Abstract
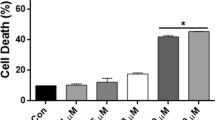
Atomoxetine (ATX) is a presynaptic norepinephrine transporter (NET) inhibitor widely prescribed for attention-deficit/hyperactivity disorder (ADHD) due to its low abuse potential and absence of psychostimulant effects. While NET inhibition is implicated in the clinical response, several additional pharmacoactivities may contribute to clinical efficacy or unwanted side effects. We recently reported that ATX can dose-dependently alter mitochondrial function and cellular redox status. Here, we assessed potential alterations in mitochondrial biogenesis, mitochondrial dynamics and cellular antioxidant capacity following high- and low-dose ATX treatment of differentiated human neuroblastoma cells. Human SH-SY5Y neuroblastoma cells were treated with ATX (1, 5, 10, 20 and 50 μM) for 7 days under differentiation culture conditions. Changes in the expression levels of protein markers for mitochondrial biogenesis, fusion and fission as well as of antioxidant proteins were analysed by Western blot. High-dose ATX (50 μM) reduced while low-dose ATX (10 μM) increased mitochondrial biogenesis as evidenced by parallel changes in SDHA, COX-I, PGC1α and TFAM expression. High-dose ATX also reduced mitochondrial fusion as evidenced by OPA1 and MFN2 downregulation, and mitochondrial fission as indicated by DRP1 and Fis1 downregulation. In contrast, ATX did not alter expression of the antioxidant enzymes SOD1 and catalase, the phase II transcription factor Nfr2, or the Nfr2-regulated antioxidant enzyme NQO1. Clinical responses and side effects of ATX may be mediated by dose-dependent modulation of mitochondrial biogenesis and dynamics as well as NET inhibition.






Similar content being viewed by others
Data Availability
All data presented and discussed are contained within the paper. All the data and materials are available from J.C.C.
References
Posner, J., Polanczyk, G. V., & Sonuga-Barke, E. (2020). Attention-deficit hyperactivity disorder. Lancet, 395(10222), 450–462. https://doi.org/10.1016/S0140-6736(19)33004-1.
Cortese, S. (2020). Pharmacologic Treatment of Attention Deficit-Hyperactivity Disorder. New England Journal of Medicine, 383(11), 1050–1056. https://doi.org/10.1056/NEJMra1917069.
Corona, J. C. (2018). Natural Compounds for the Management of Parkinson’s Disease and Attention-Deficit/Hyperactivity Disorder. BioMed Research International, 2018, 4067597 https://doi.org/10.1155/2018/4067597.
Corona, J. C. (2021). Pharmacological approaches for the treatment of Attention-deficit/hyperactivity disorder. In B. M. Kyser (ed), Attention-Deficit Hyperactivity Disorder: Diagnosis, Prevalence and Treatment (pp. 1–39). New York: Nova Science Publishers, Inc. pp.
Genro, J. P., Kieling, C., Rohde, L. A., & Hutz, M. H. (2010). Attention-deficit/hyperactivity disorder and the dopaminergic hypotheses. Expert Review of Neurotherapeutics, 10(4), 587–601. https://doi.org/10.1586/ern.10.17.
Swanson, J. M., Kinsbourne, M., Nigg, J., Lanphear, B., Stefanatos, G. A., Volkow, N., Taylor, E., Casey, B. J., Castellanos, F. X., & Wadhwa, P. D. (2007). Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine hypothesis. Neuropsychology Review, 17(1), 39–59. https://doi.org/10.1007/s11065-007-9019-9.
Prince, J. (2008). Catecholamine dysfunction in attention-deficit/hyperactivity disorder: an update. Journal of Clinical Psychopharmacology, 28(3 Suppl 2), S39–S45. https://doi.org/10.1097/JCP.0b013e318174f92a.
Del Campo, N., Chamberlain, S. R., Sahakian, B. J., & Robbins, T. W. (2011). The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biological Psychiatry, 69(12), e145–e157. https://doi.org/10.1016/j.biopsych.2011.02.036.
