Abstract
Objectives
Unrecognized delirium is associated with significant adverse outcomes. Despite decades of effort and educational initiatives, validated screening tools have not improved delirium recognition in the emergency department (ED). There remains a fundamental knowledge gap of why it is consistently missed. The objective of this study was to explore the perceptions of ED physicians and nurses regarding factors contributing to missed delirium in older ED patients.
Methods
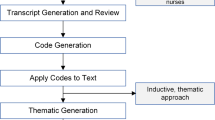
We conducted a qualitative descriptive study at two academic tertiary care EDs in Toronto, Canada. Emergency physicians and nurses were interviewed by a trained qualitative researcher using a semi-structured interview guide. We coded transcripts with an iteratively developed codebook. Interviews were conducted until thematic saturation occurred. Thematic data analysis occurred in conjunction with data collection to continuously monitor emerging themes and areas for further exploration.
Results
We interviewed 26 ED physicians and nurses. We identified key themes at four levels: clinical practice, provider attitudes, systematic processes, and education. The four themes include: (1) there are varied approaches to delirium recognition and infrequent use of screening tools; (2) delirium assessment is perceived as overly time consuming and of lower priority than other symptoms and syndromes; (3) it is unclear whose responsibility it is to recognize delirium; and (4) there is a need for a deeper or “functional” understanding of delirium that includes its consequences.
Conclusions
Our findings demonstrate a need for ED leadership to identify clear team roles for delirium recognition, standardize use of delirium screening tools, and prioritize delirium as a symptom of an acute medical emergency.
Résumé
Objectifs
Le délire non reconnu est associé à des résultats négatifs importants. Malgré des décennies d'efforts et d'initiatives éducatives, les outils de dépistage validés n'ont pas amélioré la reconnaissance du délire au service des urgences (SU). Il reste une lacune fondamentale dans la connaissance des raisons pour lesquelles elle est systématiquement manquée. L’objectif de cette étude était d’explorer les perceptions des médecins et des infirmières de l’urgence au sujet des facteurs contribuant au délire manqué chez les patients âgés des urgences.
Méthodes
Nous avons mené une étude qualitative descriptive dans deux urgences universitaires de soins tertiaires à Toronto, au Canada. Les médecins et les infirmières des urgences ont été interrogés par un chercheur qualitatif formé à l'aide d'un guide d'entretien semi-structuré. Nous avons codé les transcriptions à l'aide d'un livre de codes développé de manière itérative. Les entretiens ont été menés jusqu'à saturation thématique. L'analyse thématique des données s'est déroulée conjointement avec la collecte des données afin de surveiller continuellement les thèmes émergents et les domaines à explorer davantage.
Résultats
Nous avons interrogé 26 médecins et infirmières des urgences. Nous avons identifié des thèmes clés à quatre niveaux : la pratique clinique, les attitudes des prestataires, les processus systématiques et l'éducation. Les quatre thèmes abordés sont les suivants : 1) les approches de la reconnaissance du délire sont variées et les outils de dépistage peu utilisés ; 2) l'évaluation du délire est perçue comme prenant trop de temps et moins prioritaire que d'autres symptômes et syndromes ; 3) il n'est pas clair à qui revient la responsabilité de reconnaître le délire ; et 4) il est nécessaire d'avoir une compréhension plus profonde ou "fonctionnelle" du délire, qui inclut ses conséquences.
Conclusions
Nos résultats démontrent la nécessité pour les responsables des urgences de définir clairement les rôles de l'équipe pour la reconnaissance du delirium, de normaliser l'utilisation des outils de dépistage du delirium et d'accorder la priorité au delirium en tant que symptôme d'une urgence médicale aiguë.
Similar content being viewed by others
References
Ewan Alexander B, John H. Delirium within the emergency care setting, occurrence and detection: a systematic review. Emerg Med J. 2013;4:263.
Michel É, François R, Martin C, François P, Jane M, François B. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;8:977.
McCusker J, Cole M, Dendukuri N, Belzile É, Primeau F. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ. 2001;165(5):575–83.
Kakuma R, du Fort GG, Arsenault L, Perrault A, Platt RW, Monette J, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51(4):443–50.
LaHue SC, Douglas VC, Kuo T, Conell CA, Liu VX, Josephson SA, et al. Association between inpatient delirium and hospital readmission in patients >/= 65 years of age: a retrospective cohort study. J Hosp Med. 2019;14(4):201–6.
Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. J Am Geriatr Soc. 2014;3:462.
Han JH, Shintani A, Eden S, Morandi A, Solberg LM, Schnelle J, et al. Delirium in the Emergency department: an independent predictor of death within 6 months. Ann Emerg Med. 2010;3:244.
Lee JS, Tong T, Chignell M, Tierney MC, Goldstein J, Eagles D, et al. Prevalence, management and outcomes of unrecognized delirium in a National Sample of 1493 older emergency department patients: how many were sent home and what happened to them? Age Age. 2022;51(2).
Lewis LM, Miller DK, Morley JE, Nork MJ, Lasater LC. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13(2):142–5.
Elie M, Rousseau F, Cole M, Primeau F, McCusker J, Bellavance F. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;163(8):977–81.
Hustey FM, Meldon SW, Smith MD, Lex CK. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;41(5):678–84.
Han JH, Zimmerman EE, Cutler N, Schnelle J, Morandi A, Dittus RS, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193–200.
Wong CL, Holroyd-Leduc J, Simel DL, Straus SE. Does this patient have delirium? Value of bedside instruments. Chicago: American Medical Association; 2010. p. 779.
Carpenter C, Kennedy M, Arendts G, Schnitker L, Eagles D, Mooijaart S, et al. 243 accuracy of emergency department delirium screening: a diagnostic meta-analysis. Ann Emerg Med. 2018;72(4):S96–7.
