- 1Department of General Surgery, Peking University First Hospital, Beijing, China
- 2Department of Endoscopy Center, Peking University First Hospital, Beijing, China
- 3Department of General Surgery, Tianjin Fifth Centre Hospital, Tianjin, China
Objectives: The effects of early drain removal (EDR) on postoperative complications after pancreaticoduodenectomy (PD) remains to be investigated. This single-center retrospective cohort study was designed to explore the safety of EDR after PD.
Methods: A total of 112 patients undergoing PD with drain fluid amylase (DFA) on postoperative day (POD) 1 and 3 <= 5000 were divided into EDR and late drain removal (LDR). Propensity Score Matching (PSM) was used. We compared postoperative outcomes between two groups and explore the risk factors of total complications using univariate and multiple logistic regression analyses.
Results: No statistical differences were found in primary outcomes, including Grade B/C postoperative pancreatic fistula (POPF) (Original cohort: 5.71% vs. 3.90%; P = 1.000; PSM cohort: 3.33% vs. 6.67%; P = 1.000), and total complications (Original cohort: 17.14% vs. 32.47%; P = 0.093; PSM cohort: 13.33% vs. 33.33%; P = 0.067). The EDR was associated with shorter in-hospital stay (Original cohort: 11 days vs. 15 days; P < 0.0001; PSM cohort: 11 days vs. 15 days; P < 0.0001).
Conclusions: EDR on POD 3 is safe for patients undergoing PD with low risk of POPF.
Introduction
With the rapid development of surgical technique in the last decades, the perioperative mortality of pancreaticoduodenectomy (PD) decreased significantly, whereas the incidences of postoperative complications are still high (1–3). The postoperative pancreatic fistula (POPF) remains one of the most significant postoperative complications after PD, which significantly increases postoperative in-hospital stay and medical burden (4). A growing body of study proposed the predicted models to evaluate the risk of POPF after pancreatic surgery (5, 6). The management of intraperitoneal drainage plays a crucial role in the process of postoperative recovery of patients undergoing PD. The detection of drain fluid around the operative area is perceived as an important indicator for early identifying POPF, postpancreatectomy hemorrhage (PPH) or intra-abdominal infection, therefore prophylactic drainage placement during PD is accepted in most of pancreatic centers (7). However, many studies raised concerns about the placement of intraperitoneal drainage after PD. For example, Conlon et al. (8) performed the first randomized controlled trial (RCT) to demonstrate that the placement of drainage after pancreatic resection failed to reduce postoperative complications, but increased the incidences of intra-abdominal collections and infection. Subsequently, multiple RCTs and meta-analysis proved the safety of omission of drainage after pancreatic resection (9–13). However, one RCT was stopped because of the significantly increased mortality from 3% to 12% for patients undergoing PD without the placement of intraperitoneal drainage (14). Therefore, no consensus was reached with regard to whether to place prophylactic intraperitoneal drainage.
Recently, multiple studies paid more attention to evaluating the feasibility of EDR. Bassi et al. (15) performed the first RCT to explore the safety of EDR, and results showed that EDR significantly decreased complications, in-hospital stay and costs than late drain removal (LDR). Thereafter, Dai et al. (16, 17) performed single and multiple-center RCT to compare EDR and LDR regarding Clavien-Dindo grades 2–4 complications. The strict inclusion criteria were used to select patients with low or middle risk of POPF, which demonstrated EDR is safe in selected patients. The American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) was also utilized to explore the effects of EDR on postoperative complications for PD. EDR after PD was associated with better outcomes (18). Although the safety of EDR after PD was proved preliminarily, the low risk patient selection criteria and the time-point of EDR remains to be further explored.
Here, we designed single-center retrospective cohort study to the confirm the safety of EDR on POD 3 for PD patients with the low risk of POPF. A total of 112 patients undergoing PD with drain fluid amylase (DFA) on POD 1 and 3 <= 5000 were divided into EDR and LDR groups. Propensity Score Matching (PSM) was used. We found that there were no significant differences in Grade B/C POPF and total complications. In addition, EDR was associated with shorter in-hospital stay.
