Abstract
Herpes simplex virus (HSV) infection induces a rapid and transient increase in intracellular calcium concentration ([Ca2+]i), which plays a critical role in facilitating viral entry. T-type calcium channel blockers and EGTA, a chelate of extracellular Ca2+, suppress HSV-2 infection. But the cellular mechanisms mediating HSV infection-activated Ca2+ signaling have not been completely defined. In this study we investigated whether the TRPV4 channel was involved in HSV-2 infection in human vaginal epithelial cells. We showed that the TRPV4 channel was expressed in human vaginal epithelial cells (VK2/E6E7). Using distinct pharmacological tools, we demonstrated that activation of the TRPV4 channel induced Ca2+ influx, and the TRPV4 channel worked as a Ca2+-permeable channel in VK2/E6E7 cells. We detected a direct interaction between the TRPV4 channel protein and HSV-2 glycoprotein D in the plasma membrane of VK2/E6E7 cells and the vaginal tissues of HSV-2–infected mice as well as in phallic biopsies from genital herpes patients. Pretreatment with specific TRPV4 channel inhibitors, GSK2193874 (1−4 μM) and HC067047 (100 nM), or gene silence of the TRPV4 channel not only suppressed HSV-2 infectivity but also reduced HSV-2-induced cytokine and chemokine generation in VK2/E6E7 cells by blocking Ca2+ influx through TRPV4 channel. These results reveal that the TRPV4 channel works as a Ca2+-permeable channel to facilitate HSV-2 infection in host epithelial cells and suggest that the design and development of novel TRPV4 channel inhibitors may help to treat HSV-2 infections.
Similar content being viewed by others
Introduction
Herpes simplex virus (HSV) infection induces a rapid and transient increase in the intracellular calcium concentration ([Ca2+]i), which plays a critical role in facilitating viral entry [1]. Studies have shown that the interaction between HSV-2 glycoprotein H and integrin alpha V beta 3 promotes the release of intracellular calcium stores and contributes to viral entry into human cervical and primary genital tract epithelial cells [2]. Additionally, HSV-1 glycoprotein D binds the TRPC1 channel to elicit intracellular Ca2+ release [1]. Deletion of glycoprotein D from HSV-1 does not induce an [Ca2+]i response [3, 4]. Moreover, T-type calcium channel blockers and EGTA [Ethylene-bis (oxyethylenenitrilo) tetraacetic acid], a chelate of extracellular Ca2+, suppress HSV-2 infection [5].
The transient receptor potential vanilloid (TRPV) channel family is part of the transient receptor potential (TRP) superfamily, which includes TRPV1-6 [6]. Among them, the TRPV1 and TRPV4 channels are thermosensitive, share 40%–50% sequence identity, are widely expressed and control various physiological functions [6, 7]. Accumulating evidence indicates that the function of the TRPV1 channel is closely related to several viral infections. TRPV1 channel activation triggers Ca2+ influx that regulates coxsackievirus B [8], HSV-1 [9], Chikungunya virus [10], human rhinovirus [11] and respiratory syncytial virus infections [12,13,14]. Glycoprotein G, secreted by HSV-2, mediates the localization and activation of the TRPV1 channel to alter thermal pain sensitivity in the dermis [15]. However, little is known about the relationship between HSV-2 infection and the TRPV4 channel. In this study, we investigated the involvement of the TRPV4 channel in HSV-2 infection using human epithelial cells, mouse models, and phallic biopsies from HSV-2-infected patients.
We found that the TRPV4 channel is a Ca2+-permeable channel in host epithelial cells. During HSV-2 infection, viral glycoprotein D binds to the TRPV4 channel and induces an increase in intracellular calcium concentration. Blocking TRPV4 channels exerts antiviral and anti-inflammatory effects via suppression of Ca2+ oscillations. These findings reveal a previously unidentified role of the TRPV4 channel in HSV-2 infection.
Materials and methods
Cells, viruses, and animals
The human vaginal epithelial cell line VK2/E6E7 (ATCC® CRL-2616TM) was cultured in keratinocyte serum-free medium supplemented with 50 μg/mL bovine pituitary extract, 0.1 ng/ml recombinant epidermal growth factor (rEGF), 100 μg/ml streptomycin, 100 units/ml penicillin, and 0.4 mM CaCl2. Vero cells, CHO cells, and human HaCaT keratinocytes were cultured in DMEM supplemented with glucose (Gobio, USA), 10% fetal bovine serum (Gibco, Life Technologies), and 1% gentamicin (Sigma).
The HSV-2 strain 333 was provided by the Guangzhou Institute of Biomedicine and Health (Guangzhou, China). Female BALB/c mice at the age of five to seven weeks were purchased from Guangdong Medical Laboratory Animals Center in Guangzhou, China. The animals were provided with ad libitum access to food and water in a room maintained at a constant temperature of 24 ± 0.5 °C with a 12:12 h light/dark photoperiod.
