Abstract
Background
The field of bariatric surgery has seen peaks and troughs in the types of metabolic procedures performed. Our primary aim was to evaluate bariatric case volumes among fellows enrolled in bariatric Fellowship Council (FC)-accredited programs. Our secondary aim was to assess trends in revisional case volumes.
Methods
We reviewed de-identified FC case logs for all bariatric surgery-accredited programs from 2010 through 2019. The number of primary sleeve gastrectomy, gastric band, gastric bypass, biliopancreatic diversion, and major revisional bariatric surgical procedures (defined as a revision with creation of a new anastomosis) were graphed for each academic year. Fellows were stratified into quartiles based on the number of revisional operations per year and graphed over ten years. Volumes of primary gastric bypass, major revisions, and total anastomotic cases were compared over time using ANOVA with p < 0.05 considered significant.
Results
Case volumes for 822 fellows were evaluated. Sleeve gastrectomy had a significant surge in 2010 and plateaued in 2016. The fellows’ number of primary gastric bypasses had a non-significant decrease from 84 to 75 cases/fellow from 2010 to 2019. This decrease was offset by a significant increase in major revisional surgery from 8 to 19 cases/fellow. As a result, the number of anastomotic cases did not change significantly over the study time period. Interestingly, as revisional volume has grown, the gap between quartiles of fellowship programs has widened with the 95th percentile growing at a much faster rate than lower quartiles.
Conclusion
The volume of bariatric procedures performed in the last decade among FC fellows follows similar trends to national data. Major revisional cases have doubled with the most robust growth isolated to a small number of programs. As revisional surgery continues to increase, applicants interested in a comprehensive bariatric practice should seek out training programs that offer strong revisional experience.
Similar content being viewed by others
Over the years, the field of metabolic and bariatric surgery has seen peaks and troughs in the types of weight loss procedures performed. The International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) published a worldwide survey showing procedure trends from 2008 to 2016 [1]. There was an increase in total number of bariatric surgical procedures performed, with significant increases in sleeve gastrectomy and decreases in gastric band placement. Revisional procedures represented 7% of the total procedural volume, with the majority of cases being performed in Europe and North America [1]. Furthermore, the American Society for Metabolic and Bariatric Surgery (ASMBS) estimated a 10% increase in the last decade in revisional surgeries. In 2019, 16.7% of total bariatric surgery cases were revisions [2]. As a result, it is important that bariatric surgeons and fellows familiarize themselves with re-operative procedures [3].
As the field of metabolic and bariatric surgery grows, many general surgery graduates have chosen to pursue additional fellowship training in programs accredited by the Fellowship Council (FC). Fellowship training has been shown to improve perioperative outcomes during a bariatric surgeons’ early experience and to accelerate the learning curve in the first year following completion of training [4]. Not only does a fellowship program benefit the trainee, it also correlates with improved hospital outcomes and has no impact on major safety benchmarks [5, 6]. It is imperative then to assess the growth patterns of primary and revisional bariatric surgery within fellowship training programs.
The purpose of this study was to longitudinally evaluate the inclusion of revisional surgery cases in FC fellowship training over the last decade. Our primary aim was to evaluate the index bariatric surgery case volumes among fellows enrolled in FC-accredited bariatric surgery fellowships. The secondary aim was to assess trends in revisional bariatric volume at these same programs.
Materials and methods
This study was determined to be exempt from review by the Institutional Review Board at the University of Texas Southwestern Medical Center (STU-2018-0331). The study design was reviewed by the FC Research Committee and Executive Committee and approved prior to the release of data. All names of institutions and fellows were replaced with a unique identifier (Program ID and Fellow ID, respectively) before the data were shared with the study team such that authors only had access to de-identified data.
We reviewed 10 years of FC case log data starting with the 2010 academic year (fellows graduating in summer 2010) and ending with the 2019 academic year (fellows graduating in summer 2019). These data represent cases completed in the decade before elective surgery disruptions related to the COVID-19 pandemic. Fellows were included in the analysis if they completed a bariatric surgery-accredited program. This included fellows who completed training at dual-accredited programs (e.g., advanced gastrointestinal/minimally invasive surgery and bariatric surgery).
Our data set included unique Fellow ID’s in each academic year. However, examination of the data revealed that some Fellow ID’s logged very few cases per academic year. These may have been fellows that were on a research year, ones that did not complete their program, or fellows that logged cases erroneously. Thus, to estimate the true number of clinically active fellows for each year analyzed, we calculated the total number of cases logged (including non-bariatric cases) by each Fellow ID. We then filtered out any Fellow ID that had logged fewer than 100 procedures in the academic year analyzed.