Methods
Single-center study design
This retrospective cohort study was approved by the Ethical Committee on Peking University First Hospital (Approval No.2021-636) and performed in accordance with the Helsinki Declaration. The consecutive patients undergoing pancreaticoduodenectomy (PD) or pylorus preserving PD (PPPD) from January 2017 and December 2020 in our institution with drain fluid amylase (DFA) on both postoperative day (POD) 1 and 3 ≤ 5000 U/L were enrolled. Specific exclusion criteria consisted in (a) patients underwent distal pancreatectomy (DP) or total pancreatectomy; (b) DFA on POD 1 or 3 > 5000 U/L; (c) patients with age < 18; (d) incomplete records of key postoperative outcomes.
The time-point of early and late drain removal was defined as POD 3 and ≥ POD 5. All the operations were performed by experienced pancreatic surgeons at our institution. Clinicopathological data were collected retrospectively through electronic medical record system.
The primary and secondary outcomes in single-center study
Postoperative complications were evaluated using the Clavien–Dindo classification system (19). The postoperative complications such as postoperative pancreatic fistula (POPF) (20), delayed gastric emptying (DGE) (21), and postpancreatectomy hemorrhage (PPH) (22) were in accordance with the consensus definition of the International Study Group of Pancreatic Fistula (ISGPF). Intra-abdominal collections were defined as collection of fluid measuring at least 3 cm in diameter demonstrated by ultrasound or CT scan. The primary outcomes in this study included Grade B/C POPF and total complications. The secondary outcomes were DGE, PPH, intra-abdominal collections, wound infection, re-operation, re-admission and post-operative in-hospital stay.
Propensity score matching
Propensity Score Matching was used to deal with confounding factors using R package “MatchIt”. Matching variables included age, BMI, pancreatitis, diabetes, cardiovascular disease, soft pancreatic texture, operation time, blood loss, diameter of main pancreatic duct, PPPD, vascular resection, ASA scores, pathology. The nearest neighbor matching method with a tolerate of 0.1 was selected.
Statistical analysis
Data was summarized as mean ± standard deviation or median (interquartile range, IQR) for continuous variables subjected to normal distribution or no normal distribution. The independent-samples t test and Mann-Whitney U test was performed to compare continuous variables between two groups. For categorical variables, data was summarized as frequency (ratio) and the chi-square test, fisher exact test, or rank sum test was used. Study of potential prognostic factors for total complications was carried out using univariate and multiple logistic regression analyses. All statistical analyses were conducted using SPSS version 22.0 software (SPSS22, Chicago, USA). Statistical significance was defined as p < 0.05.