Reagents and solutions
GSK1016790A (HY-19608), GSK2193874 (HY-100720), HC067047 (883031-03-6), thapsigargin (HY-13433), ionomycin (56092-82-1), and forskolin (66575-29-9) were purchased from MedChemExpress (MCE). Fluo-3 AM (ab145254) and antibodies against HSV-2 gD were purchased from Abcam. p-NF-κB-p65, IκBα, β-actin, and GAPDH were purchased from Cell Signaling Technology. HRP-conjugated secondary antibodies were obtained from Sigma Aldrich. A normal physiological saline solution (NPSS) was created containing 137 mM NaCl, 5 mM KCl, 1 mM MgCl2, 2.5 mM CaCl2, 10 mM Herpes, and 10 mM glucose; this solution had a pH of 7.4. A Ca2+-free physiological saline solution (Ca2+-free PSS) with a pH of 7.4 was prepared by omitting Ca2+ and adding 2 mM EGTA to the NPSS.
Measurement of intracellular calcium in uninfected cells
The human vaginal epithelial cell lines VK2/E6E7 were seeded on coverslips. Cells were washed with normal physiological saline solution and then incubated with Fluo-3 acetoxymethyl ester (10 μM) at room temperature for 45 min. Then, the coverslips were transferred to a special circular groove of the laser confocal fluorescence microscope. Drugs were added to the coverslips in the circular groove. The fluorescence signal was recorded by a laser scanning confocal imaging system (TCS SP2, Leica Microsystems, Mannheim, Germany) at a 488-nm excitation wavelength and a 520 nm absorption wavelength [1]. The data were further analyzed with Origin 8.0.
Quantitative PCR
Total RNA was extracted using TRIzol (Invitrogen, USA). RNA concentrations were measured using a NanoDrop 2000c (Thermo Scientific). cDNA was reverse transcribed using a PrimeScript™ RT Reagent Kit (Takara). Quantitative PCR was performed with ChamQ SYBR qPCR Master Mix (Vazyme, China) on a LightCycler 480 System (Roche, Switzerland).
The primers used in the quantitative PCR are listed in Table 1. The levels of the target genes were normalized to the levels of GAPDH mRNA, and relative expression was determined according to the ΔΔCt method [16].
Western blot
Total protein from epithelial cells or vaginal tissue was extracted with precooled RIPA buffer (Bio-Rad, CA, USA). The protein concentration was detected by a BCA protein kit. After separation with SDS-polyacrylamide gel electrophoresis (SDS‒PAGE), the protein samples were transferred to polyvinylidene fluoride membranes (Millipore, MA, USA). The membranes were blocked with 5% fat-free milk for one hour at room temperature, incubated with primary antibodies overnight at 4 °C, and incubated with secondary antibodies for one hour at room temperature. SuperSignal ECL reagent (Millipore, MA, USA) was used to observe the chemiluminescence signals using a multifunctional imaging system (ProteinSimple, CA, USA) [17].
Immunofluorescence
Immunofluorescent staining was performed as previously described [5]. The infected cells, vaginal tissues, and phallic biopsies were fixed with acetone at 4 °C for 10 min.
After washing with phosphate-buffered saline (PBS) and treating with 1% BSA for 30 min at room temperature, the samples were incubated with the first primary antibody at 4 °C overnight, followed by the secondary antibody, goat anti-mouse IgG conjugated to fluorescein isothiocyanate (FITC) or Texas red (Santa Cruz Biotechnology), at room temperature for one hour. VECTA-SHIELD medium (Vector Labs., Burlingame, CA, USA) was used to preserve the samples. Finally, images were captured via a fluorescence microscope (TE2000U, Tecan, USA).
Virus infection
VK2/E6E7 cells were inoculated in 6-well plates at a density of 1 × 106 cells per well. The next day, HSV-2 (MOI = 5) was administered to the cells in the presence or absence of drugs for 1 h. Subsequently, the unabsorbed virus was removed, and keratinocyte serum-free medium containing drugs was added [5]. The cells were collected at the specified time points for quantitative PCR and Western blotting. The culture supernatants were collected for plaque assays.
Plaque assay
The generation of progeny viruses was evaluated by the plaque assay [5]. Vero cells were inoculated in 12-well plates at a density of 1.2 × 105 cells per well. Diluted culture supernatants of infected cells were added to the Vero cells. After incubation for 1 h at 37 °C, the culture supernatants were discarded, and DMEM containing 2% fetal bovine serum and 1% methylcellulose was added. After incubation in this solution for 3, 4 days at 37 °C, crystal violet was used to stain the cells. The yield of progeny viruses in the supernatant was determined by calculating the number of plaques.
Measurement of intracellular Ca2+ concentrations in infected cells
The intracellular Ca2+ concentrations of infected cells were measured with BB-cell probe F03 (BB-48112, BestBio, China) [18]. Briefly, cells were inoculated in 12-well plates at a density of 1.5 × 105 cells per well. After infection with HSV-2 (MOI = 5), the cells were washed three times with Hanks’ balanced salt solution (HBSS) at the specified time points. The diluted F03 probe was loaded and incubated for 1 h at 37 °C. After three washes, the cells were incubated for another 40 min. The fluorescence values were detected with a fluorescence microplate reader. Data are expressed as fluorescence units.
