Abstract
Purpose
The aim of this study is to identify risk factors associated with postoperative DJF in long constructs for ASD.
Methods
A retrospective review was performed at a tertiary referral spine centre from 01/01/2007 to 31/12/2016. Demographic, clinical and radiographic parameters were collated for patients with DJF in the postoperative period and compared to those without DJF. Survival analyses were performed using univariate logistic regression to identify variables with a p value < 0.05 for inclusion in multivariate analysis. Spearman’s correlations were performed where applicable.
Results
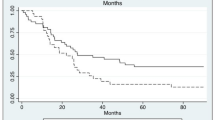
One hundred two patients were identified. 41 (40.2%) suffered DJF in the postoperative period, with rod fracture being the most common sign of DJF (13/65; 20.0%). Mean time to failure was 32.4 months. On univariate analysis, pedicle subtraction osteotomy (p = 0.03), transforaminal lumbar interbody fusion (p < 0.001), pre-op LL (p < 0.01), pre-op SVA (p < 0.01), pre-op SS (p = 0.02), postop LL (p = 0.03), postop SVA (p = 0.01), postop PI/LL (p < 0.001), LL correction (p < 0.001), SVA correction (p < 0.001), PT correction (p = 0.03), PI/LL correction (p < 0.001), SS correction (p = 0.03) all proved significant. On multivariate analysis, pedicle subtraction osteotomy (OR 27.3; p = 0.03), postop SVA (p < 0.01) and LL correction (p = 0.02) remained statistically significant as independent risk factors for DJF.
Conclusion
Recently, DJF has received recognition as its own entity due to a notable postoperative incidence. Few studies to date have evaluated risk factors for DJF. The results of our study highlight that pedicle subtraction osteotomy, poor correction of lumbar lordosis, and sagittal vertical axis are significantly associated with postoperative occurrence of DJF.



Similar content being viewed by others
References
Smith JS, Shaffrey CI, Fu KM, Scheer JK, Bess S, Schwab F et al (2013) Clinical and radiographic evaluation of the adult spinal deformity patient. Neurosurg Clin N Am 24:143–156. https://doi.org/10.1016/j.nec.2012.12.009
Zanirato A, Damilano M, Formica M, Piazzolla A, Lovi A, Villafañe JH et al (2018) Complications in adult spine deformity surgery: a systematic review of the recent literature with reporting of aggregated incidences. Eur Spine J 27(9):2272–2284. https://doi.org/10.1007/s00586-018-5535-y
Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ et al (2014) Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine 39(10):E607–E614. https://doi.org/10.1097/BRS.0000000000000266
Passias PG, Vasquez-Montes D, Poorman GW, Protopsaltis T, Horn SR, Bortz CA (2018) Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J 18(12):2187–2194. https://doi.org/10.1016/j.spinee.2018.04.017
McCarthy I, O’Brien M, Ames C, Robinson C, Errico T et al (2014) Incremental cost-effectiveness of adult spinal deformity surgery: observed quality-adjusted life years with surgery compared with predicted quality-adjusted life years without surgery. Neurosurg Focus 36(5):E3. https://doi.org/10.3171/2014.3.FOCUS1415
Schlenk RP, Kowalski RJ, Benzel EC (2003) Biomechanics of spinal deformity. Neurosurg Focus 14(1):1–15. https://doi.org/10.3171/foc.2003.14.1.3
Floccari LV, Su AW, McIntosh AL, Rathjen K, Shaughnessy WJ, Larson AN (2019) Distal junctional failure following pediatric spinal fusion. J Pediat Orthop 39(4):202–208. https://doi.org/10.1097/BPO.0000000000000898
Cho W, Mason JR, Smith JS, Shimer AS, Wilson AL, Shaffrey CI et al (2013) Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity: clinical and radiographic risk factors. J Neurosurg Spine 19:445–453. https://doi.org/10.3171/2013.6.SPINE121129
Zhu F, Bao H, Liu Z, Bentley M, Zhu Z, Ding Y, Qiu Y (2014) Unanticipated revision surgery in adult spinal deformity. Spine 39:B36-44. https://doi.org/10.1097/BRS.0000000000000463
Barton C, Noshchenko A, Patel VV, Cain CMJ, Christopher K, Burger EL (2017) Different types of mechanical complications after surgical correction of adult spine deformity with osteotomy. World J Meta Anal 5(6):132–149. https://doi.org/10.13105/wjma.v5.i6.132
Chang KW, Cheng CW, Chen HC, Chang KI, Chen TC (2008) Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine 33(13):1470–1477. https://doi.org/10.1097/BRS.0b013e3181753bcd
Dalle Ore CL, Ames CP, Deviren V, Lau D (2018) Outcomes following single-stage posterior vertebral column resection for severe thoracic kyphosis. World Neurosurg 119:E551–E559. https://doi.org/10.1016/j.wneu.2018.07.209
Dickson DD, Lenke LG, Bridwell KH, Koester LA (2014) Risk factors for and assessment of symptomatic pseudarthrosis after lumbar pedicle subtraction osteotomy in adult spinal deformity. Spine 39(15):1190–1195. https://doi.org/10.1097/BRS.0000000000000380
Kim JS, Phan K, Cheung ZB, Lee N, Vargas L, Arbind V, Merrill RK et al (2018) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Global Spine J 9(1):32–40. https://doi.org/10.1177/2192568218761362
Le Huec JC, Cogniet A, Demezon H, Rigal J, Saddiki R, Aunoble S (2014) Insufficient restoration of lumbar lordosis and FBI index following pedicle subtraction osteotomy is an indicator of likely mechanical complication. Eur Spine J 24(S1):112–120. https://doi.org/10.1007/s00586-014-3659-2
Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K (2003) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 85(A):454–463. https://doi.org/10.2106/00004623-200303000-00009
Lavage V, Schwab F, Vira S, Hart R, Burton D, Smith SJ, Boachie Adjei O et al (2011) Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine 14:184–191. https://doi.org/10.3171/2010.9.SPINE10129
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH (2007) Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Pjila Pa 1976) 32:2238–2244. https://doi.org/10.1097/BRS.0b013e31814cf24a
Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine (Phila Pa 1976) 37:1667–1675. https://doi.org/10.1097/BRS.0b013e3182552fd0
Roussouly P, Berthonnaud E, Dimnet J (2003) Geometrical and mechanical analysis of lumbar lordosis in an asymptomatic population: proposed classification. Rev Chir Orthop Reparatrice Appar Mot 89(7):632–639
Janik TJ, Harrison DD, Cailliet R, Troyanovich SJ, Harrison DE (1998) Can the sagittal lumbar curvature be closely approximated by an ellipse? J Orthop Res 16:766–770. https://doi.org/10.1002/jor.1100160620
Alzakri A, Boissière L, Cawley DT, Bourghil A, Pointillart V, Gille O et al (2018) L5 pedicle subtraction osteotomy: indication, surgical technique and specificities. Eur Spine J 27:644–651. https://doi.org/10.1007/s00586-017-5403-1
Butler JS, Lui DF, Malhotra K, Suarez-Huerta ML, Yu H, Selvadurai S et al (2019) 360-Degree complex primary reconstruction using porous tantalum cages for adult degenerative spinal deformity. Global Spine J 9(6):613–618. https://doi.org/10.1177/2192568218814531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McDonnell, J.M., Evans, S.R., Ahern, D.P. et al. Risk factors for distal junctional failure in long-construct instrumentation for adult spinal deformity. Eur Spine J 31, 3654–3661 (2022). https://doi.org/10.1007/s00586-022-07396-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07396-4