Results
Characteristics of patients in single-center study
A total of 112 patients who underwent PD performed at our institution between January 2017 and December 2020 were divided into two groups: EDR (n = 35, drains were removed on POD 3) and LDR (n = 77, drains were removed on or beyond POD 5). Patients with amylase value in drains on POD 1 or 3 > 5000 U/L were excluded. The patients previously enrolled in the multi-center study performed by Peking Union Medical College Hospital were not included in our cohort.
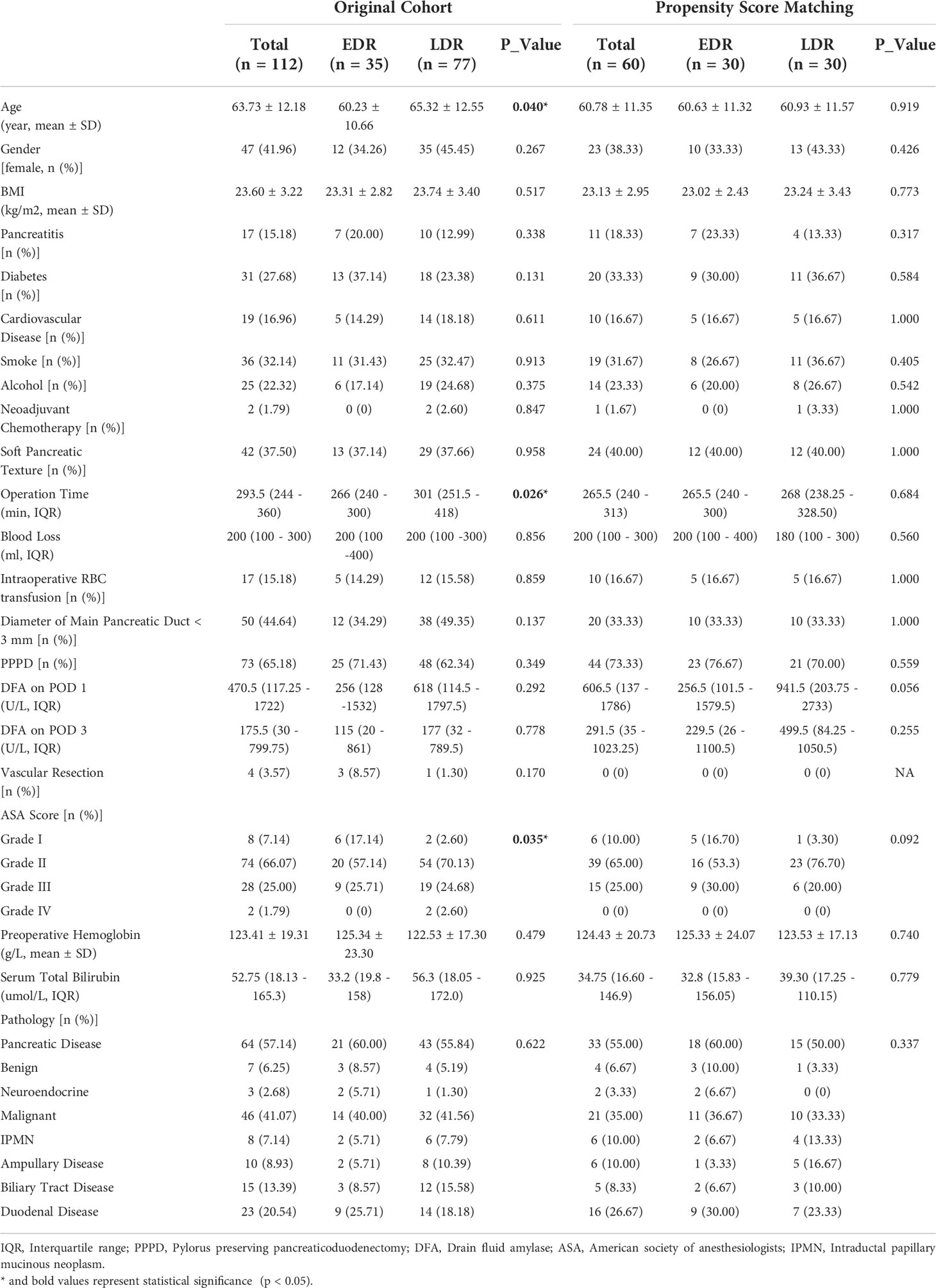
The demographic, surgical, biochemical, and pathological characteristics of patients were summarized in Table 1. There were no significant differences in gender, BMI, pancreatitis, diabetes, cardiovascular disease, smoke, alcohol, intraoperative RBC transfusion, PPPD, vascular resection, preoperative hemoglobin, serum total bilirubin, and pathology between two groups. No significant differences were found as well with particular regard to risk factors of POPF (soft pancreatic texture, blood loss, diameter of main pancreatic duct, DFA on POD 1/3). Only two patients underwent neoadjuvant chemotherapy (2 in EDR, 0 in LDR, P = 0.847). Patients in EDR had lower age (60.23 ± 10.66 vs. 65.32 ± 12.55; P = 0.04), shorter operation time (266 [240 – 300] vs. 301 [251.5 - 418]; P = 0.026), and different ASA scores (Grade I: 17.14% vs. Grade I: 2.60%; P = 0.035) in comparison with LDR. In order to reduce the impact of confounding factors to make two groups more homogeneous, Propensity Score Matching (PSM) was conducted. After PSM, all demographic, surgical, biochemical characteristics, and risk factors of POPF were similar without significant differences between these two groups (Table 1). In addition, the drain placement time was 3 days in EDR group versus 11 days (3 - 15.75) in LDR group (Table 2).
Primary and secondary outcomes in single-center study
Table 2 described postoperative complications of enrolled participants. There were no statistical differences between EDR and LDR group in primary outcomes, including Grade B/C POPF (Original cohort: 5.71% vs. 3.90%; P = 1.000; PSM cohort: 3.33% vs. 6.67%; P = 1.000), and total complications (Original cohort: 17.14% vs. 32.47%; P = 0.093; PSM cohort: 13.33% vs. 33.33%; P = 0.067).