Mouse model of vaginal HSV-2 infection
All animal experiments were conducted following protocols approved by the Animal Use and Care Committee of Southern Medical University. The vaginal cavity of mice was washed with PBS and rubbed with sterile cotton to increase mouse susceptibility to vaginal HSV-2 infection. The mice were then inoculated vaginally with 1 × 106 PFU HSV-2. After seven days, the phenotypes of the infected mice were scored as follows [19]: “1”, slight genital erythema and edema; “2”, moderate genital inflammation; “3”, severe exudative genital lesions; “4”, hind limb paralysis; or “5”, death. Vaginal tissues were collected for immunofluorescent analysis or immunoprecipitation.
Immunoprecipitation
The interaction between the TRPV4 channels and HSV-2 glycoprotein D was investigated by immunoprecipitation [1]. Epithelial cells were infected with HSV-2 (MOI = 5) for one hour. After the cells were washed with precooled PBS, IP lysis buffer (Beyotime, Shanghai, China) was added for 30 min on ice. Next, the lysates of infected cells or vaginal tissues were centrifuged at 12,000 rpm for 15 min at 4 °C. The 10% supernatant was removed for use as the input group. The other lysates were mixed with protein A/G beads (GE Healthcare, Sweden) and incubated overnight with anti-TRPV4 antibody at 4 °C. After the lysates were washed with precooled IP buffer, an appropriate amount of the solution was analyzed by Western blot.
Statistical analysis
Experimental data are expressed as the means ± SEMs. The Students’ two-tailed t-tests were used for two sets of data analysis. Three or more groups were analyzed with one-way ANOVAs followed by Dunnett’s post hoc test using GraphPad Prism 8.0 software (*P < 0.05, **P < 0.01, ***P < 0.001). Two-tailed P values < 0.05 were considered statistically significant.
Results
The TRPV4 channel is expressed in HSV-2-infected epithelial cells
The TRPV channel family has six members, namely, TRPV1 through TRPV6 [20]. The expression of TRPV channels was measured by real-time quantitative PCR. The results showed that mRNA from the TRPV1, TRPV3, and TRPV4 channels was present in human vaginal epithelial cells (VK2/E6E7), as shown in Fig. 1a. The expression of the TRPV4 channel was detected by Western blot in human HaCaT keratinocytes (Fig. 1b) and was further confirmed by immunofluorescent staining. Intense immunofluorescence from the TRPV4 channel (green) was observed in the plasma membrane (Fig. 1c). These results demonstrate the presence of the TRPV4 channel in HSV-2 host epithelium cells.
a mRNA expression of TRPV1-6 in the human vaginal epithelial cell line VK2/E6E7 was measured with quantitative PCR. b TPRV4 channel expression in human HaCaT keratinocytes was detected by Western blot. c The localization of the TRPV4 channel (green) was observed by immunofluorescent staining in VK2/E6E7 cells. Upper scale bar: 10 μm; lower scale bar: 20 μm.
The TRPV4 channel is a Ca2+-permeable channel in host epithelial cells
To assess the function of the TRPV4 channel in epithelial cells, we observed the dynamic changes in intracellular Ca2+ with confocal microscopy. The classic activator of the TRPV4 channel, GSK1016790A (GSK, 1 μM), induced a significant increase in [Ca2+]i in epithelial cells in normal physiological saline solution (NPSS), as seen in Fig. 2a. Interestingly, GSK did not evoke this [Ca2+]i increase in Ca2+-free solution, as seen in Fig. 2b. Thapsigargin (Tg, 1 μM) induces the release of intracellular endoplasmic reticulum (ER) Ca2+ stores and prevents refilling by inhibiting ER Ca2+-ATPase. However, thapsigargin pretreatment did not eliminate the GSK-induced Ca2+ influx (Fig. 2c), indicating that activation of the TRPV4 channel causes Ca2+ influx. In addition, the GSK-induced Ca2+ influx was eliminated by pretreating cells with ruthenium red (RUR, a nonspecific TRPV4-channel inhibitor) or HC067047 (a specific TRPV4-channel inhibitor) [21], as shown in Fig. 2d, e. These data suggest that the TRPV4 channel is a Ca2+-permeable channel in host epithelial cells. Each experiment was independently repeated three times, and the data from 30 cells were selected for statistical analysis, as shown in Fig. 2f.
a GSK1016790A (GSK, 1 μM), a specific TRPV4 channel activator, significantly increased the intracellular Ca2+ concentration in normal physiological saline solution (NPSS). b GSK1016790A (GSK, 1 μM) did not increase the intracellular Ca2+ concentration in Ca2+-free solution (Ca2+-free-PSS). Thapsigargin (Tg, 1 μM) was used to indicate cell survival. c Thapsigargin (Tg, 1 μM), which induces the release of Ca2+ stores in the endoplasmic reticulum (ER) and prevents refilling by inhibiting the ER Ca2+-ATPase, had no noticeable effect on the elevation of intracellular Ca2+ induced by GSK in NPSS. Ionomycin (Iono, 5 μM) was used to indicate cell survival. d, e Ruthenium red (RUR, 100 nM, a nonspecific TRPV4 inhibitor) or HC067047 (HC067, 100 nM, a specific TRPV4 inhibitor) obviously hindered GSK-induced elevation of intracellular Ca2+. f The inhibitory effects of different conditions on the GSK-induced Ca2+ influx are summarized. Data are represented as the mean ± SD (**P < 0.01, compared with controls) and are from three independent experiments consisting of 30 cells each.
