Abstract
Background
The COVID-19 pandemic required immediate systematic change in healthcare delivery. Many institutions relied on telemedicine as an alternative to in-person visits. There is limited data in the bariatric surgery literature to determine how telemedicine impacts patient volume. This study evaluates the effects of using telemedicine for introductory bariatric surgery seminars on patient volume at a single institution.
Methods
A retrospective review was performed before and after implementing virtual introductory seminars for bariatric surgery patients at a comprehensive metabolic and surgery center. The effect on attendance rates for introductory seminars and completion rates of bariatric surgery was evaluated.
Results
The introductory seminar attendance rate for the in-person/pre-telemedicine period, April 2019 to February 2020, was compared to that of the virtual/post-telemedicine period, June 2020 to April 2021. A total of 836 patients registered for an introductory seminar during the pre-telemedicine period with a 65.79% attendance rate. In the post-telemedicine period, 806 patients registered with a 67.87% attendance rate, which was not statistically different (p = 0.37, 95% CI − 0.03–0.07). Completion rates of bariatric surgery were analyzed using June 2019 to October 2019 as the pre-telemedicine period and June 2020 to October 2020 as the post-telemedicine period. Similarly, there was no difference between the pre-telemedicine surgery rate of 23.43% and post-telemedicine surgery rate of 19.68% (p = 0.31, 95% CI − 0.11–0.04).
Conclusion
Despite abruptly transitioning to virtual introductory bariatric seminars, there was no change in attendance rates nor was there a difference in the number of patients progressing through the program and undergoing bariatric surgery at our institution. This demonstrates similar efficacy of telemedicine and in-person introductory seminars for bariatric surgery patients, which supports telemedicine as a promising tool for this patient population in the post-pandemic era.
Graphical abstract

Similar content being viewed by others
There are several pre-operative requirements patients must meet prior to gaining approval for bariatric surgery [1]. In addition to demonstrating the medical necessity for bariatric surgery, patients must complete psychological-behavioral evaluations, nutritional evaluations, and obtain clearance by the surgical team. Many institutions, including ours, also require patients to first attend an Introduction to Bariatric Surgery Seminar prior to starting the pre-operative evaluation process. This introductory seminar provides patients with a basic overview of the bariatric surgery program and allows them to ask questions prior to making any commitments.
However, the COVID-19 pandemic disrupted the normal work flow throughout healthcare systems and many bariatric surgery programs were forced to incorporate telemedicine encounters into their pre- and post-operative patient encounters. One study in Poland found that 92% of surgeons reported that the care for their bariatric patients now incorporates an element of telemedicine since the COVID-19 pandemic began [2], which appears to be the trend worldwide. Our institution transitioned completely to virtual introductory bariatric surgery seminars without an in-person option. Since attending the introductory seminar at our institution is a required first step prior to enrollment in the bariatric surgery program, it is important to understand the effects of transitioning to a telemedicine platform on patient volume. The impact that telemedicine has on patient volume, attrition, and completion rates of bariatric surgery is not clearly defined in the literature. This study aims to evaluate the effect on attendance rates for introductory seminars and completion rates of bariatric surgery before and after transitioning to a telemedicine platform for the Introductory to bariatric surgery seminars at a single institution.
Materials and methods
At the beginning of the COVID-19 pandemic, a virtual Introduction to Bariatric Surgery seminar was developed for patients interested in bariatric surgery. During this time, our institution transitioned solely to virtual introductory seminars and no longer offered in-person seminars in order to maintain safety for our patients and healthcare providers. After gaining Institutional Review Boards (IRB) approval, a retrospective review of clinical records from our Bariatric Surgery Center before and after the implementation of virtual introductory seminars was performed. The purpose of this study is to evaluate the effect on (1) attendance rates for introductory seminars and (2) completion rates of bariatric surgery before and after transitioning to a telemedicine platform for the Introductory to bariatric surgery seminars. It is important to note that although introductory seminars transitioned completely to a virtual platform, all clinic visits remained in-person throughout the study period. This is a single-institution study conducted from the Bariatric and Metabolic Center of Excellence within the Department of Surgery at Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire, which is a large, tertiary-care healthcare system in a rural setting.