EDR was associated with a decrease of Grade 2-4 complications (Original cohort: 11.43% vs. 28.57%; P = 0.046; PSM cohort: 6.67% vs. 26.67%; P = 0.038), post-operative in-hospital stay (Original cohort: 11 [9 - 14] vs. 15 [12.5 – 22.5]; P < 0.0001; PSM cohort: 11 [9 - 14] vs. 15 [11.75 – 21.5]; P < 0.0001). No significant differences were observed in single abdominal complications, including PPH (Original cohort: 0 vs. 5.19%; P = 0.307; PSM cohort: 0 vs. 6.67%; P = 0.492), intra-abdominal infection (Original cohort: 0 vs. 9.09%; P = 0.096; PSM cohort: 0 vs. 10.00%; P = 0.237), delayed gastric emptying (Original cohort: 8.57 vs. 11.69%; P = 0.869; PSM cohort: 6.67 vs. 6.67%; P = 1.000), and intra-abdominal fluid collections (Original cohort: 8.57 vs. 5.19%; P = 0.792; PSM cohort: 6.67 vs. 6.67%; P = 1.000). The rates of biliary fistula, wound infection, pulmonary complications between two groups were also comparable. The mortality, intervention, re-admission re-operation occurred in 0/0/3/0 patients in EDR group versus 2/3/2/1 patients in LDR group without significant differences. After PSM, the results were the same.
Exploring risk factors of total complications after PD
The correlation analysis of total complications and multiple characteristics were summarized in Table 3. Total complications were related to age, operation time, ASA scores, serum total bilirubin, and pathology. After continuous variables being converted into categorical variables, univariate logistic regression was performed, and