Bymaster, F. P., Katner, J. S., Nelson, D. L., Hemrick-Luecke, S. K., Threlkeld, P. G., Heiligenstein, J. H., Morin, S. M., Gehlert, D. R., & Perry, K. W. (2002). Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology, 27(5), 699–711. https://doi.org/10.1016/S0893-133X(02)00346-9.
Koda, K., Ago, Y., Cong, Y., Kita, Y., Takuma, K., & Matsuda, T. (2010). Effects of acute and chronic administration of atomoxetine and methylphenidate on extracellular levels of noradrenaline, dopamine and serotonin in the prefrontal cortex and striatum of mice. Journal of Neurochemistry, 114(1), 259–270. https://doi.org/10.1111/j.1471-4159.2010.06750.x.
Swanson, C. J., Perry, K. W., Koch-Krueger, S., Katner, J., Svensson, K. A., & Bymaster, F. P. (2006). Effect of the attention deficit/hyperactivity disorder drug atomoxetine on extracellular concentrations of norepinephrine and dopamine in several brain regions of the rat. Neuropharmacology, 50(6), 755–760. https://doi.org/10.1016/j.neuropharm.2005.11.022.
Moran-Gates, T., Zhang, K., Baldessarini, R. J., & Tarazi, F. I. (2005). Atomoxetine blocks motor hyperactivity in neonatal 6-hydroxydopamine-lesioned rats: implications for treatment of attention-deficit hyperactivity disorder. International Journal of Neuropsychopharmacology, 8(3), 439–444. https://doi.org/10.1017/S1461145705005249.
Corona, J. C., Carreon-Trujillo, S., Gonzalez-Perez, R., Gomez-Bautista, D., Vazquez-Gonzalez, D., & Salazar-Garcia, M. (2019). Atomoxetine produces oxidative stress and alters mitochondrial function in human neuron-like cells. Scientific Reports, 9(1), 13011 https://doi.org/10.1038/s41598-019-49609-9.
Ighodaro OMA, O.A. (2018). First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alexandria Journal of Medicine, 54(4), 287–293.
Corona, J. C., & Duchen, M. R. (2015). Impaired mitochondrial homeostasis and neurodegeneration: towards new therapeutic targets? Journal of Bioenergetics and Biomembranes, 47(1–2), 89–99. https://doi.org/10.1007/s10863-014-9576-6.
Nolfi-Donegan, D., Braganza, A., & Shiva, S. (2020). Mitochondrial electron transport chain: Oxidative phosphorylation, oxidant production, and methods of measurement. Redox Biology, 37, 101674 https://doi.org/10.1016/j.redox.2020.101674.
Giacomello, M., Pyakurel, A., Glytsou, C., & Scorrano, L. (2020). The cell biology of mitochondrial membrane dynamics. Nature Reviews Molecular Cell Biology, 21(4), 204–224. https://doi.org/10.1038/s41580-020-0210-7.
Tilokani, L., Nagashima, S., Paupe, V., & Prudent, J. (2018). Mitochondrial dynamics: overview of molecular mechanisms. Essays in Biochemistry, 62(3), 341–360. https://doi.org/10.1042/EBC20170104.
Flippo, K. H., & Strack, S. (2017). Mitochondrial dynamics in neuronal injury, development and plasticity. Journal of Cell Science, 130(4), 671–681. https://doi.org/10.1242/jcs.171017.
Sebastian, D., Palacin, M., & Zorzano, A. (2017). Mitochondrial Dynamics: Coupling Mitochondrial Fitness with Healthy Aging. Trends in Molecular Medicine, 23(3), 201–215. https://doi.org/10.1016/j.molmed.2017.01.003.
Yoo, S. M., & Jung, Y. K. (2018). A Molecular Approach to Mitophagy and Mitochondrial Dynamics. Molecules and Cells, 41(1), 18–26. https://doi.org/10.14348/molcells.2018.2277.
Corona, J. C., & Duchen, M. R. (2015). PPARgamma and PGC-1alpha as therapeutic targets in Parkinson’s. Neurochemical Research, 40(2), 308–316. https://doi.org/10.1007/s11064-014-1377-0.