All patients who registered for an Introduction to Bariatric Surgery Seminar during the pre-telemedicine and post-telemedicine study dates were eligible for inclusion in the study. Patients were 18 years or older. For analysis of the introductory seminar attendance rates, pre-telemedicine data was collected during an 11-month period from April 2019 to February 2020 to establish a baseline and compared to post-telemedicine data collected during an 11-month period from June 2020 to April 2021. However, for analysis of bariatric surgery completion rates, the periods analyzed were shorter in duration [5 months instead of 11 months] to allow time for patients to progress through the program after attending a virtual introductory seminar and undergo bariatric surgery in the post-telemedicine group. Therefore, for analysis of bariatric surgery completion rates, pre-telemedicine data was collected during a 5-month period from June 2019 to October 2019 to establish a baseline and compared to post-telemedicine data collected during a 5-month period from June 2020 to October 2020. Two weight-loss surgeries are offered at our institution, either gastric bypass or sleeve gastrectomy. The number of gastric bypasses versus sleeve gastrectomies were also analyzed before and after implementing virtual introductory seminars. Patients were excluded if they attended multiple introductory seminars both before and after implementing the telemedicine platform.
Statistical analysis was performed with Stata Statistics/Data Analysis, Special Edition 17, StataCorp LLC, College Station, Texas. Univariate analysis was accomplished with student’s t test. A p value of ≤ 0.05 was determined to be statistically significant.
Results
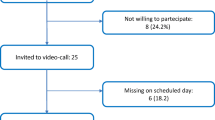
Seventeen patients were excluded from the study who attended multiple introductory seminars both before and after implementing telemedicine seminars. During the 11-month, pre-telemedicine period from April 2019 to February 2020, a total of 836 patients registered for an in-person Introduction to Bariatric Surgery seminar (Fig. 1). Of these patients, the attendance rate for the introductory seminar was 65.79%. After transitioning to virtual introductory seminars, a total of 806 patients registered during the 11-month, post-telemedicine period from June 2020 to April 2021. Of these patients, the attendance rate was 67.87%, which was slightly improved but not statistically different than the in-person, pre-pandemic attendance rate (p = 0.37, 95% CI − 0.03–0.07, Fig. 1).
Completion rates of bariatric surgery were analyzed during a shorter, 5-month period, before and after implementing virtual introduction to bariatric surgery seminars. During the 5-month, pre-telemedicine period from June 2019 to October 2019, a total of 239 attended an in-person introductory seminar (Table 1). Of these patients, 56 progressed through the program and completed bariatric surgery. During the 5-month, post-pandemic period from June 2020 to October 2020, a total of 249 attended a virtual introductory seminar. Of these patients, 49 progressed through the program and completed bariatric surgery. There was no statistical difference between the in-person, pre-telemedicine surgery rate of 23.43% and virtual, post-telemedicine surgery rate of 19.68% (p = 0.31, 95% CI − 0.11–0.04, Table 1).
More patients who attended a virtual introductory seminar underwent gastric bypass surgery compared to those who attended an in-person seminar (p = 0.04, 95% CI 0.01–0.38, Fig. 2). Out of the 56 patients who completed bariatric surgery during the pre-telemedicine period from June 2019 to October 2019, 26 patients underwent sleeve gastrectomy and 30 underwent gastric bypass surgery. Out of the 49 patients who completed bariatric surgery during the post-telemedicine period from June 2020 to October 2020, 13 patients underwent sleeve gastrectomy and 36 underwent gastric bypass surgery.
Discussion
The abrupt transition to virtual Introduction to bariatric surgery seminars did not affect the attendance rate of these seminars, nor did it affect the number of patients progressing through the program and ultimately undergoing bariatric surgery at our institution during the COVID-19 pandemic. More patients who attended a virtual introductory seminar underwent gastric bypass surgery instead of a sleeve gastrectomy compared to those who attended an in-person seminar. The clinical relevance of this is unclear and likely due to the small sample size.
It is interesting that there was not a decrease in seminar attendance nor in surgery completion rates considering the socioeconomic constraints for patients during this time. At the beginning of the study period in June 2020, the pandemic had resulted in over 4.3 million confirmed cases and over 290,000 deaths globally [3], leading to travel restrictions, border shutdowns, and quarantine mandates. This significantly reduced the workforce across all economic sectors. Many businesses were forced to close, leading to a rise in unemployment rates and loss of insurance status for many. High healthcare costs, shortages of personal protective equipment, and low numbers of ICU beds and ventilators continued to impede healthcare delivery [3]. During the initial COVID surge, our program canceled elective surgeries, including bariatric operations. Therefore, this study did not evaluate the initial few months of the pandemic (March–May 2020) and instead started in June 2020 when elective surgeries resumed. Despite ongoing socioeconomic hardships, our bariatric surgery volume quickly returned to numbers similar to those of the pre-pandemic era. Alternatively, offering a virtual platform for patients in this rural academic setting likely helped to offset the socioeconomic burden by improving access to care and convenience for patients. Patients may have preferred the virtual method of healthcare delivery to avoid the risk of COVID exposure during an in-person visit, but this data was not captured in our study. The back log of patients needing bariatric surgery who had been canceled during the initial shutdown may have also contributed to the increased case volume observed during the pandemic period. Obese individuals with several comorbidities may have been more willing to undergo bariatric surgery since an improvement in metabolic abnormalities has been linked to lower rates of ICU admissions, morbidity, and mortality in those with obesity who become infected with COVID [4]. Anecdotally, many practices experienced increased patient volume during the pandemic, likely due to all of these social, economic, and psychological factors which are difficult to measure.
