Abstract
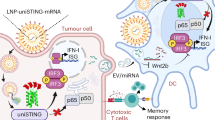
The clinical utility of stimulator of interferon genes (STING) agonists has been limited due to poor tumour-targeting and unwanted toxicity following systemic delivery. Here we describe a robust tumour-targeted STING agonist, ZnCDA, formed by the encapsulation of bacterial-derived cyclic dimeric adenosine monophosphate (CDA) in nanoscale coordination polymers. Intravenously injected ZnCDA prolongs CDA circulation and efficiently targets tumours, mediating robust anti-tumour effects in a diverse set of preclinical cancer models at a single dose. Our findings reveal that ZnCDA enhances tumour accumulation by disrupting endothelial cells in the tumour vasculature. ZnCDA preferentially targets tumour-associated macrophages to modulate antigen processing and presentation and subsequent priming of an anti-tumour T-cell response. ZnCDA reinvigorates the anti-tumour activity of both radiotherapy and immune checkpoint inhibitors in immunologically ‘cold’ pancreatic and glioma tumour models, offering a promising combination strategy for the treatment of intractable human cancers.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article and its Supplementary Information files. All raw sequencing data (SRA: PRJNA770747) are available online. The publicly available data used in this study are cited wherever relevant. Mouse reference genome (mm10): https://www.ncbi.nlm.nih.gov/grc/mouse; Molecular Signature Database: https://www.gsea-msigdb.org/gsea/msigdb/index.jsp.
References
Sun, L., Wu, J., Du, F., Chen, X. & Chen, Z. J. Cyclic GMP-AMP synthase is a cytosolic DNA sensor that activates the type I interferon pathway. Science 339, 786–791 (2013).
Wu, J. et al. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science 339, 826–830 (2013).
Ishikawa, H., Ma, Z. & Barber, G. N. STING regulates intracellular DNA-mediated, type I interferon-dependent innate immunity. Nature 461, 788–792 (2009).
Chen, Q., Sun, L. & Chen, Z. J. Regulation and function of the cGAS–STING pathway of cytosolic DNA sensing. Nat. Immunol. 17, 1142–1149 (2016).
Deng, L. et al. STING-dependent cytosolic DNA sensing promotes radiation-induced type I interferon-dependent antitumor immunity in immunogenic tumors. Immunity 41, 843–852 (2014).
Pantelidou, C. et al. PARP inhibitor efficacy depends on CD8+ T-cell recruitment via intratumoral sting pathway activation in BRCA-deficient models of triple-negative breast cancer. Cancer Discov. 9, 722–737 (2019).
Wang, Z. et al. cGAS/STING axis mediates a topoisomerase II inhibitor-induced tumor immunogenicity. J. Clin. Invest. 129, 4850–4862 (2019).
Parkes, E. E. et al. Activation of STING-dependent innate immune signaling by S-phase-specific DNA damage in breast cancer. J. Natl Cancer Inst. 109, djw199 (2017).
Mender, I. et al. Telomere stress potentiates STING-dependent anti-tumor immunity. Cancer Cell 38, 400–411.e6 (2020).
Lara, P. N. et al. Randomized phase III placebo-controlled trial of carboplatin and paclitaxel with or without the vascular disrupting agent vadimezan (ASA404) in advanced non-small-cell lung cancer. J. Clin. Oncol. 29, 2965–2971 (2011).
Gao, P. et al. Binding-pocket and lid-region substitutions render human STING sensitive to the species-specific drug DMXAA. Cell Rep. 8, 1668–1676 (2014).
Ding, C., Song, Z., Shen, A., Chen, T. & Zhang, A. Small molecules targeting the innate immune cGAS‒STING‒TBK1 signaling pathway. Acta Pharm. Sin. B 10, 2272–2298 (2020).
Meric-Bernstam, F. et al. Phase Ib study of MIW815 (ADU-S100) in combination with spartalizumab (PDR001) in patients (pts) with advanced/metastatic solid tumors or lymphomas. J. Clin. Oncol. 37, 2507–2507 (2019).
Pan, B. S. et al. An orally available non-nucleotide STING agonist with antitumor activity. Science https://doi.org/10.1126/science.aba6098 (2020).
Sun, X. et al. Amplifying STING activation by cyclic dinucleotide–manganese particles for local and systemic cancer metalloimmunotherapy. Nat. Nanotechnol. 16, 1260–1270 (2021).
Yao, Y. et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front. Mol. Biosci. 7, 193 (2020).
Irvine, D. J. & Dane, E. L. Enhancing cancer immunotherapy with nanomedicine. Nat. Rev. Immunol. 20, 321–334 (2020).