The TRPV4 channel interacts with HSV-2 glycoprotein D
During the early stages of viral entry, HSV glycoprotein D interacts with multiple cell surface receptors, including HVEM [22, 23], nectin-1 [24], and nectin-2 [25]. HSV-1 glycoprotein D also directly interacts with the TRPC1 channel, another member of the TRP superfamily [1]. This study aimed to examine whether HSV-2 glycoprotein D interacts with the TRPV4 channel. In coimmunoprecipitation, the TRPV4 channel and HSV-2 glycoprotein D were detected in the infected epithelial cells, as shown in Fig. 3a (left), but other viral glycoproteins, such as glycoprotein B, were not found, as shown in Fig. 3a (middle). To further explore the interaction of the TRPV4 channel and glycoprotein D under pathological conditions, we established a WT mouse model of vaginal infection using HSV-2 strain 333. Consistent with the results in infected cells, coimmunoprecipitation of the TRPV4 channel and glycoprotein D was observed in infected mice, as shown in Fig. 3a (right). These data suggest that the TRPV4 protein directly interacts with HSV-2 glycoprotein D.
a The human vaginal epithelial cell line VK2/E6E7 was infected with HSV-2 (MOI = 5). After 24 h of incubation, the cells were collected for immunoprecipitation to evaluate the interaction between the TRPV4 channel and glycoprotein D (left) or glycoprotein B (middle). Vaginal tissues collected from infected mice underwent immunoprecipitation to observe the TRPV4-gD interaction (right). b After transfection with the TRPV4 channel, CHO cells were infected with HSV-2 (MOI = 5) for 24 h and then collected for immunofluorescence staining to determine TRPV4-glycoprotein D colocalization. In the Pearson correlation analysis, Image J calculated r = 0.78 ± 0.09. Dil indicates the plasma membrane in red, the TRPV4 protein in blue and the HSV-2 glycoprotein D in green. “a” represents CHO cells successfully transfected with the TRPV4 channel; “b” represents CHO cells not successfully transfected with the TRPV4 channel. c A WT-mouse model of vaginal infection was established using HSV-2 strain 333; mouse vaginal tissues were collected for immunofluorescent staining. Here, red represents the TRPV4 protein, and green represents HSV-2 glycoprotein D. d The phallic biopsies from genital herpes patients were fixed and labeled with immunofluorescent staining, in which red indicates the TRPV4 protein and green indicates HSV-2 glycoprotein D.
To evaluate the colocalization of the TRPV4 protein and glycoprotein D, we transfected CHO cells lacking nectin-1 (a glycoprotein D receptor [26]) with the TRPV4 channel. The overlap of the fluorescence signal between the TRPV4 channel (blue) and glycoprotein D (green) was observed in the TRPV4-transfected cells, as shown in Fig. 3b. The CHO cells that were successfully transfected with the TRPV4 channel are indicated with “a”; those not successfully transfected with the TRPV4 channel are indicated with “b”. The data show that “a” exhibit greater glycoprotein D fluorescence than “b” in the plasma membrane. Image J was used to perform Pearson correlation analysis on fifty images; r was calculated as 0.78 ± 0.09, indicating that the green fluorescence of glycoprotein D and the blue fluorescence of the TRPV4 channel had high colocalization.
To further examine the colocalization of TRPV4 and glycoprotein D under pathological conditions, vaginal tissues from infected mice and phallic biopsies from genital herpes patients were collected for immunofluorescence assays. The fluorescence analysis indicated colocalization of the TRPV4 channel (red) and glycoprotein D (green) in the vaginal tissues of infected mice, as shown in Fig. 3c. Genital herpes and vaginitis are common symptoms of HSV-2 infection among humans [27]. Thus, some phallic biopsies from patients were selected for detection, and the same colocalization pattern of glycoprotein D and the TRPV4 channel was observed, as shown in Fig. 3d. These findings confirm that the TRPV4 channel and glycoprotein D colocalize in the plasma membrane of HSV-2-infected cells.
Blocking TRPV4 activity produces an anti-HSV-2 effect
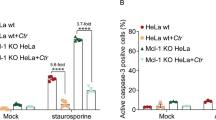
The Ca2+ influx mediated by the TRPV4 channel controls RNA virus infectivity [28]. Here, we explored the possibility that Ca2+ influx through TRPV4 channels contributes to infection of HSV-2, a DNA virus. The specific TRPV4-channel inhibitors GSK2193874 and HC067047 markedly decreased the Ca2+ oscillations induced by HSV-2 infection (Fig. 4a; left). A reduction in Ca2+ oscillations was also observed in the cells with siRNA knockdown of the TRPV4 channel (Fig. 4a; right). The data show that the increase in the intracellular calcium concentration triggered by HSV-2 infection is partly dependent on the TRPV4 channel.
a Effects of TRPV4 channel inhibitors and siRNA on HSV-2-induced Ca2+ oscillations in epithelial cells. The cells were infected with HSV-2 (MOI = 5) in the presence or absence of the specific TRPV4-channel inhibitors HC067047 (HC067, 100 nM) and GSK2193874 (GSK219, 4 μM). The cells were collected at the time specified by the calcium determination kit, and the changes in Ca2+ oscillations are shown in the left image. After transfection with siRNA, the cells infected with HSV-2 (MOI = 5) were collected at the time specified by the kit. The changes in Ca2+ oscillations are shown in the right image. b Effects of TRPV4 channel inhibitors on viral protein expression. The cells were infected with HSV-2 (MOI = 5) in the presence of the indicated concentrations of GSK2193874, HC067047 (100 nM), EGTA (an extracellular calcium chelating agent; 3.6 mM), or acyclovir (ACV; 1 μg/ml) separately for 24 h. The cells were collected to analyze viral glycoprotein D expression by Western blot. c The supernatant was harvested for virus titration by plaque assay. d The expression of the viral genes glycoprotein D and VP16 was measured by real-time quantitative PCR. Acyclovir, the typical drug used to treat HSV infection, served as the positive control. Data represent the mean ± SD of three independent experiments. **P < 0.01 vs. the control.