The clinical benefit of using telehealth for the bariatric surgery population has been well established. Eaton, et al. demonstrated that patients retain more information using a telemedicine platform for the introductory seminars compared to in-person seminars in a cohort of 338 patients [5]. Sherf-Dagan, et al. similarly demonstrated significantly improved nutrition knowledge in a 200-patient trial for patients who watched an online lecture 1–2 weeks prior to surgery compared to the control group who received standard clinic visits without an online lecture [6]. Increased physical fitness [7], improved weight loss [8, 9], and eating habits [8, 10] as well as overall high patient satisfaction [7, 11,12,13,14,15] have also been reported when incorporating telemedicine into the care for bariatric surgery patients. However, these studies do not address in a unifying manner the effect that telemedicine has on patient volume, attrition, or completion rates of the program.
There are mixed results on the reported impact of telemedicine on bariatric surgery volumes and patient accrual and retention rates. Chao et al. found a 38% improvement in no-show rates after implementing telehealth pre-operative clinic visits during the COVID-19 pandemic compared to the year prior [16]. However, Brown et al. evaluated the impact of transitioning to virtual clinic visits (new and follow-up) for bariatric surgery patients during the COVID-19 pandemic and found a 75% decrease in new visits for surgeons after telehealth implementation [17]. Attributable reasons were multifactorial, including the pandemic’s effect on insurance status and unemployment rates, technological limitations, and patient preferences. On the other hand, Wang et al. found no difference in post-operative appointment attendance between telemedicine patients compared with non-telemedicine patients [18], and Lodewijks et al. found no difference in the numbers of patients approved for bariatric surgery by the obesity team after transitioning to telehealth for initial screenings [19]. Our findings similarly did not show a difference in introductory seminar attendance rates or completion rates of bariatric surgery after implementing virtual introductory seminars.
For programs interested in implementing a telehealth component to their practice, the practical aspects of our virtual introductory seminars involved several components. The Webex platform was used, which required the host to register for a new user account. Introductory seminars were hosted every 2 weeks on Friday afternoons by the metabolic and bariatric surgery team, consisting of office administrators, advanced practice providers, nutritionists and surgeons. Patients interested in bariatric surgery were required to register for the introductory seminar on our hospital website and attend prior to scheduling pre-operative clinic appointments. Patients were provided a link to the Webex meeting and logged in at the scheduled time. Patients could simply login as a guest on the Webex website, or they could download the Webex application on their computers or personal devices and register for an account if they wished. Usernames were hidden from each other to maintain anonymity and HIPPA compliance. The bariatric team presented the material in a live format, using Powerpoint slides to discuss the nutritional, psychological, and surgical components of bariatric surgery as well as insurance coverage details (Fig. 3). During the presentation, the chat function was available for questions but patients’ video and speaker functions were disabled. Questions from the chat were answered at the end of each session.
The limitations of this study include its retrospective study design. There are also several unmeasured, confounding variables with regard to the socioeconomic factors associated with the COVID-19 pandemic on bariatric surgery patients that must be kept in mind when interpreting the outcomes of this study. Another limitation to consider is how this study only evaluates the effect of virtual introductory seminars, not virtual clinic visits, or any other aspect of the bariatric surgery program. There are many factors that contribute to patient progression through bariatric surgery programs as well as attrition rates that are not addressed in this study. Larger, prospective studies are needed to more clearly delineate these associations.
Conclusion
While the clinical benefit of incorporating telemedicine into the care of bariatric surgery patients has been well-established, the effect of telemedicine on patient accrual and retention rates is variable in the literature. This study supports the use of telemedicine for introductory bariatric surgery seminars with no difference in seminar attendance rates or bariatric surgery completion rates throughout the COVID-19 pandemic. Larger, prospective studies are needed for a better understanding of the effects of telemedicine on bariatric clinic and surgery volumes.