Sykes, E. A., Chen, J., Zheng, G. & Chan, W. C. W. Investigating the impact of nanoparticle size on active and passive tumor targeting efficiency. ACS Nano 8, 5696–5706 (2014).
Duan, X. et al. Immunostimulatory nanomedicines synergize with checkpoint blockade immunotherapy to eradicate colorectal tumors. Nat. Commun. 10, 1899 (2019).
Corrales, L. et al. Direct activation of STING in the tumor microenvironment leads to potent and systemic tumor regression and immunity. Cell Rep. 11, 1018–1030 (2015).
Lemos, H. et al. Overcoming resistance to STING agonist therapy to incite durable protective antitumor immunity. J. Immunother. Cancer 8, e001182 (2020).
Bulbake, U., Doppalapudi, S., Kommineni, N. & Khan, W. Liposomal formulations in clinical use: an updated review. Pharmaceutics 9, 12 (2017).
Fang, J., Nakamura, H. & Maeda, H. The EPR effect: unique features of tumor blood vessels for drug delivery, factors involved, and limitations and augmentation of the effect. Adv. Drug Deliv. Rev. 63, 136–151 (2011).
Kingston, B. R. et al. Specific endothelial cells govern nanoparticle entry into solid tumors. ACS Nano 15, 14080–14094 (2021).
Yang, H. et al. STING activation reprograms tumor vasculatures and synergizes with VEGFR2 blockade. J. Clin. Invest. 129, 4350–4364 (2019).
Barber, G. N. STING: infection, inflammation and cancer. Nat. Rev. Immunol. 15, 760–770 (2015).
Xia, T., Konno, H., Ahn, J. & Barber, G. N. Deregulation of STING signaling in colorectal carcinoma constrains DNA damage responses and correlates with tumorigenesis. Cell Rep. 14, 282–297 (2016).
Sangfelt, O. & Strander, H. Apoptosis and cell growth inhibition as antitumor effector functions of interferons. Med. Oncol. 18, 3–14 (2001).
Ivashkiv, L. B. IFNγ: signalling, epigenetics and roles in immunity, metabolism, disease and cancer immunotherapy. Nat. Rev. Immunol. 18, 545–558 (2018).
Gao, Y. et al. γδ T cells provide an early source of interferon γ in tumor immunity. J. Exp. Med. 198, 433–442 (2003).
Adachi, K. & Chiba, K. FTY720 story. Its discovery and the following accelerated development of sphingosine 1-phosphate receptor agonists as immunomodulators based on reverse pharmacology. Perspect. Med. Chem. 1, 11–23 (2007).
Zheng, W. et al. Combination of radiotherapy and vaccination overcome checkpoint blockade resistance. Oncotarget 7, 43039–43051 (2016).
Siddiqui, I. et al. Intratumoral Tcf1+PD-1+CD8+ T cells with stem-like properties promote tumor control in response to vaccination and checkpoint blockade immunotherapy. Immunity 50, 195–211.e10 (2019).
Cheng, N. et al. A nanoparticle-incorporated STING activator enhances antitumor immunity in PD-L1-insensitive models of triple-negative breast cancer. JCI insight https://doi.org/10.1172/jci.insight.120638 (2018).
Ohkuri, T., Kosaka, A., Nagato, T. & Kobayashi, H. Effects of STING stimulation on macrophages: STING agonists polarize into ‘classically’ or ‘alternatively’ activated macrophages? Hum. Vaccin. Immunother. 14, 285–287 (2018).
You, L. et al. The crosstalk between autophagic and endo-/exosomal pathways in antigen processing for MHC presentation in anticancer T cell immune responses. J. Hematol. Oncol. 10, 165 (2017).
Delamarre, L., Pack, M., Chang, H., Mellman, I. & Trombetta, E. S. Differential lysosomal proteolysis in antigen-presenting cells determines antigen fate. Science 307, 1630–1634 (2005).
Wu, J., Dobbs, N., Yang, K. & Yan, N. Interferon-independent activities of mammalian STING mediate antiviral response and tumor immune evasion. Immunity 53, 115–126.e5 (2020).
Smyth, M. J., Ngiow, S. F., Ribas, A. & Teng, M. W. L. Combination cancer immunotherapies tailored to the tumour microenvironment. Nat. Rev. Clin. Oncol. 13, 143–158 (2016).
Bush, N. A. O., Chang, S. M. & Berger, M. S. Current and future strategies for treatment of glioma. Neurosurgic. Rev. 40, 1–14 (2017).
Filippone, A. et al. PD1/PD-L1 immune checkpoint as a potential target for preventing brain tumor progression. Cancer Immunol. Immunother. 71, 2067–2075 (2022).