Dominy J. E., Puigserver P. (2013). Mitochondrial biogenesis through activation of nuclear signaling proteins. Cold Spring Harbor Perspectives in Biology 5(7). https://doi.org/10.1101/cshperspect.a015008.
Puigserver, P., Wu, Z., Park, C. W., Graves, R., Wright, M., & Spiegelman, B. M. (1998). A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell, 92(6), 829–839. https://doi.org/10.1016/s0092-8674(00)81410-5.
Simmons, E. C., Scholpa, N. E., & Schnellmann, R. G. (2020). Mitochondrial biogenesis as a therapeutic target for traumatic and neurodegenerative CNS diseases. Experimental Neurology, 329, 113309 https://doi.org/10.1016/j.expneurol.2020.113309.
Flippo, K. H., Gnanasekaran, A., Perkins, G. A., Ajmal, A., Merrill, R. A., Dickey, A. S., Taylor, S. S., McKnight, G. S., Chauhan, A. K., Usachev, Y. M., & Strack, S. (2018). AKAP1 Protects from Cerebral Ischemic Stroke by Inhibiting Drp1-Dependent Mitochondrial Fission. Journal of Neuroscience, 38(38), 8233–8242. https://doi.org/10.1523/JNEUROSCI.0649-18.2018.
Corona, J. C., & Duchen, M. R. (2016). PPARgamma as a therapeutic target to rescue mitochondrial function in neurological disease. Free Radical Biology and Medicine, 100, 153–163. https://doi.org/10.1016/j.freeradbiomed.2016.06.023.
Golpich, M., Amini, E., Mohamed, Z., Azman Ali, R., Mohamed Ibrahim, N., & Ahmadiani, A. (2017). Mitochondrial Dysfunction and Biogenesis in Neurodegenerative diseases: Pathogenesis and Treatment. CNS Neuroscience & Therapeutics, 23(1), 5–22. https://doi.org/10.1111/cns.12655.
Jamwal, S., Blackburn, J. K., & Elsworth, J. D. (2021). PPARgamma/PGC1alpha signaling as a potential therapeutic target for mitochondrial biogenesis in neurodegenerative disorders. Pharmacology & Therapeutics, 219, 107705 https://doi.org/10.1016/j.pharmthera.2020.107705.
Alvarez-Arellano L., Gonzalez-Garcia N., Salazar-Garcia M., Corona J. C. (2020). Antioxidants as a Potential Target against Inflammation and Oxidative Stress in Attention-Deficit/Hyperactivity Disorder. Antioxidants 9(2). https://doi.org/10.3390/antiox9020176.
Joseph, N., Zhang-James, Y., Perl, A., & Faraone, S. V. (2015). Oxidative Stress and ADHD: A Meta-Analysis. Journal of Attention Disorders, 19(11), 915–924. https://doi.org/10.1177/1087054713510354.
Corona J. C. (2020) Role of Oxidative Stress and Neuroinflammation in Attention-Deficit/Hyperactivity Disorder. Antioxidants 9 (11). https://doi.org/10.3390/antiox9111039.
Lopresti, A. L. (2015). Oxidative and nitrosative stress in ADHD: possible causes and the potential of antioxidant-targeted therapies. Attention Deficit and Hyperactivity Disorders, 7(4), 237–247. https://doi.org/10.1007/s12402-015-0170-5.
Poljsak, B., Suput, D., & Milisav, I. (2013). Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxidative Medicine and Cellular Longevity, 2013, 956792 https://doi.org/10.1155/2013/956792.
He, L., He, T., Farrar, S., Ji, L., Liu, T., & Ma, X. (2017). Antioxidants Maintain Cellular Redox Homeostasis by Elimination of Reactive Oxygen Species. Cellular Physiology and Biochemistry, 44(2), 532–553. https://doi.org/10.1159/000485089.