the result showed that pathological characteristic was related to total complications. Early drain removal decreased slightly the total complications rate, but it was not significant difference (OR = 0.430; P = 0.098) (Table 4). Finally, the variables (P < 0.1) were included into multivariate logistic regression analysis, which also proved that only pathological characteristic was the independent risk factor associated with the incidence of total complications compared with benign pancreatic diseases (IPMN: OR = 0.087; P = 0.024; duodenal disease: OR = 0.098; P = 0.049) (Table 4).
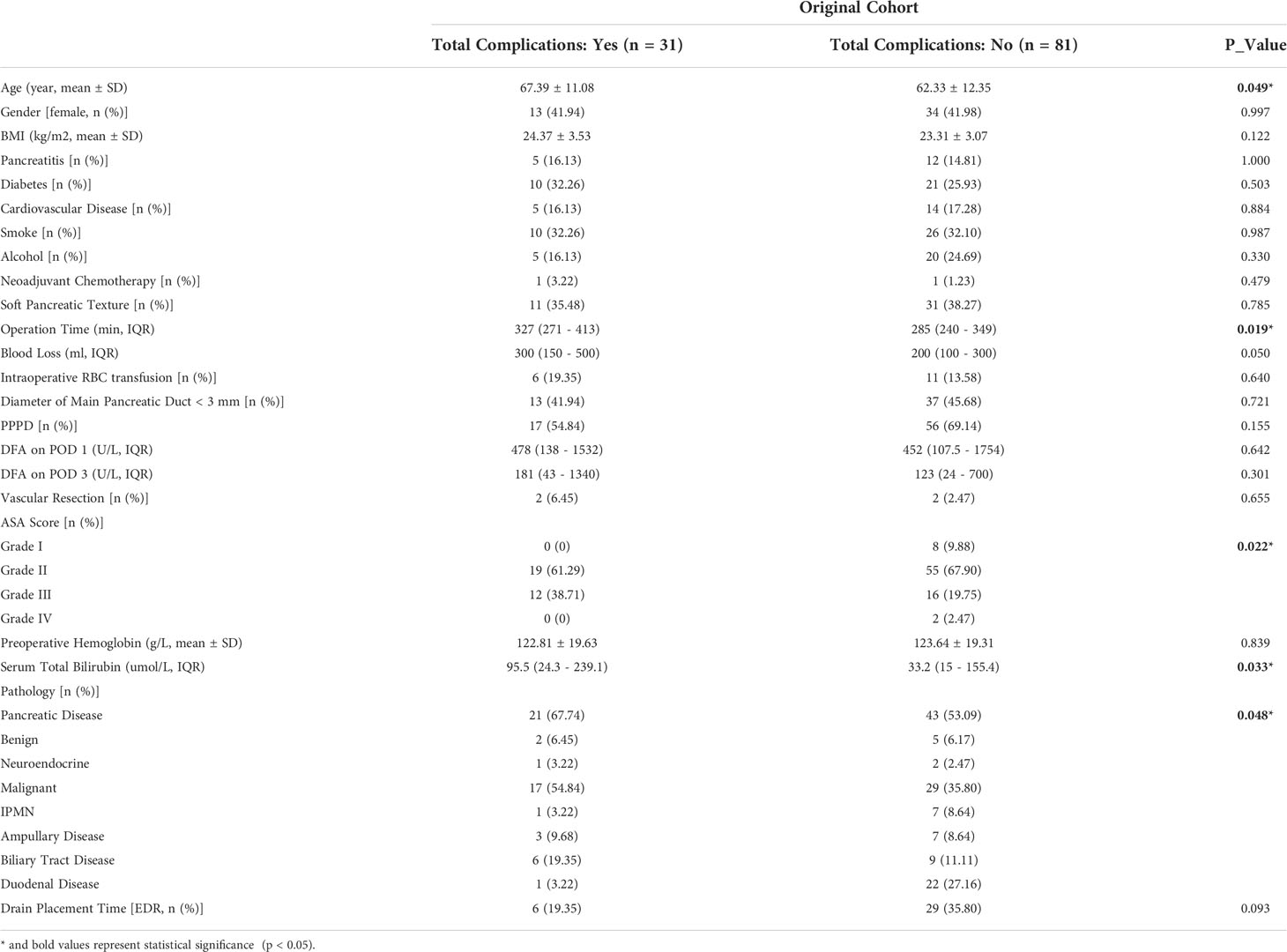
Table 3 Correlation analysis of total complications of enrolled participants in retrospective cohort study.
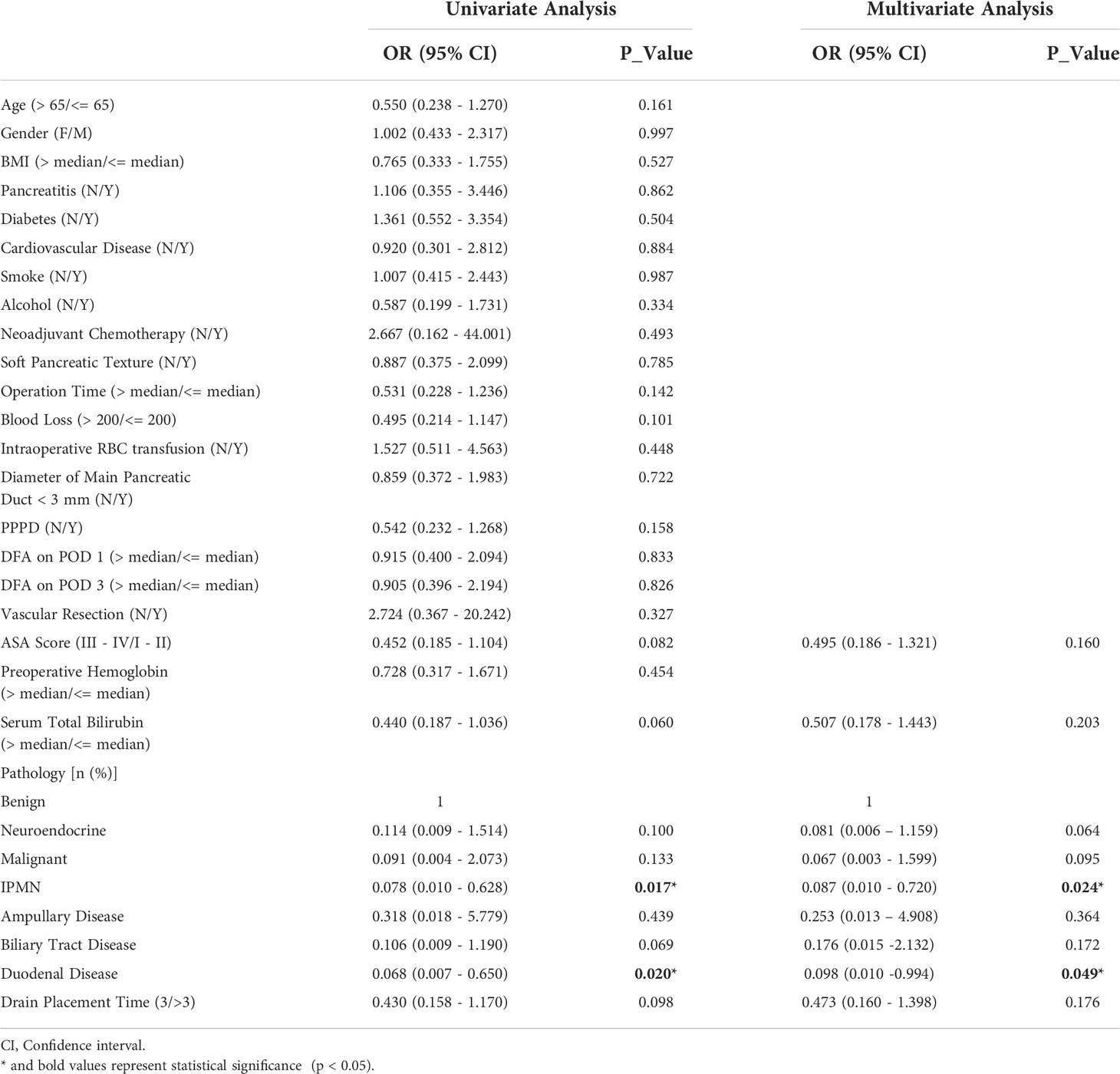
Table 4 Univariate and multivariate logistic regression of total complications of enrolled participants in retrospective cohort study.
Management of postoperative pancreatic fistula
In total, the rate of Grade B/C POPF was 4.46% (5/112), which occurred in 2 patients in EDR and 3 patients in LDR (P = 1.000). Low Grade B/C POPF rate indicated that low risk patient selection strategy (DFA on POD 1 and 3 <= 5000 U/L) works. EDR group had 2 grade B POPF. In contrast, LDR had 2 grade B POPF and 1 grade C POPF. Postoperative course of patients with pancreatic fistula were recorded in (Table 5). The patient had grade C POPF in LDR group even though DFA on POD 1 and 3 < 40 U/L, who underwent PD because of cholangiocarcinoma. Drains were removed