Abstract
Purpose
This study aims to assess whether computer navigation can improve the accuracy of the trough position and clinical outcomes of expansive open-door cervical laminoplasty (EOLP).
Methods
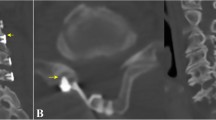
We reviewed a single centre of 28 conventional EOLP and 24 computer navigation EOLP cases. The conventional group had 102 laminae while the navigation group had 88. The distance from the medial cortex to the pedicle on the open-door side (OD) and hinge side (HD) was measured. Furthermore, the area of the spinal canal corresponding to each lamina before and after the surgical procedure was also measured. We then compared the differences in radiographic parameters and clinical outcomes between the two groups.
Results
OD and HD were smaller in the navigation group compared to the conventional group, and the enlarged area of the spinal canal was larger in the navigation group than in the conventional group. The Japanese Orthopaedic Association (JOA) scores one year after the surgical procedure improved in both groups compared to the pre-operative period, and the JOA recovery rate was higher in the navigation group. The incidence of hinge fracture was lower in the navigation group, and the incidence of C5 palsy and axial pain was not statistically different between the two groups.
Conclusion
The use of computer navigation techniques has the potential to significantly improve the accuracy of EOLP compared to conventional procedures. It has been shown to more fully expand the spinal canal and contribute to clinical efficacy.




Similar content being viewed by others
References
Ogawa Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Hirabayashi H, Hirabayashi K, Nishiwaki Y, Toyama Y (2005) Long-term results after expansive open-door laminoplasty for the segmental-type of ossification of the posterior longitudinal ligament of the cervical spine: a comparison with nonsegmental-type lesions. J Neurosurg Spine 3:198–204. https://doi.org/10.3171/spi.2005.3.3.0198
Wang LN, Wang L, Song YM, Yang X, Liu LM, Li T (2016) Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. Int Orthop 40:1267–1274. https://doi.org/10.1007/s00264-016-3194-3
Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, Matsumoto M, Toyama Y (2006) Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine 31:2998–3005. https://doi.org/10.1097/01.brs.0000250307.78987.6b
Yeh KT, Lee RP, Chen IH, Yu TC, Liu KL, Peng CH, Wang JH, Wu WT (2015) Laminoplasty instead of laminectomy as a decompression method in posterior instrumented fusion for degenerative cervical kyphosis with stenosis. J Orthop Surg Res 10:138. https://doi.org/10.1186/s13018-015-0280-y
Hur JW, Park YK, Kim BJ, Moon HJ, Kim JH (2016) Risk factors for delayed hinge fracture after plate-augmented cervical open-door laminoplasty. J Korean Neurosurg Soc 59:368–373. https://doi.org/10.3340/jkns.2016.59.4.368
Uematsu Y, Tokuhashi Y, Matsuzaki H (1998) Radiculopathy after laminoplasty of the cervical spine. Spine 23:2057–2062. https://doi.org/10.1097/00007632-199810010-00004
Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES, Baethis H (2010) Image-guided spine surgery: state of the art and future directions. Eur Spine J 19:25–45. https://doi.org/10.1007/s00586-009-1091-9
Lange N, Meyer B, Meyer HS (2021) Navigation for surgical treatment of disorders of the cervical spine – a systematic review. J Orthop Surg 29:23094990211012864. https://doi.org/10.1177/23094990211012865
Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Sautot P (1998) Pedicle screw placement using image guided techniques. Clin Orthop Relat Res:39–48. https://doi.org/10.1097/00003086-199809000-00006
Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K (1999) Accurate pedicle screw insertion under the control of a computer-assisted image guiding system: laboratory test and clinical study. J Orthop Sci 4:197–206. https://doi.org/10.1007/s007760050094
Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K (2000) Cervical pedicle screw insertion: assessment of safety and accuracy with computer-assisted image guidance. J Spinal Disord 13:218–224. https://doi.org/10.1097/00002517-200006000-00004
Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 99:257–263. https://doi.org/10.3171/spi.2003.99.3.0257