To examine trends in volumes of index bariatric surgical procedures performed each academic year, the cases were stratified into five types: sleeve gastrectomy, gastric band, gastric bypass, biliopancreatic diversion, and major revisional bariatric procedure. A major revisional procedure was defined as a revision with creation of a new anastomosis, for example, gastric band removal with conversion to gastric bypass. Therefore, cases such as band removal alone or conversion to sleeve gastrectomy were not included as major revisions. For each of the five case types, we calculated the mean volume per fellow for that academic year and graphed it over 10 years. The means were compared using ANOVA with p < 0.05 considered significant.
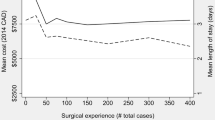
In order to provide more granular data regarding revisional bariatric surgery case volumes, we calculated the 25th percentile, 50th percentile, 75th percentile, and 95th percentile benchmarks for revisional surgery volume each year. These benchmarks were then graphed over the 10 years to observe whether growth in revisional volume was consistent across the whole cohort of fellows or whether it was driven primarily by top quartiles. The same descriptive analysis was performed for total anastomotic procedures (i.e., gastric bypass, duodenal switch, and major revisional procedures).
Results
Our study included 298,017 cases performed by 822 fellows. The sleeve gastrectomy had a significant surge in fellowship training in 2010 from an average of 8 cases/fellow to a peak of 85 cases/fellow in 2016 where the volume was noted to plateau (Fig. 1). The primary gastric bypass had a non-significant decrease from an average of 84 to 75 cases/fellow (p = 0.78). Revisional anastomotic cases had a significant increase from 8 to 19 cases/fellow (p = 2 × 10–15). These data are displayed in Fig. 2. As a result, the increase in revisional surgery offset the decrease in primary gastric bypass with minimal fluctuations in the overall number of anastomotic case volume for fellows (Fig. 3).
When examining the distribution of major revisional bariatric cases, all fellows had an increase in case volume (Fig. 2). The fellows with the volumes in the 95th percentile had a much faster growth rate over the 10-year period compared to the 25th, 50th, and 75th quartiles. The gap between the quartiles of fellowship programs widened by 2019, with the majority of revisional cases being done by the top 5% of high-volume programs.
Discussion
Bariatric surgery case volume growth in fellowship programs mirrors national procedural data [2]. Bariatric surgeons and fellows have seen a substantial rise in the number of sleeve gastrectomy procedures performed and a significant decline in the placement of gastric bands. The one difference between descriptive FC fellowship program and ASMBS data has been primary gastric bypass case volumes. The fellows who were part of FC-accredited programs did not see as significance of a decline in gastric bypass procedures performed as compared to the national procedural volume average, in which there was a 20% decline from 2011 to 2019 [2].
The average number of revisional cases per fellow per academic year has doubled in the last decade. Similarly, national data show that revisional cases increased from 6 to 16% over the same time period. Our study demonstrates that the most robust growth in revisional case volume, among FC training programs, is isolated to a small number of training programs. These results are comparable to a survey conducted by Mahawar et al. of 456 metabolic and bariatric surgeons [7]. The survey found that the majority of surgeons (44%) were performing less than 10 revisional procedures per year compared to a small proportion of surgeons (4%) who were doing more than 100 revisions per year. Internationally, revisional bariatric cases are also mainly isolated to Europe (11% of all bariatric interventions) and North America (10%) when compared to Latin America (1%) [1].
Despite a small number of facilities and surgeons performing a disproportionate volume of revisional surgery, our study shows that all fellows are seeing a higher number of bariatric revisions. This is likely due to improved outcomes in regards to weight loss and resolution/control of medical co-morbidities and post-procedural complications, such as gastroesophageal reflux disease [8, 9]. Revisional procedures are typically more complicated with longer operative times, potentially increased complication rates, and the necessity for an advanced technical skill set [10]. As revisional surgery continues to increase, future bariatric surgeons interested in a comprehensive practice can seek out training programs that offer strong revisional experience, pursue job opportunities with great mentorship, look for additional training courses, and attend conferences related to this matter.
A survey of graduated fellows indicated that FC-accredited fellowship programs prepare surgeons for independent practice, bridge training gaps, and help fellows acquire desired jobs [11]. This study shows that fellows are performing bariatric surgical procedures at volumes comparable to national data and getting increased exposure to revisional operations. This likely contributes to the high satisfaction of graduated fellows and should continue to be of great importance for the FC moving forward.
The limitations to this study included primarily a database dependent on accuracy of the fellows’ self-reported case log. For example, if they logged a gastric band revision to gastric bypass as a primary bypass case that would change our data analysis. However, this likely would have underestimated the volume of revisional cases in FC-accredited programs.
In regards to anastomotic cases, all FC-accredited bariatric surgery fellowships require 50 anastomotic procedures, which likely influenced the higher gastric bypass numbers as compared to the national average.