on POD 8. Reoperation was conducted to explore for dehiscence of the anastomotic stoma and hemorrhage, which significantly extended in-hospital stay for 77 days, and finally caused mortality. Three of five patients with Grade B/C POPF had positive drain fluid cultures, thus antibiotic therapy was established according to drug sensitivity test. Percutaneous drain insertion or conservative treatment were used for grade B POPF.
Discussion
One of major concerns of EDR is intra-abdominal fluid collection, and caused infection and hemorrhage. This single-center study indicated that EDR could not increase the risk of intra-abdominal fluid collection and hemorrhage. The selection strategy of low risk patients: DFA on POD 1 <= 5000 U/L was utilized by previous studies (15–18, 23), and low Grade B/C POPF rate was observed in these studies. Single and multiple-center RCT performed by Dai and our single-center retrospective study used the stricter selection criteria (DFA on POD 1 and 3 <= 5000 U/L). The Grade B/C POPF rates were 1.75%, 5.13%, and 4.46% respectively. The strict selection strategy guarantees the safety of early drain removal, and aid in surgeon confidence to make a decision of EDR. However, the stricter selection strategy will narrow the clinical application of EDR. Thus, it is very important to balance selection criteria and the range of clinical application of EDR. Nowadays, the selection strategy for low risk of POPF, time-point of EDR, DFA cut-off value remains to be further investigated.
