Abstract
Background
Idiopathic infantile hypercalcemia (IIH) etiologies include pathogenic variants in CYP24A1, leading to increased 1,25(OH)2 D, hypercalciuria and suppressed parathyroid hormone (PTH), and in SLC34A1 and SLC34A3, leading to the same metabolic profile via increased phosphaturia. IIH has not been previously described in CKD due to kidney hypodysplasia (KHD).
Methods
Retrospective study of children with bilateral KHD and simultaneously tested PTH and 1,25(OH)2D, followed in a tertiary care center between 2015 and 2021.
Results
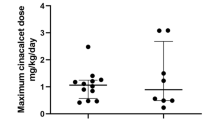
Of 295 screened patients, 139 had KHD, of them 16 (11.5%) had IIH (study group), 26 with normal PTH and any 1,25(OH)2D were controls. There were no differences between groups’ gender, obstructive uropathy rate and baseline eGFR. Study patients were younger [median (IQR) age: 5.2 (3.2–11.3) vs. 61 (13.9–158.3) months, p < 0.001], had higher 1,25(OH)2D (259.1 ± 91.7 vs. 156.5 ± 46.4 pmol/l, p < 0.001), total calcium (11.1 ± 0.4 vs. 10.7 ± 0.3 mg/dl, p < 0.001), and lower phosphate standard deviation score (P-SDS) [median (IQR): − 1.4 (− 1.9, − 0.4) vs. − 0.3 (− 0.8, − 0.1), p = 0.03]. During 12 months of follow-up, PTH increased among the study group (8.8 ± 2.8 to 22.7 ± 12.4 pg/ml, p < 0.001), calcium decreased (11 ± 0.5 to 10.3 ± 0.6 mg/dl, p = 0.004), 1,25(OH)2D decreased (259.5 ± 91.7 to 188.2 ± 42.6 pmol/l, p = 0.1), P-SDS increased [median (IQR): − 1.4 (− 1.9, − 0.4) vs. − 0.3 (− 0.9, 0.4), p = 0.04], while eGFR increased. Five of 9 study group patients with available urine calcium had hypercalciuria. Five patients had nephrocalcinosis/lithiasis. Genetic analysis for pathogenic variants in CYP24A1, SLC34A1 and SLC34A3 had not been performed.
Conclusions
Transient IIH was observed in infants with KHD, in association with hypophosphatemia, resembling SLC34A1 and SLC34A3 pathogenic variants’ metabolic profile.
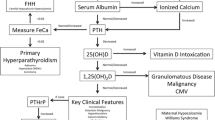
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
References
Woolf AS, Price KL, Scambler PJ, Winyard PJ (2004) Evolving concepts in human renal dysplasia. J Am Soc Nephrol 15:998–1007. https://doi.org/10.1097/01.asn.0000113778.06598.6f
Ichikawa I, Kuwayama F, Pope JC 4th, Stephens FD, Miyazaki Y (2002) Paradigm shift from classic anatomic theories to contemporary cell biological views of CAKUT. Kidney Int 61:889–898. https://doi.org/10.1046/j.1523-1755.2002.00188.x
Ekstrom T (1955) Renal hypoplasia; a clinical study of 179 cases. Acta Chir Scand 203:1–168
Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, Andress DL (2007) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71:31–38. https://doi.org/10.1038/sj.ki.5002009
Schmitt CP, Mehls O (2008) Disorders of bone mineral metabolism in chronic kidney disease. In: Geary D, Schaefer F (eds) Comprehensive Pediatric Nephrology. Mosby Elsevier, Philadelphia
Salusky IB, Goodman WG, Sahney S, Gales B, Perilloux A, Wang HJ, Elashoff RM, Jüppner H (2005) Sevelamer controls parathyroid hormone-induced bone disease as efficiently as calcium carbonate without increasing serum calcium levels during therapy with active vitamin D sterols. J Am Soc Nephrol 16:2501–2508. https://doi.org/10.1681/ASN.2004100885