To determine the antiviral effect of specific TRPV4-channel inhibitors, we evaluated their effect on HSV-2 infection in host epithelial cells. The results showed that GSK2193874 and HC067047 visibly suppressed the synthesis of viral glycoprotein D (Fig. 4b), the production of progeny viruses (Fig. 4c), and the transcription of viral genes (VP16 and gD) (Fig. 4d). Acyclovir, the typical drug used to treat HSV infections, served as the positive control [29]. EGTA, which depleted extracellular Ca2+, as seen in Fig. 4b-d, had similar antiviral effects, indicating that the anti-HSV-2 effect of blocking the TRPV4 channel is closely related to Ca2+ oscillations. Further investigation showed that siRNA knockdown of the TRPV4 channel also inhibited viral gene transcription (Fig. 5b) and progeny virus production (Fig. 5c). These results suggest that blocking the TRPV4 channel inhibits HSV-2 infection by reducing the Ca2+ influx.
a Western blot analysis of TRPV4 channel expression in human epithelial cells transfected with siRNA against the TRPV4 channel. b The transfected cells were infected with HSV-2 (MOI = 5) for 24 h and collected for viral gene (glycoprotein D and VP16) expression analysis by real-time quantitative PCR. c The supernatant was harvested for virus titration by plaque assay. Data represent the mean ± SD of three independent experiments. **P < 0.01 vs. the control.
Blocking TRPV4 activity alleviates HSV-2-induced inflammation
Previous studies have shown that Ca2+ influx through TRPV4 channels creates a long-lasting inflammatory signal, and TLR-mediated inflammation is suppressed by blocking the TRPV4 channel [30]. Various pattern recognition receptors, such as TLR2, TLR9, and cGAS, can identify HSV-2 and then promote proinflammatory cytokine generation [31, 32]. To explore the relationship between the TRPV4 channel, a Ca2+-permeable channel, and the inflammatory signals in epithelial cells induced by HSV-2 infection, we investigated the anti-inflammatory effect of TRPV4-channel inhibitors in the infected cells. The specific TPRV4-channel inhibitor HC067047 (100 nM) reduced the HSV-2-induced expression of cytokines (TNF-α and IL-6) and chemokines (CXCL-9 and CXCL-10) at three specific time points, as shown in Fig. 6a. Three different concentrations of GSK2193874, another specific TPRV4-channel inhibitor, effectively decreased the expression of TNF-α, IL-6, CXCL-9, and CXCL-10 at 24 h, as shown in Fig. 6b. After transfection with siRNA against the TRPV4 channel, the inflammatory signals in infected cells markedly declined, as shown in Fig. 6c. These data indicate that the inflammatory signals induced by HSV-2 infection are closely tied to TRPV4 channel activity in epithelial cells.
a Human epithelial cells were infected with HSV-2 (MOI = 5) in the presence or absence of HC067047 (100 nM) and then harvested at 2, 4, or 6 h to analyze the expression of cytokines (TNF-α, IL-6) and chemokines (CXCL-9 and CXCL-10) by real-time quantitative PCR. b The infected cells were treated with the indicated concentrations of GSK2193874 for 24 h and then collected for cytokine and chemokine expression analysis. c The transfected cells were infected with HSV-2 (MOI = 5) for 24 h and then digested for cytokine and chemokine expression analysis by real-time quantitative PCR. d The cells were infected with HSV-2 (MOI = 5) in the presence or absence of HC067047, EGTA, or acyclovir (ACV, 1 μg/ml) for 24 h and then IκBα and phosphorylated p65 protein expression was detected by Western blot. Data represent the mean ± SD of three independent experiments. **P < 0.01 vs. the control.
An increase in intracellular Ca2+ has been shown to promote the transcriptional activity of NF-κB [33]. HSV-2 infection has also been shown to promote the activation of NF-κB and the secretion of interleukins and chemokines [34]. According to the above findings, we decided to explore whether NF-κB activation induced by HSV-2 infection was due to Ca2+ influx through TRPV4 channels. We found that inhibition of the TRPV4 channel by HC067047 (100 nM) or EGTA (3.6 mM) markedly reduced the expression of phosphorylated p65 and IκBα in infected cells, as shown in Fig. 6d. These data indicate that the TRPV4 channel participates in NF-κB activation in HSV-2-infected cells.
