Abstract
Background
Further data are necessary to evaluate the risk of complications associated with the use of non-steroidal anti-inflammatory drugs (NSAIDs) postoperatively. This study aimed to determine the correlation between the use of NSAIDs in intravenous patient-controlled analgesia (IV-PCA) and postoperative complications after laparoscopic gastrectomy in patients with gastric cancer.
Methods
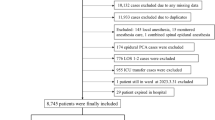
This retrospective, single-center study was conducted. The study population comprised 2150 patients who underwent laparoscopic gastrectomy for gastric cancer treatment. They were divided into two groups: non-NSAIDs (n = 1215) and NSAIDs (n = 935) according to their use of the drugs. Clinicopathologic characteristics, operative details, postoperative complications within 30 days, risk factors for complications, and survival were analyzed.
Results
Of the 2150 patients, 935 (43.49%) used NSAIDs. The overall complication rate showed no significant difference between the NSAIDs and non-NSAIDs groups (22.7% vs. 20.7%, p = 0.280), while the rates of anastomotic leakage and duodenal leakage were higher in the NSAID group (2.4% vs. 0.7%, p = 0.002 and 1.8% vs. 0.6%, p = 0.007, respectively). The rates of intra-abdominal bleeding and intra-abdominal abscess were significantly higher in the NSAID group (2.1% vs. 0.7%, p = 0.005 and 1.5% vs. 0.4%, p = 0.008, respectively). However, postoperative ileus occurred more frequently in the non-NSAID group (3.0% vs. 1.4%, p = 0.015). On multivariate analysis, NSAID use was an independent risk factor for early postoperative complications (1.303 [1.042–1.629], p = 0.020). Meanwhile, the NSAID group showed no differences in overall survival at each pathological stage.
Conclusion
Postoperative NSAID use by IV-PCA is associated with anastomotic leakage, duodenal stump leakage, intra-abdominal bleeding, and intra-abdominal abscess in patients who underwent laparoscopic gastrectomy for gastric cancer. Caution is advised when NSAIDs are used peri-operatively.
Graphical abstract


Similar content being viewed by others
References
Information Committee of the Korean Gastric Cancer Association (2021) Korean Gastric Cancer Association-Led Nationwide Survey on Surgically Treated Gastric Cancers in 2019. J Gastric Cancer 21(3):221–235
Papenfuss WA et al (2014) Morbidity and mortality associated with gastrectomy for gastric cancer. Ann Surg Oncol 21(9):3008–3014
Risser A et al (2009) NSAID prescribing precautions. Am Fam Phys 80(12):1371–1378
Bacchi S et al (2012) Clinical pharmacology of non-steroidal anti-inflammatory drugs: a review. Antiinflamm Antiallergy Agents Med Chem 11(1):52–64
Inan A, Koca C, Sen M (2006) Effects of diclofenac sodium on bursting pressures of anastomoses and hydroxyproline contents of perianastomotic tissues in a laboratory study. Int J Surg 4(4):222–227
Tibble JA et al (2000) Comparison of the intestinal toxicity of celecoxib, a selective COX-2 inhibitor, and indomethacin in the experimental rat. Scand J Gastroenterol 35(8):802–807
Busti AJ et al (2005) Effects of perioperative antiinflammatory and immunomodulating therapy on surgical wound healing. Pharmacotherapy 25(11):1566–1591
Vonkeman HE, van de Laar MA (2010) Nonsteroidal anti-inflammatory drugs: adverse effects and their prevention. Semin Arthritis Rheum 39(4):294–312
Jamjittrong S et al (2020) Postoperative non-steroidal anti-inflammatory drugs and anastomotic leakage after gastrointestinal anastomoses: systematic review and meta-analysis. Ann Gastroenterol Surg 4(1):64–75
Kverneng Hultberg D et al (2017) Nonsteroidal anti-inflammatory drugs and the risk of anastomotic leakage after anterior resection for rectal cancer. Eur J Surg Oncol 43(10):1908–1914
Klein M, Gögenur I, Rosenberg J (2012) Postoperative use of non-steroidal anti-inflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data. BMJ 345:e6166
Saleh F et al (2014) Perioperative nonselective non-steroidal anti-inflammatory drugs are not associated with anastomotic leakage after colorectal surgery. J Gastrointest Surg 18(8):1398–1404
Fjederholt KT et al (2018) Ketorolac and other NSAIDs increase the risk of anastomotic leakage after surgery for GEJ cancers: a cohort study of 557 patients. J Gastrointest Surg 22(4):587–594
Yoon S et al (2021) Effect of postoperative non-steroidal anti-inflammatory drugs on anastomotic leakage after pancreaticoduodenectomy. Korean J Anesthesiol 75:61–70
Stumpf M et al (2002) Collagen distribution and expression of matrix metalloproteinases 1 and 13 in patients with anastomotic leakage after large-bowel surgery. Langenbecks Arch Surg 386(7):502–506
van der Ham AC et al (1990) Eicosanoid profile of healing colon anastomosis and peritoneal macrophages in the rat. Gut 31(7):807–811
Hendriks T, Mastboom WJ (1990) Healing of experimental intestinal anastomoses. Dis Colon Rectum 33(10):891–901
Hendriks JM et al (1999) Experimental study of intraperitoneal suramin on the healing of colonic anastomoses. Br J Surg 86(9):1171–1175
Sheth KR et al (2020) Perioperative bleeding and non-steroidal anti-inflammatory drugs: an evidence-based literature review, and current clinical appraisal. Medicine (Baltimore) 99(31):e20042
Ghaferi AA, Birkmeyer JD, Dimick JB (2009) Variation in hospital mortality associated with inpatient surgery. N Engl J Med 361(14):1368–1375
Castellsague J et al (2012) Individual NSAIDs and upper gastrointestinal complications. Drug Saf 35(12):1127–1146
Ruggeri ZM (2006) Platelet interactions with vessel wall components during thrombogenesis. Blood Cells Mol Dis 36(2):145–147
Scharf RE (2012) Drugs that affect platelet function. Semin Thromb Hemost 38:865–883
Weng TC et al (2011) Ibuprofen worsens Streptococcus pyogenes soft tissue infections in mice. J Microbiol Immunol Infect 44(6):418–423
Rimailho A et al (1987) Fulminant necrotizing fasciitis and nonsteroidal anti-inflammatory drugs. J Infect Dis 155(1):143–146
Lepelletier D et al (2017) Is there an association between prior anti-inflammatory drug exposure and occurrence of peritonsillar abscess (PTA)? A national multicenter prospective observational case-control study. Eur J Clin Microbiol Infect Dis 36(1):57–63
Douketis JD et al (2012) Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e326S-e350S
Kim SH et al (2015) Risk factors for anastomotic leakage: a retrospective cohort study in a single gastric surgical unit. J Gastric Cancer 15(3):167–175
Acknowledgements
The authors thank Professor Hoon Choi of the Department of Anesthesiology for his advice in this study. The authors also wish to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2021.
Funding
This study was financially supported by the Korean Gastric Cancer Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
So Jung Kim, Chul Hyo Jeon, Han Hong Lee, Kyo Young Song, and Ho Seok Seo have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, S.J., Jeon, C.H., Lee, H.H. et al. Impact of postoperative NSAIDs (IV-PCA) use on short-term outcomes after laparoscopic gastrectomy for the patients of gastric cancer. Surg Endosc 37, 1123–1131 (2023). https://doi.org/10.1007/s00464-022-09600-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09600-4