Schlingmann KP, Kaufmann M, Weber S, Irwin A, Goos C, John U, Misselwitz J, Klaus G, Kuwertz-Bröking E, Fehrenbach H, Wingen AM, Güran T, Hoenderop JG, Bindels RJ, Prosser DE, Jones G, Konrad M (2011) Mutations in CYP24A1 and idiopathic infantile hypercalcemia. N Engl J Med 365:410–421. https://doi.org/10.1056/NEJMoa1103864
Schlingmann KP, Ruminska J, Kaufmann M, Dursun I, Patti M, Kranz B, Pronicka E, Ciara E, Akcay T, Bulus D, Cornelissen EA, Gawlik A, Sikora P, Patzer L, Galiano M, Boyadzhiev V, Dumic M, Vivante A, Kleta R, Dekel B, Levtchenko E, Bindels RJ, Rust S, Forster IC, Hernando N, Jones G, Wagner CA, Konrad M (2016) Autosomal-recessive mutations in SLC34A1 encoding sodium-phosphate cotransporter 2A cause idiopathic infantile hypercalcemia. J Am Soc Nephrol 27:604–614. https://doi.org/10.1681/ASN.2014101025
Nesterova G, Malicdan MC, Yasuda K, Sakaki T, Vilboux T, Ciccone C, Horst R, Huang Y, Golas G, Introne W, Huizing M, Adams D, Boerkoel CF, Collins MT, Gahl WA (2013) 1,25-(OH)2D–24 hydroxylase (CYP24A1) deficiency as a cause of nephrolithiasis. Clin J Am Soc Nephrol 8:649–657. https://doi.org/10.2215/CJN.05360512
De Paolis E, Scaglione GL, De Bonis M, Minucci A, Capoluongo E (2019) CYP24A1 and SLC34A1 genetic defects associated with idiopathic infantile hypercalcemia: from genotype to phenotype. Clin Chem Lab Med 57:1650–1667. https://doi.org/10.1515/cclm-2018-1208
Dinour D, Beckerman P, Ganon L, Tordjman K, Eisenstein Z, Holtzman EJ (2013) Loss-of-function mutations of CYP24A1, the vitamin D 24-hydroxylase gene, cause long-standing hypercalciuric nephrolithiasis and nephrocalcinosis. J Urol 190:552–557. https://doi.org/10.1016/j.juro.2013.02.3188
Meusburger E, Mündlein A, Zitt E, Obermayer-Pietsch B, Kotzot D, Lhotta K (2013) Erratum: Medullary nephrocalcinosis in an adult patient with idiopathic infantile hypercalcaemia and a novel CYP24A1 mutation. Clin Kidney J 6:453. https://doi.org/10.1093/ckj/sft091.Erratumfor:(2013)ClinKidneyJ6:211-215
Al Kalbani N, Frieling M, Teh JC, Harvey E, Geary DF (2011) Idiopathic hypercalcemia in infants with renal dysplasia. Clin Nephrol 75:466–471. https://doi.org/10.5414/cnp75466
Kodous N, Filler G, Sharma AP, Van Hooren TA (2015) PTHrP-related hypercalcaemia in infancy and congenital anomalies of the kidney and urinary tract (CAKUT). Can J Kidney Health Dis 11:21. https://doi.org/10.1186/s40697-015-0052-y
Feinstein S, Becker-Cohen R, Rinat C, Frishberg Y (2006) Hyperphosphatemia is prevalent among children with nephrotic syndrome and normal renal function. Pediatr Nephrol 21:1406–1412. https://doi.org/10.1007/s00467-006-0195-2
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Ishimura E, Nishizawa Y, Inaba M, Matsumoto N, Emoto M, Kawagishi T, Shoji S, Okuno S, Kim M, Miki T, Morii H (1999) Serum levels of 1,25-dihydroxyvitamin D, 24,25- dihydroxyvitamin D, and 25-hydroxyvitamin D in nondialyzed patients with chronic renal failure. Kidney Int 55:1019–1027. https://doi.org/10.1046/j.1523-1755.1999.0550031019.x