Discussion
The transient receptor potential vanilloid (TRPV) channels have been implicated in various pathophysiological processes, including viral infections. The TRPV4 channel binds the DEAD-box RNA helicase DDX3X to regulate RNA virus infectivity [28]. Inhibition of the TRPV4 channel thus provides an antiviral effect against RNA viruses, such as the Zika virus [35]. This study found that TRPV1, TRPV3 and TRPV4 channels are expressed in human epithelial cells. A previous study reported a correlation between TRPV1 channel activity and HSV-2 infection and demonstrated that HSV-2 glycoprotein G modulates TRPV1 channel activation [15]. In infected epithelial cells, the expression of the TRPV3 channel is lower than that of the TRPV4 channel. In addition, the TRPV3 channel is mainly expressed in the endoplasmic reticulum (ER) [36]. The changes in [Ca2+]i play a critical role in the entry of herpes simplex virus into cells [1], indicating that the Ca2+-permeable channel expressed in the plasma membrane (TRPV4) is more important than the channel expressed in the ER (TRPV3) for viral entry. Thus, we investigate the effects of the TRPV4 channel on HSV-2 infection in this study. Our findings show that the TRPV4 channel, a Ca2+-permeable channel, directly binds HSV-2 glycoprotein D to facilitate HSV-2 infection and inflammation in host epithelial cells.
The HSV-2 virus enters the body primarily through epithelial cells and eventually establishes latent infections in the sacral ganglion [37]. The TRPV4 channel is abundantly expressed in nerve cells [38]. Therefore, we suspect that the interaction between the TRPV4 channel and glycoprotein D may be a potential mechanism underlying the establishment of latent infection in the sacral ganglion. Our study therefore implies that the TRPV4 channel plays a potential role in latent infection.
The TRPV4 channel protein contains 871 amino acids and four extracellular domains [6]. Which of these four extracellular domains is key to the interaction between the TRPV4 channel and glycoprotein D? We attempted to identify the specific binding site(s) of the TRPV4-gD interaction with virtual docking procedures. Multiple binding sites were predicted at the protein‒protein interface (data not shown). These binding sites are mutated and individually expressed in CHO cells during HSV-2 infection. However, differences in the interactions between glycoprotein D and the mutant TRPV4s have not been detected in infected CHO cells. This outcome may be explained as follows. On the one hand, CHO cells transfected with mutant TRPV4 and infected with HSV-2 have low survival rates. On the other hand, the TRPV4 channel has five different splice variants (TRPV4A-E), all of which have different amino acid deletions [7, 38]. Therefore, it’s reasonable for us to doubt that the effective interaction between glycoprotein D and the five different TRPV4 splice variants extensively differs; additionally, it would be complicated to analyze. The specific binding sites merit further evaluation.
Several pattern-recognition receptors (PRRs), such as TLRs and cyclic GMP-AMP synthase (cGAS), act as the sensors of HSV-2 [39,40,41]. These PRRs recognize the HSV-2 glycoprotein and then induce NF-κB activation and inflammatory secretion [32, 42], including TNF-α, IL-6, CXCL-9, and CXCL-10 [37, 43]. In addition, a rise in intracellular Ca2+ concentration can enhance transcription of NF-κB and thereby aggravate inflammatory signaling [44, 45]. Indeed, we found that blockade of the TRPV4 channel prevents the production of TNF-α, IL-6, CXCL-9, and CXCL-10 and reduces the phosphorylation of p65 in HSV-2-infected cells, indicating that the TRPV4 channel regulates the inflammatory signals caused by HSV-2 infection.
In conclusion, we propose the model shown in Fig. 7. During HSV-2 infection, the interaction between glycoprotein D and the TRPV4 channel triggers intracellular Ca2+ oscillation, an essential factor in virus entry [2, 4] that facilitates virus infection and exacerbates the activation of NF-κB. Blockade of the TRPV4 channel decreases the production of progeny viruses and the activation of NF-κB. Our findings elucidate the previously unknown role of the TRPV4 channel in HSV-2 infection. Further investigations are urgently needed to confirm that the TRPV4 channel is an entry receptor for HSV-2.
The TRPV4 channel is a calcium-permeable channel in epithelial cells. During HSV-2 infection, the interaction between glycoprotein D and the TRPV4 channel facilitates virus infection and exacerbates NF-κB activation by increasing the intracellular calcium concentration. Inhibition of TRPV4 channel activity diminishes viral infection and inflammation.
References
He D, Mao A, Li Y, Tam S, Zheng Y, Yao X, et al. TRPC1 participates in the HSV-1 infection process by facilitating viral entry. Sci Adv. 2020;6:z3367.
Cheshenko N, Trepanier JB, Gonzalez PA, Eugenin EA, Jacobs WJ, Herold BC. Herpes simplex virus type 2 glycoprotein H interacts with integrin alphavbeta3 to facilitate viral entry and calcium signaling in human genital tract epithelial cells. J Virol. 2014;88:10026–38.
Cheshenko N, Trepanier JB, Stefanidou M, Buckley N, Gonzalez P, Jacobs W, et al. HSV activates Akt to trigger calcium release and promote viral entry: novel candidate target for treatment and suppression. Faseb J. 2013;27:2584–99.
Cheshenko N, Liu W, Satlin LM, Herold BC. Multiple receptor interactions trigger release of membrane and intracellular calcium stores critical for herpes simplex virus entry. Mol Biol Cell. 2007;18:3119–30.