El Adham, E. K., Hassan, A. I., & El Aziz El-Mahdy, A. A. (2011). Nutritional and Metabolic Disturbances in Attention Deficit Hyperactivity Disease. Research Journal of Medical Sciences, 6(1), 10–16.
Ceylan, M., Sener, S., Bayraktar, A. C., & Kavutcu, M. (2010). Oxidative imbalance in child and adolescent patients with attention-deficit/hyperactivity disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 34(8), 1491–1494. https://doi.org/10.1016/j.pnpbp.2010.08.010.
Nasim, S., Naeini, A. A., Najafi, M., Ghazvini, M., & Hassanzadeh, A. (2019). Relationship between Antioxidant Status and Attention Deficit Hyperactivity Disorder Among Children. International Journal of Preventive Medicine, 10, 41 https://doi.org/10.4103/ijpvm.IJPVM_80_18.
Comim, C. M., Gomes, K. M., Reus, G. Z., Petronilho, F., Ferreira, G. K., Streck, E. L., Dal-Pizzol, F., & Quevedo, J. (2014). Methylphenidate treatment causes oxidative stress and alters energetic metabolism in an animal model of attention-deficit hyperactivity disorder. Acta Neuropsychiatrica, 26(2), 96–103. https://doi.org/10.1017/neu.2013.35.
Schmitz, F., Scherer, E. B., Machado, F. R., da Cunha, A. A., Tagliari, B., Netto, C. A., & Wyse, A. T. (2012). Methylphenidate induces lipid and protein damage in prefrontal cortex, but not in cerebellum, striatum and hippocampus of juvenile rats. Metabolic Brain Disease, 27(4), 605–612. https://doi.org/10.1007/s11011-012-9335-5.
Motaghinejad, M., Motevalian, M., Shabab, B., & Fatima, S. (2017). Effects of acute doses of methylphenidate on inflammation and oxidative stress in isolated hippocampus and cerebral cortex of adult rats. Journal of Neural Transmission, 124(1), 121–131. https://doi.org/10.1007/s00702-016-1623-5.
Gomes, K. M., Petronilho, F. C., Mantovani, M., Garbelotto, T., Boeck, C. R., Dal-Pizzol, F., & Quevedo, J. (2008). Antioxidant enzyme activities following acute or chronic methylphenidate treatment in young rats. Neurochemical Research, 33(6), 1024–1027. https://doi.org/10.1007/s11064-007-9544-1.
Barygin, O. I., Nagaeva, E. I., Tikhonov, D. B., Belinskaya, D. A., Vanchakova, N. P., & Shestakova, N. N. (2017). Inhibition of the NMDA and AMPA receptor channels by antidepressants and antipsychotics. Brain Research 1660, 58–66. https://doi.org/10.1016/j.brainres.2017.01.028.
Ludolph, A. G., Udvardi, P. T., Schaz, U., Henes, C., Adolph, O., Weigt, H. U., Fegert, J. M., Boeckers, T. M., & Fohr, K. J. (2010). Atomoxetine acts as an NMDA receptor blocker in clinically relevant concentrations. British Journal of Pharmacology, 160(2), 283–291. https://doi.org/10.1111/j.1476-5381.2010.00707.x.
Jesinkey, S. R., Korrapati, M. C., Rasbach, K. A., Beeson, C. C., & Schnellmann, R. G. (2014). Atomoxetine prevents dexamethasone-induced skeletal muscle atrophy in mice. Journal of Pharmacology and Experimental Therapeutics, 351(3), 663–673. https://doi.org/10.1124/jpet.114.217380.
Reid, W. M., & Hamm, R. J. (2008). Post-injury atomoxetine treatment improves cognition following experimental traumatic brain injury. Journal of Neurotrauma, 25(3), 248–256. https://doi.org/10.1089/neu.2007.0389.
Hou, Q. X., Yu, L., Tian, S. Q., Jiang, C. J., Yang, W. J., & Wang, Z. J. (2016). Neuroprotective effects of atomoxetine against traumatic spinal cord injury in rats. Iranian Journal of Basic Medical Sciences, 19(3), 272–280.