Moore T, McLain RF (2005) Image-guided surgery in resection of benign cervicothoracic spinal tumors: a report of two cases. Spine J 5:109–114. https://doi.org/10.1016/j.spinee.2004.06.020
Smith HE, Vaccaro AR, Yuan PS, Papadopoulos S, Sasso R (2006) The use of computerized image guidance in lumbar disk arthroplasty. J Spinal Disord Tech 19:22–27. https://doi.org/10.1097/01.bsd.0000187977.76926.85
Seichi A, Takeshita K, Kawaguchi H, Kawamura N, Higashikawa A, Nakamura K (2005) Image-guided surgery for thoracic ossification of the posterior longitudinal ligament. Technical note. J Neurosurg Spine 3:165–168. https://doi.org/10.3171/spi.2005.3.2.0165
Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y (1983) Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 8:693–699. https://doi.org/10.1097/00007632-198310000-00003
Sun Y, Li L, Zhao J, Gu R (2015) Comparison between anterior approaches and posterior approaches for the treatment of multilevel cervical spondylotic myelopathy: a meta-analysis. Clin Neurol Neurosurg 134:28–36. https://doi.org/10.1016/j.clineuro.2015.04.011
Lee JH, Chough CK (2018) Risk factors for hinge fracture associated with surgery following cervical open-door laminoplasty. Korean J Neurotrauma 14:118–122. https://doi.org/10.13004/kjnt.2018.14.2.118
Xia Y, Xia Y, Shen Q, Li H, Xu T (2011) Influence of hinge position on the effectiveness of expansive open-door laminoplasty for cervical spondylotic myelopathy. J Spinal Disord Tech 24:514–520. https://doi.org/10.1097/BSD.0b013e3182064632
Zhang X, Zhang Y, Duan D, Xie H (2018) A novel drill navigation template combines preoperative simulation in expansive open-door laminoplasty. World Neurosurg 118:e758–e765. https://doi.org/10.1016/j.wneu.2018.07.041
Park AE, Heller JG (2004) Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion—surgical technique. J Spinal Disord Tech 17:265–271. https://doi.org/10.1097/01.bsd.0000095401.27687.c0
Hosono N, Yonenobu K, Ono K (1996) Neck and shoulder pain after laminoplasty A noticeable complication. Spine 21:1969–1973. https://doi.org/10.1097/00007632-199609010-00005
Chen H, Liu H, Zou L, Li T, Gong Q, Song Y, Zeng J, Liu L, Kong Q (2016) Effect of mini-plate fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty. Clin Spine Surg 29:E288-295. https://doi.org/10.1097/bsd.0000000000000131
Hirabayashi K, Satomi K (1988) Operative procedure and results of expansive open-door laminoplasty. Spine 13:870–876. https://doi.org/10.1097/00007632-198807000-00032
Okada M, Minamide A, Endo T, Yoshida M, Kawakami M, Ando M, Hashizume H, Nakagawa Y, Maio K (2009) A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Spine 34:1119–1126. https://doi.org/10.1097/BRS.0b013e31819c3b61
Kong Q, Zhang L, Liu L, Li T, Gong Q, Zeng J, Song Y, Liu H, Wang S, Sun Y, Zhang F, Li M, Chen Z (2011) Effect of the decompressive extent on the magnitude of the spinal cord shift after expansive open-door laminoplasty. Spine 36:1030–1036. https://doi.org/10.1097/BRS.0b013e3181e80507
Imagama S, Matsuyama Y, Yukawa Y, Kawakami N, Kamiya M, Kanemura T, Ishiguro N (2010) C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br 92:393–400. https://doi.org/10.1302/0301-620x.92b3.22786
Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Hirabayashi K (2002) Segmental motor paralysis after expansive open-door laminoplasty. Spine 27:2108–2115. https://doi.org/10.1097/00007632-200210010-00006
Acknowledgements
We would like to thank Dr. Kai Zhang from Shanghai Ninth People’s Hospital for helpful discussion.
Funding
This work was supported by the Natural Science Foundation of Fujian Province, China (Grant No. 2021J05073).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by JT, YL, WZ, and YX. The first draft of the manuscript was written by JT, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Fujian Provincial Hospital.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tian, J., Lin, Y., Zheng, W. et al. Accuracy of the trough position in expansive open-door cervical laminoplasty using computer navigation techniques: a single-centre retrospective study. International Orthopaedics (SICOT) 46, 2907–2912 (2022). https://doi.org/10.1007/s00264-022-05585-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05585-w