Ding L, Jiang P, Xu X, Lu W, Yang C, Li L, et al. T-type calcium channels blockers inhibit HSV-2 infection at the late stage of genome replication. Eur J Pharmacol. 2021;892:173782.
Pumroy RA, Fluck ER, Ahmed T, Moiseenkova-Bell VY. Structural insights into the gating mechanisms of TRPV channels. Cell Calcium. 2020;87:102168.
Toft-Bertelsen TL, MacAulay N. TRPing to the point of clarity: Understanding the function of the complex TRPV4 ion channel. Cells. 2021;10:2–16.
Taylor D, Hamid SM, Andres AM, Saadaeijahromi H, Piplani H, Germano JF, et al. Antiviral effects of menthol on Coxsackievirus B. Viruses. 2020;12:692–701.
Cortright DN, Buck ME, Krause JE. Hunting for ion channel modulators with herpes simplex virus. Nat Methods. 2007;4:692–3.
Sanjai KP, Nayak TK, Mahish C, Sahoo SS, Radhakrishnan A, De S, et al. Inhibition of transient receptor potential vanilloid 1 (TRPV1) channel regulates chikungunya virus infection in macrophages. Arch Virol. 2021;166:139–55.
Abdullah H, Heaney LG, Cosby SL, McGarvey LP. Rhinovirus upregulates transient receptor potential channels in a human neuronal cell line: implications for respiratory virus-induced cough reflex sensitivity. Thorax. 2014;69:46–54.
Harford TJ, Rezaee F, Scheraga RG, Olman MA, Piedimonte G. Asthma predisposition and respiratory syncytial virus infection modulate transient receptor potential vanilloid 1 function in children’s airways. J Allergy Clin Immunol. 2018;141:414–6.
Harford TJ, Grove L, Rezaee F, Scheraga R, Olman MA, Piedimonte G. RSV infection potentiates TRPV1-mediated calcium transport in bronchial epithelium of asthmatic children. Am J Physiol Lung Cell Mol Physiol. 2021;320:L1074–84.
Jing X, Yan W, Zeng H, Cheng W. Qingfei oral liquid alleviates airway hyperresponsiveness and mucus hypersecretion via TRPV1 signaling in RSV-infected asthmatic mice. Biomed Pharmacother. 2020;128:110340.
Cabrera JR, Viejo-Borbolla A, Alcami A, Wandosell F. Secreted herpes simplex virus-2 glycoprotein G alters thermal pain sensitivity by modifying NGF effects on TRPV1. J Neuroinflammation. 2016;13:210.
Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101–8.
Ding L, Jiang P, Xu X, Lu W, Yang C, Zhou P, et al. Resveratrol promotes HSV-2 replication by increasing histone acetylation and activating NF-kappaB. Biochem Pharmacol. 2020;171:113691.
Xie Q, Chen X, Meng ZM, Huang XL, Zhang Q, Zhou JQ, et al. Glial-derived neurotrophic factor regulates enteric mast cells and ameliorates dextran sulfate sodium-induced experimental colitis. Int Immunopharmacol. 2020;85:106638.
Sasaki K, Hayashi K, Matsuya Y, Sugimoto K, Lee JB, Kurosaki F, et al. In vitro and in vivo antiherpetic effects of (1R,2R)-1-(5’-methylful-3’-yl)propane-1,2,3-triol. J Nat Med. 2016;70:217–24.
Nilius B, Owsianik G. The transient receptor potential family of ion channels. Genome Biol. 2011;12:218.
Veteto AB, Peana D, Lambert MD, McDonald KS, Domeier TL. TRPV4 contributes to stretch-induced hypercontractility and time-dependent dysfunction in the aged heart. Cardiovasc Res. 2019;231:116555.
Geraghty RJ, Krummenacher C, Cohen GH, Eisenberg RJ, Spear PG. Entry of alphaherpesviruses mediated by poliovirus receptor-related protein 1 and poliovirus receptor. Science. 1998;280:1618–20.
Krummenacher C, Nicola AV, Whitbeck JC, Lou H, Hou W, Lambris JD, et al. Herpes simplex virus glycoprotein D can bind to poliovirus receptor-related protein 1 or herpesvirus entry mediator, two structurally unrelated mediators of virus entry. J Virol. 1998;72:7064–74.
Cocchi F, Lopez M, Dubreuil P, Campadelli FG, Menotti L. Chimeric nectin1-poliovirus receptor molecules identify a nectin1 region functional in herpes simplex virus entry. J Virol. 2001;75:7987–94.
Struyf F, Martinez WM, Spear PG. Mutations in the N-terminal domains of nectin-1 and nectin-2 reveal differences in requirements for entry of various alphaherpesviruses and for nectin-nectin interactions. J Virol. 2002;76:12940–50.
Ishino R, Kawase Y, Kitawaki T, Sugimoto N, Oku M, Uchida S, et al. Oncolytic virus therapy with HSV-1 for hematological malignancies. Mol Ther. 2021;29:762–74.
Du Q, Gu Z, Leneva I, Jiang H, Li R, Deng L, et al. The antiviral activity of arbidol hydrochloride against herpes simplex virus type II (HSV-2) in a mouse model of vaginitis. Int Immunopharmacol. 2019;68:58–67.
