95% confidence interval before multiple testing corrections (error bar).
Extended Data Fig. 8 Variance explained for IBD associations across EUR and EAS.
We included all loci from Supplementary Table 8. For loci with fine-mapping analyses performed, we used the conditional OR (using COJO, Methods) for variants with the highest PIP in each credible set to account for multiple independent associations. We took fine-mapping results from ref. 12 for EUR and from this study for EAS. For loci with no fine-mapping results, we used the index variant (variant with the most significant P-value) as the proxy for the loci. We only plotted associations that have variance explained > 0.3% in either EAS or EUR. Different MAF is defined as Fst > 0.01, and different OR is defined as heterogeneity test P-value < 0.05 after Bonferroni correction. Because the heterogeneity test was corrected using a higher multiple testing burden, the significance for a handful of loci, for example, RNF186, can be different from Fig. 3c. Nearest genes to the associations were used as labels for associations when the text space is available.
Extended Data Fig. 9 Difference between variance explained for CD and UC across EUR and EAS.
Index variants from Supplementary Table 8 were plotted. Difference between variance explained was calculated as variance explained of CD − variance explained of UC.
Extended Data Fig. 10 Polygenic risk prediction on Chinese, Korean and Japanese study participants.
a, Leave-one-country-out strategy was performed to test the performance of PRS on SHA1 (Chinese), KOR1 (Korean), and JPN1 (Japanese) individuals, respectively. The prediction accuracy was measured as R2 on the liability scale using the population prevalence (Methods). For the testing cohort, we randomly split study participants into validation and testing 100 times (Methods). All other EAS cohorts were used as discovery. Results are plotted as mean value ± 95% confidence interval of R2 across the 100 replicates (error bar). b, Effective sample size of training datasets calculated as 4/(1/ncase + 1/ncontrol).
Supplementary information
Supplementary Information
Supplementary Note.
Supplementary Tables
Supplementary Tables 1–13.
Supplementary Data 1
Manhattan plot for IBD genetic associations.
Supplementary Data 2
Regional association plot for IBD-associated loci in EAS.
Supplementary Data 3
Forest plot for index variants in IBD-associated loci.
Supplementary Data 4
Forest plot for putative causal variants identified in EAS and in EUR.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Z., Liu, R., Gao, H. et al. Genetic architecture of the inflammatory bowel diseases across East Asian and European ancestries. Nat Genet 55, 796–806 (2023). https://doi.org/10.1038/s41588-023-01384-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41588-023-01384-0
This article is cited by
-
Transcriptome-wide association studies associated with Crohn’s disease: challenges and perspectives
Cell & Bioscience (2024)
-
Association between inflammatory bowel disease and cancer risk: evidence triangulation from genetic correlation, Mendelian randomization, and colocalization analyses across East Asian and European populations
BMC Medicine (2024)
-
Neutrophils: from IBD to the gut microbiota
Nature Reviews Gastroenterology & Hepatology (2024)
-
Real-world NUDT15 genotyping and thiopurine treatment optimization in inflammatory bowel disease: a multicenter study
Journal of Gastroenterology (2024)
-
Evaluating significance of European-associated index SNPs in the East Asian population for 31 complex phenotypes
BMC Genomics (2023)