Rockwood K. Educational interventions in delirium. Dement Geriatr Cogn Disord. 1999;10(5):426–9.
Young LJ, George J. Do guidelines improve the process and outcomes of care in delirium? Age Ageing. 2003;32(5):525–8.
LaMantia MA, Messina FC, Hobgood CD, Miller DK. Screening for delirium in the emergency department: a systematic review. Ann Emerg Med. 2014;63(5):551–60.
Colquhoun HL, Squires JE, Kolehmainen N, Fraser C, Grimshaw JM. Methods for designing interventions to change healthcare professionals’ behaviour: a systematic review. Implement Sci IS. 2017;12(1):30.
Eagles D, Cheung WJ, Avlijas T, Yadav K, Ohle R, Taljaard M, et al. Barriers and facilitators to nursing delirium screening in older emergency patients: a qualitative study using the theoretical domains framework. Age Ageing. 2022;51(1).
Sullivan-Bolyai S, Bova C, Harper D. Developing and refining interventions in persons with health disparities: the use of qualitative description. Nurs Outlook. 2005;53(3):127–33.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
DeCuir-Gunby JT, Marshall PL, McCulloch AW. Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods. 2011;23(2):136–55.
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis: sage; 2006.
Denzin NK, Lincoln, Y.S. Handbook of qualitative research. 2nd edition ed. Thousand Oaks: Sage. 2000.
Kelle U, Bird K. Computer-aided qualitative data analysis: theory, methods and practice: Sage. 1995.
Leaker H, Fox L, Holroyd-Leduc J. The impact of geriatric emergency management nurses on the care of frail older patients in the emergency department: a systematic review. Can Geriat J. 2020;23(3):250.
Kennedy M, Hwang U, Han JH. Delirium in the emergency department: moving from tool-based research to system-wide change. J Am Geriatr Soc. 2020;68(5):956–8.
Gage BF, Coopersmith CM, Stark S, Griffey RT, Carpenter CR. Physician and nurse acceptance of technicians to screen for geriatric syndromes in the emergency department. Western J Emerg Med. 2011;12(4):489.
Mohamed EH, Sandra H, Vincent S. Factors that contribute to underrecognition of delirium by registered nurses in acute care settings: a scoping review of the literature to explain this phenomenon. J Clin Nurs. 2015;78:906.
LaMantia MA, Messina FC, Jhanji S, Nazir A, Maina M, McGuire S, et al. Emergency medical service, nursing, and physician providers’ perspectives on delirium identification and management. Dementia (Lond Engl). 2017;16(3):329–43.
Daniel D, Alasdair M. Understanding barriers to delirium care: a multicentre survey of knowledge and attitudes amongst UK junior doctors. Age Ageing. 2009;5:559.
Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM Jr. Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161(20):2467–73.
McCrow J, Sullivan KA, Beattie ER. Delirium knowledge and recognition: a randomized controlled trial of a web-based educational intervention for acute care nurses. Nurse Educ Today. 2014;34(6):912–7.
Rockwood K, Cosway S, Stolee P, Kydd D, Carver D, Jarrett P, et al. Increasing the recognition of delirium in elderly patients. J Am Geriatr Soc. 1994;42(3):252–6.
Hillman A. ‘Why must I wait?’The performance of legitimacy in a hospital emergency department. Sociol Health Illn. 2014;36(4):485–99.
Pérez-Ros P, Martínez-Arnau FM. Delirium assessment in older people in emergency departments. A literature review. Diseases. 2019;7(1):14.
Hare M, Wynaden D, McGowan S, Speed G. Assessing cognition in elderly patients presenting to the emergency department. Int Emerg Nurs. 2008;16(2):73–9.
Schofield I, Dewing J. The care of older people with a delirium in acute care settings. Nurs Older People. 2001;13(1):21–5.
Babine RL, Honess C, Wierman HR, Hallen S. The role of clinical nurse specialists in the implementation and sustainability of a practice change. J Nurs Manag. 2016;24(1):39–49.
Yevchak AM. Informal caregiver detection, recognition, and reporting of symptoms of delirium in hospitalized older adults with dementia: Pennsylvania State University; 2013.
Bridges J, Collins P, Flatley M, Hope J, Young A. Older people's experiences in acute care settings: systematic review and synthesis of qualitative studies. Int J Nurs Stud. 2020;102.
Rice KL, Bennett MJ, Clesi T, Linville L. Mixed-methods approach to understanding nurses’ clinical reasoning in recognizing delirium in hospitalized older adults. J Contin Educ Nurs. 2014;45(3):136–48.
Acknowledgements
Dr. Jacques S. Lee is supported by the Schwartz/Reisman Emergency Medicine Institute (SREMI) Inaugural Research Chair in Geriatric Emergency Medicine. Dr. Katie N. Dainty is supported by the North York General Hospital Research Chair in Patient-Centred Outcomes.
Funding
Canadian Association of Emergency Physicians (CAEP) 2019 Junior Investigators Grant.
Author information
Authors and Affiliations
Contributions
JSL, RS and KD conceived the study and designed the methods. All authors contributed to the grant application to obtain research funding. RS led recruitment, conduction of the interviews, and data management. Under the guidance of KD, RS completed the data analysis; KD provided expertise on study design and assisted in data analysis. RS drafted the manuscript. All authors contributed substantially to editing the manuscript and approved the final submission. RS takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
RS, KND, SLM, DM, and JSL report no conflict of interest.
Presentations
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schonnop, R., Dainty, K.N., McLeod, S.L. et al. Understanding why delirium is often missed in older emergency department patients: a qualitative descriptive study. Can J Emerg Med 24, 820–831 (2022). https://doi.org/10.1007/s43678-022-00371-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00371-4