References
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J, Urman RD, Adams S, Cleek JB, Correa R, Figaro MK, Flanders K, Grams J, Hurley DL, Kothari S, Seger MV, Still CD (2019) Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures—2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, the Obesity Society. Am Soc Me Endocr Pract 25(12):1346–1359
Major P, Stefura T, Wysocki M, Małczak P, Rzepa A, Proczko-Stepaniak M, Szeliga J, Pędziwiatr M (2020) Impact of SARS-CoV-2 pandemic on bariatric care in Poland: results of national survey. BMC Surg 20(1):314
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg 2020(78):185–193. https://doi.org/10.1016/j.ijsu.2020.04.018
Aminian A, Fathalizadeh A, Tu C, Butsch WS, Pantalone KM, Griebeler ML, Kashyap SR, Rosenthal RJ, Burguera B, Nissen SE (2021) Association of prior metabolic and bariatric surgery with severity of coronavirus disease 2019 (COVID-19) in patients with obesity. Surg Obes Relat Dis 17(1):208–214
Eaton L, Walsh C, Magnuson T, Schweitzer M, Lidor A, Nguyen H, Steele K (2012) On-line bariatric surgery information session as effective as in-person information session. Surg Obes Relat Dis 8(2):225–229
Sherf-Dagan S, Hod K, Mardy-Tilbor L, Gliksman S, Ben-Porat T, Sakran N, Zelber-Sagi S, Goitein D, Raziel A (2018) The effect of pre-surgery information online lecture on nutrition knowledge and anxiety among bariatric surgery candidates. Obes Surg 28(7):1876–1885
Baillot A, Boissy P, Tousignant M, Langlois MF (2017) Feasibility and effect of in-home physical exercise training delivered via telehealth before bariatric surgery. J Telemed Telecare 23:529–535
Bradley LE, Forman EM, Kerrigan SG, Goldstein SP, Butryn ML, Thomas JG, Herbert JD, Sarwer DB (2017) Project HELP: a remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg 27:586–598
Versteegden DPA, Scheerhoorn J, Van Himbeeck MJJ, Smulders JF, de Hingh IH, Nienhuijs SW (2021) The value of an e-health platform in bariatric surgery: a retrospective study on the impact on weight loss. Telemed J E-Health 27(11):1241–1248
Weineland S, Arvidsson D, Kakoulidis TP, Dahl J (2012) Acceptance and commitment therapy for bariatric surgery patients, a pilot RCT. Obes Res Clin Pract 6(1):e1–e90
Vilallonga R, Lecube A, Fort JM, Boleko MA, Hidalgo M, Armengol M (2013) Internet of things and bariatric surgery follow-up: comparative study of standard and IoT follow-up. Minim Invasive Ther Allied Technol 22(5):304–311
Sudan R, Salter M, Lynch T, Jacobs DO (2011) Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 202(1):71–76
Sada A, Harmsen WS, McKenzie TJ, Kellogg TA, Ghanem O, Kendrick ML, Habermann EB (2021) Telemedicine video follow-up for bariatric surgery patients: what do patients prefer? A prepandemic pilot randomized clinical trial. Am Surg. https://doi.org/10.1177/00031348211054547
Vosburg RW, Robinson KA, Gao C, Kim JJ (2021) Patient and provider satisfaction with telemedicine in a comprehensive weight management program. Telemed J E-Health 28(3):384–390
Maurice AP, Punnasseril JEJ, King SE, Dodd BR (2020) Improving access to bariatric surgery for rural and remote patients: experiences from a state-wide bariatric telehealth service in Australia. Obes Surg 30(11):4401–4410
Chao GF, Ehlers AP, Ellimoottil C, Varban OA, Dimick JB, Telem DA (2021) Convergent mixed methods exploration of telehealth in bariatric surgery: maximizing provider resources and access. Obes Surg 31(4):1877–1881
Brown AM, Ardila-Gatas J, Yuan V, Devas N, Docimo S, Spaniolas K, Pryor AD (2020) The impact of telemedicine adoption on a multidisciplinary bariatric surgery practice during the COVID-19 pandemic. Ann Surg 272(6):e306–e310
Wang CD, Rajaratnam T, Stall B, Hawa R, Sockalingam S (2019) Exploring the effects of telemedicine on bariatric surgery follow-up: a matched case control study. Obes Surg 29(8):2704–2706
Lodewijks Y, Nienhuijs S (2022) Bariatric telescreening during the COVID-19 pandemic: holding back for direct approval? Obes Surg 32(4):1072–1076
Acknowledgements
We would like to thank Kristin Slack, our administrative coordinator, who helped with data collection, organization, and management as well as Irma Allen who also helped with data collection. We would like to thank our dedicated team of bariatric administrators, nutritionists, and advanced practice providers who helped develop and conduct the virtual introductory seminars: Kristin Slack, Darcy Smith, Jennifer Letendre, Sarah Lange, Corinne Kelliher, and Clara Spalding.
Funding
No sources to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kaela E. Parnell, Justin Philip, Sarah E. Billmeier, Thadeus L. Trus have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Parnell, K.E., Philip, J., Billmeier, S.E. et al. The effects of using telemedicine for introductory bariatric surgery seminars during the COVID-19 pandemic. Surg Endosc 37, 5509–5515 (2023). https://doi.org/10.1007/s00464-022-09640-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09640-w