Abstract
Purpose
Current guidelines recommend hospital admission for patients who present to the emergency department (ED) with chest pain and are scored as intermediate risk for adverse outcomes based on the HEART score. While hospital admission for these patients allows for timely investigation and treatment, it is a resource-intensive process. This study examines whether intermediate HEART score patients can be safely managed on an outpatient basis through rapid access chest pain clinics.
Methods
This retrospective observational study included all ED chest pain patients referred to rapid access clinics from January 2018 to April 2020 in Regina and Saskatoon, Saskatchewan. ED physician HEART scores were used in lieu of reviewer HEART scores when available. The primary outcome was the rate of major adverse coronary events (MACE), a composite measure of death, acute coronary syndrome, stroke, coronary angiography, and revascularization at 6 weeks in intermediate-risk patients. Secondary outcomes were the type of MACE, rate of MACE before rapid access clinic appointment and the most predictive component of the HEART score.
Results
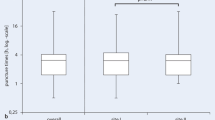
There were 1989 ED referrals, of which 817 were for intermediate-risk patients. 9.3% of intermediate-risk patients had a MACE at 6 weeks. MACE occurred before rapid access clinic follow-up in 1.1% of intermediate-risk patients, with coronary angiography being the most common MACE. Excluding coronary angiography, the risk of MACE before rapid access clinic follow-up was 0.7% in intermediate-risk patients. Components of the HEART score most predictive of MACE were troponin (OR 11.0, 95% CI: 3.7–32.3) and history (5.3, 95% CI: 2.4–11.8).
Conclusion
This study demonstrates that rapid access clinics are likely a safe alternative to admission for intermediate-risk chest pain patients and could reduce costly inpatient admissions for chest pain. With angiography excluded, MACE rates were well below the American College of Emergency Physicians cited 2% threshold.
Résumé
Objectif
Les directives actuelles recommandent l'admission à l'hôpital des patients qui se présentent aux urgences avec une douleur thoracique et qui sont classés comme présentant un risque intermédiaire d'effets indésirables selon le score HEART. Bien que l’hospitalisation de ces patients permette une investigation et un traitement en temps opportun, il s’agit d’un processus exigeant en ressources. Cette étude examine si les patients ayant un score HEART intermédiaire peuvent être pris en charge en toute sécurité en ambulatoire par des cliniques d'accès rapide aux douleurs thoraciques.
Méthodes
Cette étude observationnelle rétrospective a inclus tous les patients souffrant de douleurs thoraciques aux urgences orientés vers des cliniques d'accès rapide de janvier 2018 à avril 2020 à Regina et Saskatoon, en Saskatchewan. Les scores HEART des médecins des urgences ont été utilisés à la place des scores HEART des examinateurs lorsqu'ils étaient disponibles. Le principal résultat était le taux d'événements coronariens indésirables majeurs (MACE), une mesure composite du décès, du syndrome coronarien aigu, de l'accident vasculaire cérébral, de l'angiographie coronaire et de la revascularisation à 6 semaines chez les patients à risque intermédiaire. Les résultats secondaires étaient le type de MACE, le taux de MACE avant un rendez-vous à la clinique d’accès rapide et la composante la plus prédictive du score HEART.
Résultats
Il y a eu 1989 orientations vers les urgences, dont 817 pour des patients à risque intermédiaire. 9,3 % des patients à risque intermédiaire ont subi un MACE à 6 semaines. Un MACE est survenu avant le suivi clinique d'accès rapide chez 1,1 % des patients à risque intermédiaire, la coronarographie étant le MACE le plus fréquent. À l’exclusion de l’angiographie coronarienne, le risque de MACE avant le suivi clinique d’accès rapide était de 0,7 % chez les patients à risque intermédiaire. Les composants du score HEART les plus prédictifs de MACE étaient la troponine (OR 11,0, IC 95 % : 3,7-32,3) et les antécédents (5,3, IC 95 % : 2,4-11,8).
Conclusion
Cette étude démontre que les cliniques d'accès rapide sont probablement une alternative sûre à l'admission pour les patients souffrant de douleurs thoraciques à risque intermédiaire et pourraient réduire les admissions coûteuses de patients hospitalisés pour des douleurs thoraciques. En excluant l'angiographie, les taux de MACE étaient bien inférieurs au seuil de 2 % cité par l'American College of Emergency Physicians.