Altunkaynak, B. Z., Onger, M. E., Turkmen, A. P., Yurt, K. K., Altun, G., & Yuce, M. (2016). Effects of Methylphenidate and Atomoxetine on Development of the Brain. In F. López-Muñoz, V. Srinivasan, D. de Berardis, C. Álamo & A. T. Kato (eds), Melatonin, Neuroprotective Agents and Antidepressant Therapy (pp. 825–845). New Delhi: Springer. pp.
Gur, F., Cengiz, M., & Gur, B. (2021). Alternations in nuclear factor kappa beta activity (NF-kB) in the rat brain due to long-term use of atomoxetine for treating ADHD: In vivo and in silico studies. Biochemical and Biophysical Research Communications, 534, 927–932. https://doi.org/10.1016/j.bbrc.2020.10.072.
Tian, C., Murrin, L. C., & Zheng, J. C. (2009). Mitochondrial fragmentation is involved in methamphetamine-induced cell death in rat hippocampal neural progenitor cells. PLoS ONE, 4(5), e5546 https://doi.org/10.1371/journal.pone.0005546.
Brillo V., Chieregato L., Leanza L., Muccioli S., Costa R. (2021). Mitochondrial Dynamics, ROS, and Cell Signaling: A Blended Overview. Life 11 (4). https://doi.org/10.3390/life11040332.
Willems, P. H. G. M., Rossignol, R., Dieteren, C. E. J., Murphy, M. P., & Koopman, W. J. H. (2015). Redox Homeostasis and Mitochondrial Dynamics. Cell Metabolism, 22(2), 207–218.
Jendrach, M., Mai, S., Pohl, S., Voth, M., & Bereiter-Hahn, J. (2008). Short- and long-term alterations of mitochondrial morphology, dynamics and mtDNA after transient oxidative stress. Mitochondrion, 8(4), 293–304. https://doi.org/10.1016/j.mito.2008.06.001.
Gur, F., Gur, B., Erkayman, B., Halici, Z., & Karakoc, A. (2020). Investigation of serum and brain superoxide dismutase levels depending on atomoxetine used in attention-deficit/hyperactivity disorder treatment: A combination of in vivo and molecular docking studies. Bioorganic Chemistry, 105, 104435 https://doi.org/10.1016/j.bioorg.2020.104435.
Dutt, M., Dharavath, R. N., Kaur, T., Chopra, K., & Sharma, S. (2020). Differential effects of alprazolam against methylphenidate-induced neurobehavioral alterations. Physiology & Behavior, 222, 112935 https://doi.org/10.1016/j.physbeh.2020.112935.
Udvardi, P. T., Fohr, K. J., Henes, C., Liebau, S., Dreyhaupt, J., Boeckers, T. M., & Ludolph, A. G. (2013). Atomoxetine affects transcription/translation of the NMDA receptor and the norepinephrine transporter in the rat brain–an in vivo study. Drug Design, Development and Therapy, 7, 1433–1446. https://doi.org/10.2147/DDDT.S50448.
Ramoz, N., Boni, C., Downing, A. M., Close, S. L., Peters, S. L., Prokop, A. M., Allen, A. J., Hamon, M., Purper-Ouakil, D., & Gorwood, P. (2009). A haplotype of the norepinephrine transporter (Net) gene Slc6a2 is associated with clinical response to atomoxetine in attention-deficit hyperactivity disorder (ADHD. Neuropsychopharmacology, 34(9), 2135–2142. https://doi.org/10.1038/npp.2009.39.
Funding
This work was supported by Fondos Federales HIM/2019/029 SSA. 1575.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Consent to Publish
All authors agreed with the content and gave explicit consent to submit before submission of the publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carreón-Trujillo, S., Vázquez-González, D. & Corona, J.C. Atomoxetine Decreases Mitochondrial Biogenesis, Fission and Fusion In Human Neuron-like Cells But Does Not Alter Antioxidant Defences. Cell Biochem Biophys 81, 105–115 (2023). https://doi.org/10.1007/s12013-022-01116-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-022-01116-x