Ranoa, D. R. E. et al. Molecular cell biology STING promotes homeostasis via regulation of cell proliferation and chromosomal stability. Cancer Res. 79, 1465–1479 (2019).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet. J. 17, 10–12 (2011).
Kim, D., Paggi, J. M., Park, C., Bennett, C. & Salzberg, S. L. Graph-based genome alignment and genotyping with HISAT2 and HISAT-genotype. Nat. Biotechnol. 37, 907–915 (2019).
Liao, Y., Smyth, G. K. & Shi, W. FeatureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics https://doi.org/10.1093/bioinformatics/btt656 (2014).
Costa-Silva, J., Domingues, D. & Lopes, F. M. RNA-Seq differential expression analysis: an extended review and a software tool. PLoS ONE 12, e0190152 (2017).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Orecchioni, M., Ghosheh, Y., Pramod, A. B. & Ley, K. Macrophage polarization: different gene signatures in M1(Lps+) vs. classically and M2(LPS–) vs. alternatively activated macrophages. Front. Immunol. https://doi.org/10.3389/fimmu.2019.01084 (2019).
Acknowledgements
We are grateful to Z. Sun, A. Arina, S. P. Pitroda and T. Luo for helpful discussions, and R. Torres for technical assistance. We thank A. K. Huser for editing the manuscript. This work was supported by a grant from the Ludwig Foundation and an NIH grant (R01CA262508) to R.R.W., NIH grants (R01CA223184 and R01CA216436) to W.L. and NIH grants (R35CA232109 and R01AI141333) to J.P.Y.T. A.P. is the recipient of a Walter Benjamin scholarship provided by the German Research Foundation (Deutsche Forschungsgemeinschaft). J.B. was supported by a Clinical Therapeutics Training Grant (T32GM007019). We acknowledge the technical support from the University of Chicago Human Tissue Resource Center (RRID: SCR_019199), Animal Studies Core (P30CA014599), Microscopy Core (P30CA014599), Flow Cytometry Core (RRID: SCR_017760) and Mass Spectrometry Facility (CHE-1048528).
Author information
Authors and Affiliations
Contributions
K.Y., W.H., W.L. and R.R.W. conceived the study; K.Y. designed the experiments; W.H. and X.J. prepared the nanoparticles; K.Y., W.H., X.J., A.P., C.H., S.L., Z.X., X.H., W.Z. and L.W. performed the experiments; K.Y. and J.W. performed mouse genotyping; K.Y., W.H., X.J. and A.P. analysed the data; J.B., H.L., J.P.Y.T. and Y.-X.F. contributed resources; K.Y., J.B., W.L. and R.R.W. drafted and finalized the manuscript with input from all other authors.
Corresponding authors
Ethics declarations
Competing interests
R.R.W. has stock and other ownership interests with Boost Therapeutics, Immvira, Reflexion Pharmaceuticals, Coordination Pharmaceuticals, Magi Therapeutics and Oncosenescence. R.R.W. has served in a consulting or advisory role for Aettis, AstraZeneca, Coordination Pharmaceuticals, Genus, Merck Serono, Nano proteagen, NKMax America and Shuttle Pharmaceuticals. R.R.W. has a patent pending entitled ’Methods and kits for diagnosis and triage of patients with colorectal liver metastases’ (US Patent application no. PCT/US2019/028071). R.R.W. has received research grant funding from Varian and Regeneron. R.R.W. has received compensation, including travel, accommodations or expense reimbursement, from AstraZeneca, Boehringer Ingelheim and Merck Serono. W.L. is the founder and chairman of Coordination Pharmaceuticals, which licensed the NCP technology from the University of Chicago. The other authors have no competing interests.
Peer review
Peer review information
Nature Nanotechnology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–10.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, K., Han, W., Jiang, X. et al. Zinc cyclic di-AMP nanoparticles target and suppress tumours via endothelial STING activation and tumour-associated macrophage reinvigoration. Nat. Nanotechnol. 17, 1322–1331 (2022). https://doi.org/10.1038/s41565-022-01225-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41565-022-01225-x
This article is cited by
-
Nanomaterial-encapsulated STING agonists for immune modulation in cancer therapy
Biomarker Research (2024)
-
Nanoparticles in tumor microenvironment remodeling and cancer immunotherapy
Journal of Hematology & Oncology (2024)
-
Glioma-associated macrophages: unraveling their dual role in the microenvironment and therapeutic implications
Current Medicine (2024)
-
Exploring the crosstalk between endothelial cells, immune cells, and immune checkpoints in the tumor microenvironment: new insights and therapeutic implications
Cell Death & Disease (2023)
-
Regulating metalloimmunology with nanomedicine for cancer therapy
Nano Research (2023)