Similar content being viewed by others
Availability of data and materials
The data supporting the findings of the study are available within the article. Raw data will be stored with the principal investigator.
Code availability
N/A.
References
Christenson J, Innes G, McKnight D, Boychuk B, Grafstein E, Thompson CR, et al. Safety and efficiency of emergency department assessment of chest discomfort. CMAJ. 2004;170(12):1803–7.
Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, et al. Missed Diagnoses of Acute Cardiac Ischemia in the Emergency Department. N Engl J Med. 2000;342(16):1163–70.
Fanaroff AC, Rymer JA, Goldstein SA, Simel DL, Newby LK. Does this patient with chest pain have acute coronary syndrome?: The rational clinical examination systematic review. JAMA. 2015;314:1955–65.
Mehta RH, Eagle KA. Missed Diagnoses of Acute Coronary Syndromes in the Emergency Room — Continuing Challenges. N Engl J Med. 2000;342(16):1207–10.
Sandhu AT, Heidenreich PA, Bhattacharya J, Bundorf MK. Cardiovascular testing and clinical outcomes in emergency department patients with chest pain. JAMA Intern Med. 2017;177(8):1175–82.
Reinhardt SW, Lin CJ, Novak E, Brown DL. Noninvasive cardiac testing vs clinical evaluation alone in acute chest pain: A secondary analysis of the ROMICAT-II randomized clinical trial. In: JAMA Internal Medicine. American Medical Association; 2018. p. 212–9.
Chew PG, Frost F, Mullen L, Fisher M, Zadeh H, Grainger R, et al. A direct comparison of decision rules for early discharge of suspected acute coronary syndromes in the era of high sensitivity troponin. Eur Hear J Acute Cardiovasc Care. 2019;8(5):421–31.
Poldervaart JM, Langedijk M, Backus BE, Dekker IMC, Six AJ, Doevendans PA, et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol. 2017;227:656–61.
Fernando SM, Tran A, Cheng W, Rochwerg B, Taljaard M, Thiruganasambandamoorthy V, et al. Prognostic Accuracy of the HEART Score for Prediction of Major Adverse Cardiac Events in Patients Presenting With Chest Pain: a Systematic Review and Meta-analysis. Vol. 26, Academic Emergency Medicine. Blackwell Publishing Inc; 2019. p. 140–51.
Backus BE, Six AJ, Kelder JC, Mast TP, Van Den Akker F, Mast EG, et al. Chest pain in the emergency room: A multicenter validation of the heart score. Crit Pathw Cardiol. 2010;9(3):164–9.
Backus BE, Six AJ, Kelder JC, Bosschaert MAR, Mast EG, Mosterd A, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168(3):2153–8.
Mahler SA, Riley RF, Hiestand BC, Russell GB, Hoekstra JW, Lefebvre CW, et al. The HEART pathway randomized trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8(2):195–203.
Klimis H, Thiagalingam A, Altman M, Atkins E, Figtree G, Lowe H, et al. Rapid-access cardiology services: can these reduce the burden of acute chest pain on Australian and New Zealand health services? Intern Med J. 2017;47(9):986–91.
Marchick MR, Setteducato ML, Revenis JJ, Robinson MA, Weeks EC, Payton TF, et al. Comparison of 3 symptom classification methods to standardize the history component of the HEART score. Crit Pathw Cardiol. 2017;16(3):102–4.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618–51.
Jain T, Nowak R, Hudson M, Frisoli T, Jacobsen G, McCord J. Short-and long-term prognostic utility of the HEART score in patients evaluated in the emergency department for possible acute coronary syndrome. Crit Pathw Cardiol. 2016;15(2):40–5.
Mahler SA, Hiestand BC, Goff DC, Hoekstra JW, Miller CD. Can the HEART score safely reduce stress testing and cardiac imaging in patients at low risk for major adverse cardiac events? Vol. 10, Critical Pathways in Cardiology. 2011. p. 128–33.
Laureano-Phillips J, Robinson RD, Aryal S, Blair S, Wilson D, Boyd K, et al. HEART Score Risk Stratification of Low-Risk Chest Pain Patients in the Emergency Department: A Systematic Review and Meta-Analysis. Vol. 74, Annals of Emergency Medicine. Mosby Inc.; 2019. p. 187–203.