Potential changes in FC-accredited fellowships case logs may be needed to more clearly delineate the type of revisions being performed [e.g., clarifying the historical bariatric procedure (gastric band, gastric sleeve, fixed gastric band, vertical banded gastroplasty, prior failed fundoplication) and the revisional procedure (gastric bypass or duodenal switch)]. This may better stratify the volume and complexity of revisions being performed by program faculty and fellows.
Revisions to non-anastomotic operations (i.e., gastric band to sleeve gastrectomy) were not compared, as we restricted our analysis to more complex revisions (revisions to an anastomotic case). In that regard, as the population of sleeve gastrectomy patients continues to increase, we believe revisions to anastomotic cases are likely to increase due to issues related to weight regain and reflux [12].
Cases performed during the years of the COVID-19 pandemic were excluded. Further study is required to more fully understand the effects of the COVID-19 pandemic on fellow case volumes, as well as the pace of recovery of volumes to pre-pandemic levels.
Despite the limitations of our database, we believe that our study shows that the FC-accredited bariatric surgery fellowship programs offer exposure to a wide variety of bariatric surgery, including revisional bariatric procedures.
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N (2018) IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28:3783–3794. https://doi.org/10.1007/s11695-018-3450-2
ASMBS (2021) Estimate of bariatric surgery numbers, 2011–2019. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers
Aleman R, Menzo EL, Szomstein S, Rosenthal RJ (2020) Reoperative bariatric surgery. In: Nguyen NT, Brethauer SA, Morton JM, Ponce J, Rosenthal RJ (eds) The ASMBS textbook of bariatric surgery. Springer, Cham, pp 265–280
Agrawal S (2011) impact of bariatric fellowship training on perioperative outcomes for laparoscopic roux-en-y gastric bypass in the first year as consultant surgeon. Obes Surg 21:1817–1821. https://doi.org/10.1007/s11695-011-0482-2
Goldberg I, Yang J, Park J, Pryor AD, Docimo S, Bates AT, Talamini MA, Spaniolas K (2019) Surgical trainee impact on bariatric surgery safety. Surg Endosc 33:3014–3025. https://doi.org/10.1007/s00464-018-6587-0
Kim PS, Telem DA, Altieri MS, Talamini M, Yang J, Zhang Q, Pryor AD (2015) Bariatric outcomes are significantly improved in hospitals with fellowship council-accredited bariatric fellowships. J Gastrointest Surg 19:594–597. https://doi.org/10.1007/s11605-015-2758-7
Mahawar KK, Nimeri A, Adamo M, Borg C, Singhal R, Khan O, Small PK (2018) Practices concerning revisional bariatric surgery: a survey of 460 surgeons. Obes Surg 28:2650–2660. https://doi.org/10.1007/s11695-018-3226-8
Koh ZJ, Chew CAZ, Zhang JJY, Syn N, Kim G, Yan So JB, Shabbir A (2020) Metabolic outcomes after revisional bariatric surgery: a systematic review and meta-analysis. Surg Obes Relat Dis 16:1442–1454. https://doi.org/10.1016/j.soard.2020.05.029
Spyropoulos C, Kehagias I, Panagiotopoulos S, Mead N, Kalfarentzos F (2010) Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg 145:173–177. https://doi.org/10.1001/archsurg.2009.260
Clapp B, Harper B, Dodoo C, Klingsporn W, Barrientes A, Cutshall M, Tyroch A (2020) Trends in revisional bariatric surgery using the MBSAQIP database 2015–2017. Surg Obes Relat Dis 16:908–915. https://doi.org/10.1016/j.soard.2020.03.002
Watanabe Y, Madani A, Bilgic E, McKendy KM, Enani G, Ghaderi I, Fried GM, Feldman LS, Vassiliou MC, for the Research Committee of the, Fellowship Council (2017) Don’t fix it if it isn’t broken: a survey of preparedness for practice among graduates of fellowship council-accredited fellowships. Surg Endosc 31:2287–2298. https://doi.org/10.1007/s00464-016-5231-0
Musella M, Berardi G, Velotti N, Schiavone V, Vitiello A (2021) Ten-year results of laparoscopic sleeve gastrectomy: retrospective matched comparison with laparoscopic adjustable gastric banding—is there a significant difference in long term? Obes Surg 31:5267–5274. https://doi.org/10.1007/s11695-021-05735-w
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Shinil Shah has an unrelated research grant from Activ Surgical. Dr. Erik Wilson has unrelated grants from Apollo and USGI as well as unrelated honoraria from Intuitive, Medtronic, Johnson & Johnson and Gore Medical. Sara Monfared, Joshua Weis, Daniel Scott, and Melissa Felinski have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Monfared, S., Weis, J.J., Shah, S.K. et al. The rising tide of revisional surgery: tracking changes in index cases among bariatric-accredited fellowships. Surg Endosc 37, 4824–4828 (2023). https://doi.org/10.1007/s00464-022-09622-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09622-y