The definitions of EDR and LDR varied among previous studies. Bassi et al. (15) chose POD 3 as EDR time-point because the change of drain effluent happens on POD 3 which is also regarded as relatively early time-point, and POD 5 as LDR time-point because POD 5 is standard drain removal time-point in their institution. In our single-center study, we also chose POD 3 as EDR time-point, and >= POD 5 as LDR time-point that is the same as RCTs performed by Dai et al. (16, 17). It is better to select appropriate time-point of EDR and LDR according to local medical conditions. Our single-center study supported that EDR is safe and significantly decrease postoperative in-hospital stay (11 [9 – 14] vs. 15 [12.5 - 22.5]), indicating that faster recovery, lower medical costs for patients, in line with the idea of enhanced recovery after surgery (ERAS). In additions, Dai et al. (17) found late drain removal and laparoscopic procedure were the independent risk factors of major complications using multiple regression analysis. However, our single-center study did not prove the LDR was an independent risk factor of total complications (OR = 0.473, 95% CI: 0.160 - 1.398; P = 0.176), which might be attributed to small sample size.
Our work provides an evidence for the safety of EDR, and help promote the practice of ERAS after PD. However, there are some limitations in this study, such as (a) single-center retrospective cohort study with limited sample size; (b) relatively strict low risk patient selection criteria to narrow the clinical application range of EDR; (c) single-center study only focus on PD, the safety of EDR for DP remains to be explored.
In conclusion, our study demonstrates that early drain removal on POD 3 is safe for patients following PD with low risk of POPF.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by This retrospective cohort study was approved by the Ethical Committee on Peking University First Hospital (Approval No.2021-636). The ethics committee waived the requirement of written informed consent for participation.
Author contributions
Conceptualization, KC, XDT. Literature Search, KC, XHX, ZHL. Data Collection, KC, YSM. Formal Analysis, KC. Validation, KC, XHX, FW, SPZ, ZJS, and XDT. Investigation and Visualization, KC. Methodology, KC and XDT. Writing – original draft, KC. Project administration, YMY. Writing – review & editing XDT. Supervision, XDT and YMY. All authors read and approved the final version of the manuscript.
Funding
This study was supported by The Natural Science Foundation of China (NO.82171722, 81871954) and Beijing Municipal Natural Science Foundation (NO.7212111).
Acknowledgments
We would like to thank all the patients enrolled at Peking University First Hospital, Qi Wang for statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med (2014) 371(11):1039–49. doi: 10.1056/NEJMra1404198
2. Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. Pancreatic cancer. Lancet (2011) 378(9791):607–20. doi: 10.1016/S0140-6736(10)62307-0
3. Wang M, Peng B, Liu J, Yin X, Tan Z, Liu R, et al. Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: A retrospective multicenter analysis of 1029 patients. Ann Surg (2021) 273(1):145–53. doi: 10.1097/SLA.0000000000003190
4. Pratt WB, Maithel SK, Vanounou T, Huang ZS, Callery MP, Vollmer CM Jr. Clinical and economic validation of the international study group of pancreatic fistula (ISGPF) classification scheme. Ann Surg (2007) 245(3):443–51. doi: 10.1097/01.sla.0000251708.70219.d2
5. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg (2013) 216(1):1–14. doi: 10.1016/j.jamcollsurg.2012.09.002
6. Tang B, Lin Z, Ma Y, Zhang A, Liu W, Zhang J, et al. A modified alternative fistula risk score (a-FRS) obtained from the computed tomography enhancement pattern of the pancreatic parenchyma predicts pancreatic fistula after pancreatoduodenectomy. HPB (Oxford) (2021) 23(11):1759–66. doi: 10.1016/j.hpb.2021.04.015
7. Huttner FJ, Probst P, Knebel P, Strobel O, Hackert T, Ulrich A, et al. Meta-analysis of prophylactic abdominal drainage in pancreatic surgery. Br J Surg (2017) 104(6):660–8. doi: 10.1002/bjs.10505
8. Conlon KC, Labow D, Leung D, Smith A, Jarnagin W, Coit DG, et al. Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg (2001) 234(4):487–93. doi: 10.1097/00000658-200110000-00008