Sharp AL, Wu YL, Shen E, Redberg R, Lee MS, Ferencik M, et al. The HEART Score for Suspected Acute Coronary Syndrome in U.S. Emergency Departments. Vol. 72, Journal of the American College of Cardiology. Elsevier USA; 2018. p. 1875–7.
Brown MD, Wolf SJ, Byyny R, Diercks DB, Gemme SR, Gerardo CJ, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Emergency Department Patients With Suspected Non–ST-Elevation Acute Coronary Syndromes. Vol. 72, Annals of Emergency Medicine. Mosby Inc.; 2018. p. e65–106.
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Netherlands Hear J. 2008;16(6):191–6.
Wu WK, Yiadom MYAB, Collins SP, Self WH, Monahan K. Documentation of HEART score discordance between emergency physician and cardiologist evaluations of ED patients with chest pain. Am J Emerg Med. 2017;35(1):132–5.
O’Rielly CM, Andruchow JE, McRae AD. External validation of a low HEAR score to identify emergency department chest pain patients at very low risk of major adverse cardiac events without troponin testing. CJEM. 2022;24(1):68–74.
Spiegel R, Sutherland M, Brown R, Honasoge A, Witting M. Clinically relevant adverse cardiovascular events in intermediate heart score patients admitted to the hospital following a negative emergency department evaluation. Am J Emerg Med. 2021;1(46):469–75.
Melki D, Jernberg T. HEART score: A simple and useful tool that may lower the proportion of chest pain patients who are admitted. Crit Pathw Cardiol. 2013;12(3):127–31.
Poldervaart JM, Reitsma JB, Backus BE, Koffijberg H, Veldkamp RF, ten Haaf ME, et al. Effect of using the HEART score in patients with chest pain in the emergency department. Ann Intern Med. 2017;166(10):689.
Leite L, Baptista R, Leitão J, Cochicho J, Breda F, Elvas L, et al. Chest pain in the emergency department: risk stratification with Manchester triage system and HEART score. BMC Cardiovasc Disord. 2015;15(1):48.
Six AJ, Cullen L, Backus BE, Greenslade J, Parsonage W, Aldous S, et al. The HEART score for the assessment of patients with chest pain in the emergency department: a multinational validation study. Crit Pathw Cardiol. 2013;12(3):121–6.
Fesmire FM, Martin EJ, Cao Y, Heath GW. Improving risk stratification in patients with chest pain: the Erlanger HEARTS3 score. Am J Emerg Med. 2012;30(9):1829–37.
Body R, De Wit K. Two troponins, one troponin, none…the dawn of troponin-less decision aids. CJEM. 2022;24(1):7–8.
Acknowledgements
We thank the staff at the College of Medicine Clinical Research Support Unit for their statistical support, and the rapid access clinics and Health Records Departments at both sites for their assistance in data retrieval.
Funding
This research project was funded by the College of Medicine Office of the Vice-Dean Research Dean’s Summer Research Project Fund and the Department of Emergency Medicine Chief’s Discretionary Funds.
Author information
Authors and Affiliations
Contributions
LM devised the study and supervised the project. LM, AL and LR submitted the project for ethics and operational approval and provided support during data collection and manuscript writing. AL reviewed ECG scoring and HEART scores given. LR obtained patient records from the rapid access clinics at each site, reviewed data abstraction, and provided statistical support. ACM and AM participated equally in data collection and manuscript writing. LR, AL, and LM provided primary manuscript revisions. PM performed the statistical analysis. GK, JO, JS and RZ provided research support during data collection and manuscript writing and revisions.
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Ethical approval
This project was approved by the University of Saskatchewan Biomedical Research Ethics Board (REB-1794).
Consent to participate
Waiver of consent granted by the University of Saskatchewan Biomedical Research Ethics Board.
Consent for publication
Waiver of consent granted by the University of Saskatchewan Biomedical Research Ethics Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moustapha, A., Mah, A.C., Roberts, L. et al. Can ED chest pain patients with intermediate HEART scores be managed as outpatients?. Can J Emerg Med 24, 770–779 (2022). https://doi.org/10.1007/s43678-022-00355-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00355-4