Petkovich M, Jones G (2011) CYP24A1 and kidney disease. Curr Opin Nephrol Hypertens 20:337–344. https://doi.org/10.1097/MNH.0b013e3283477a7b
Lightwood R, Stapleton T (1953) Idiopathic hypercalcaemia in infants. Lancet 265:255–256. https://doi.org/10.1016/s0140-6736(53)90187-1
Rhaney K, Mitchell RG (1956) Idiopathic hypercalcaemia of infants. Lancet 270:1028–1032. https://doi.org/10.1016/s0140-6736(56)90798-x
Janiec A, Halat-Wolska P, Obrycki Ł, Ciara E, Wójcik M, Płudowski P, Wierzbicka A, Kowalska E, Książyk JB, Kułaga Z, Pronicka E, Litwin M (2021) Long-term outcome of the survivors of infantile hypercalcaemia with CYP24A1 and SLC34A1 mutations. Nephrol Dial Transplant 36:1484–1492. https://doi.org/10.1093/ndt/gfaa178
Huang J, Coman D, McTaggart SJ, Burke JR (2006) Long-term follow-up of patients with idiopathic infantile hypercalcaemia. Pediatr Nephrol 21:1676–1680. https://doi.org/10.1007/s00467-006-0217-0
Gurevich E, Levi S, Borovitz Y, Alfandary H, Ganon L, Dinour D, Davidovits M (2021) Childhood hypercalciuric hypercalcemia with elevated vitamin D and suppressed parathyroid hormone: long-term follow up. Front Pediatr 9:752312. https://doi.org/10.3389/fped.2021.752312
Kovacs CS (2014) Bone development and mineral homeostasis in the fetus and neonate: roles of the calciotropic and phosphotropic hormones. Physiol Rev 94:1143–1218. https://doi.org/10.1152/physrev.00014.2014
Northrop G, Misenhimer HR, Becker FO (1977) Failure of parathyroid hormone to cross the nonhuman primate placenta. Am J Obstet Gynecol 129:449–453. https://doi.org/10.1016/0002-9378(77)90593-2
Rigo J, Pieltain C, Viellevoye R, Bagnoli F (2018) Calcium and phosphorus homeostasis: pathophysiology. In: Buonocore G, Bracci R, Weindling M (eds) Neonatology. Springer, Cham
Mayne PD, Kovar IZ (1991) Calcium and phosphorus metabolism in the premature infant. Ann Clin Biochem 28(Pt 2):131–142. https://doi.org/10.1177/000456329102800203
Lichtenstein P, Specker BL, Tsang RC, Mimouni F, Gormley C (1986) Calcium-regulating hormones and minerals from birth to 18 months of age: a cross-sectional study. I. Effects of sex, race, age, season, and diet on vitamin D status. Pediatrics 77:883–890
Stein DR, Feldman HA, Gordon CM (2012) Vitamin D status in children with chronic kidney disease. Pediatr Nephrol 27:1341–1350. https://doi.org/10.1007/s00467-012-2143-7
Pulskens WP, Verkaik M, Sheedfar F, van Loon EP, van de Sluis B, Vervloet MG, Hoenderop JG, Bindels RJ, NIGRAM Consortium (2015) Deregulated renal calcium and phosphate transport during experimental kidney failure. PLoS One 10:e0142510. https://doi.org/10.1371/journal.pone.0142510
Acknowledgements
We thank Uri Alon, MD, for his critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gurevich, E., Borovitz, Y., Levi, S. et al. Idiopathic infantile hypercalcemia in children with chronic kidney disease due to kidney hypodysplasia. Pediatr Nephrol 38, 1067–1073 (2023). https://doi.org/10.1007/s00467-022-05740-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05740-w