Donate-Macian P, Jungfleisch J, Perez-Vilaro G, Rubio-Moscardo F, Peralvarez-Marin A, Diez J, et al. The TRPV4 channel links calcium influx to DDX3X activity and viral infectivity. Nat Commun. 2018;9:2307.
Stahl JP, Mailles A. Herpes simplex virus encephalitis update. Curr Opin Infect Dis. 2019;32:239–43.
Rayees S, Joshi JC, Tauseef M, Anwar M, Baweja S, Rochford I, et al. PAR2-mediated cAMP generation suppresses TRPV4-dependent Ca2+ signaling in alveolar macrophages to resolve TLR4-induced inflammation. Cell Rep. 2019;27:793–805.
Triantafilou K, Eryilmazlar D, Triantafilou M. Herpes simplex virus 2-induced activation in vaginal cells involves Toll-like receptors 2 and 9 and DNA sensors DAI and IFI16. Am J Obstet Gynecol. 2014;210:121–2.
Tognarelli EI, Palomino TF, Corrales N, Bueno SM, Kalergis AM, Gonzalez PA. Herpes simplex virus evasion of early host antiviral responses. Front Cell Infect Microbiol. 2019;9:127.
Berry CT, May MJ, Freedman BD. STIM- and Orai-mediated calcium entry controls NF-kappaB activity and function in lymphocytes. Cell Calcium. 2018;74:131–43.
Lu X, Huang C, Zhang Y, Lin Y, Wang X, Li Q, et al. The Us2 gene product of herpes simplex virus 2 modulates NF-kappaB activation by targeting TAK1. Sci Rep. 2017;7:8396.
Donate-Macian P, Duarte Y, Rubio-Moscardo F, Perez-Vilaro G, Canan J, Diez J, et al. Structural determinants of TRPV4 inhibition and identification of new antagonists with antiviral activity. Br J Pharmacol. 2020;6:1239–43.
Lo IC, Chan HC, Qi Z, Ng KL, So C, Tsang SY. TRPV3 channel negatively regulates cell cycle progression and safeguards the pluripotency of embryonic stem cells. J Cell Physiol. 2016;231:403–13.
Iversen MB, Reinert LS, Thomsen MK, Bagdonaite I, Nandakumar R, Cheshenko N, et al. An innate antiviral pathway acting before interferons at epithelial surfaces. Nat Immunol. 2016;17:150–8.
Garcia-Elias A, Mrkonjic S, Jung C, Pardo-Pastor C, Vicente R, Valverde MA. The TRPV4 channel. Handb Exp Pharmacol. 2014;222:293–319.
Sun L, Wu J, Du F, Chen X, Chen ZJ. Cyclic GMP-AMP synthase is a cytosolic DNA sensor that activates the type I interferon pathway. Science. 2013;339:786–91.
Ansari MA, Dutta S, Veettil MV, Dutta D, Iqbal J, Kumar B, et al. Herpesvirus genome recognition induced acetylation of nuclear IFI16 is essential for its cytoplasmic translocation, inflammasome and IFN-beta responses. PLoS Pathog. 2015;11:e1005019.
Brun P, Scarpa M, Marchiori C, Conti J, Kotsafti A, Porzionato A, et al. Herpes simplex virus type 1 engages toll like receptor 2 to recruit macrophages during infection of enteric neurons. Front Microbiol. 2018;9:2148.
Marsden V, Donaghy H, Bertram KM, Harman AN, Nasr N, Keoshkerian E, et al. Herpes simplex virus type 2-infected dendritic cells produce TNF-alpha, which enhances CCR5 expression and stimulates HIV production from adjacent infected cells. J Immunol. 2015;194:4438–45.
Ichinohe T, Pang IK, Iwasaki A. Influenza virus activates inflammasomes via its intracellular M2 ion channel. Nat Immunol. 2010;11:404–10.
Bair AM, Thippegowda PB, Freichel M, Cheng N, Ye RD, Vogel SM, et al. Ca2+ entry via TRPC channels is necessary for thrombin-induced NF-kappaB activation in endothelial cells through AMP-activated protein kinase and protein kinase Cdelta. J Biol Chem. 2009;284:563–74.
Rao A. Signaling to gene expression: calcium, calcineurin and NFAT. Nat Immunol. 2009;10:3–5.
Acknowledgements
The research was supported by the National Natural Science Foundation of China (82003815 to PJ), Major Scientific and Technological Projects of Guangdong Province (2019B020202002 to SWL), Natural Science Foundation of Guangdong Province (2017A030310602 to PJ), Chinese Academy of Traditional Chinese Medicine (ZZ13-035-02 and 2019XZZX-LG04 to SWL), and Medical Scientific Research Foundation of Guangdong Province (A2017368 to PJ).
Author information
Authors and Affiliations
Contributions
SWL and PZZ conceived the idea and designed the research. PJ, SSL, XFX, CY, CC and JSW performed the research. PJ, SSL, PZZ and SWL analyzed the results and wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, P., Li, Ss., Xu, Xf. et al. TRPV4 channel is involved in HSV-2 infection in human vaginal epithelial cells through triggering Ca2+ oscillation. Acta Pharmacol Sin 44, 811–821 (2023). https://doi.org/10.1038/s41401-022-00975-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00975-7