9. Liu X, Chen K, Chu X, Liu G, Yang Y, Tian X. Prophylactic intra-peritoneal drainage after pancreatic resection: An updated meta-analysis. Front Oncol (2021) 11:658829. doi: 10.3389/fonc.2021.658829
10. Lyu Y, Cheng Y, Wang B, Zhao S, Chen L. Peritoneal drainage or no drainage after pancreaticoduodenectomy and/or distal pancreatectomy: a meta-analysis and systematic review. Surg Endosc (2020) 34(11):4991–5005. doi: 10.1007/s00464-019-07293-w
11. McMillan MT, Fisher WE, Van Buren G 2nd, McElhany A, Bloomston M, Hughes SJ, et al. The value of drains as a fistula mitigation strategy for pancreatoduodenectomy: something for everyone? results of a randomized prospective multi-institutional study. J Gastrointest Surg (2015) 19(1):21–30. doi: 10.1007/s11605-014-2640-z
12. Van Buren G 2nd, Bloomston M, Schmidt CR, Behrman SW, Zyromski NJ, Ball CG, et al. A prospective randomized multicenter trial of distal pancreatectomy with and without routine intraperitoneal drainage. Ann Surg (2017) 266(3):421–31. doi: 10.1097/SLA.0000000000002375
13. Witzigmann H, Diener MK, Kienkotter S, Rossion I, Bruckner T, Barbel W, et al. No need for routine drainage after pancreatic head resection: The dual-center, randomized, controlled PANDRA trial (ISRCTN04937707). Ann Surg (2016) 264(3):528–37. doi: 10.1097/SLA.0000000000001859
14. Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, et al. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg (2014) 259(4):605–12. doi: 10.1097/SLA.0000000000000460
15. Bassi C, Molinari E, Malleo G, Crippa S, Butturini G, Salvia R, et al. Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg (2010) 252(2):207–14. doi: 10.1097/SLA.0b013e3181e61e88
16. Dai M, Liu Q, Xing C, Tian X, Cao F, Tang W, et al. Early drain removal is safe in patients with low or intermediate risk of pancreatic fistula after pancreaticoduodenectomy: A multicenter, randomized controlled trial. Ann Surg (2022) 275(2):e307–14. doi: 10.1097/SLA.0000000000004992
17. Dai MH, Liu QF, Xing C, Kleeff J, Liao Q, Guo JC, et al. Early drain removal after major pancreatectomy reduces postoperative complications: A prospective, randomized, single-center trial. J Pancreatol (2020) 3(2):93–100. doi: 10.1097/JP9.0000000000000049
18. Beane JD, House MG, Ceppa EP, Dolejs SC, Pitt HA. Variation in drain management after pancreatoduodenectomy: Early versus delayed removal. Ann Surg (2019) 269(4):718–24. doi: 10.1097/SLA.0000000000002570
19. Bolliger M, Kroehnert JA, Molineus F, Kandioler D, Schindl M, Riss P, et al. Experiences with the standardized classification of surgical complications (Clavien-dindo) in general surgery patients. Eur Surg (2018) 50(6):256–61. doi: 10.1007/s10353-018-0551-z
20. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the international study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery (2017) 161(3):584–91. doi: 10.1016/j.surg.2016.11.014
21. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the international study group of pancreatic surgery (ISGPS). Surgery (2007) 142(5):761–8. doi: 10.1016/j.surg.2007.05.005
22. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an international study group of pancreatic surgery (ISGPS) definition. Surgery (2007) 142(1):20–5. doi: 10.1016/j.surg.2007.02.001
Keywords: pancreaticoduodenectomy, early drain removal, postoperative pancreatic fistula, postoperative complications, pancreatic cancer
Citation: Xie X, Chen K, Liu Z, Wang F, Ma Y, Zhang S, Shao Z, Yang Y and Tian X (2022) Safety evaluation of early drain removal following pancreaticoduodenectomy: A single-center retrospective cohort study. Front. Oncol. 12:993901. doi: 10.3389/fonc.2022.993901
Received: 14 July 2022; Accepted: 15 September 2022;
Published: 29 September 2022.
Edited by:
John Gibbs, Hackensack Meridian Health, United StatesCopyright © 2022 Xie, Chen, Liu, Wang, Ma, Zhang, Shao, Yang and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yinmo Yang, YangyinmoSCI@bjmu.edu.cn; Xiaodong Tian, tianxiaodong@pkufh.com
†These authors have contributed equally to this work
 Xuehai Xie
Xuehai Xie Kai Chen
Kai Chen Zonghao Liu1
Zonghao Liu1 Xiaodong Tian
Xiaodong Tian