Abstract
Introduction
Myotomy is the gold standard treatment for achalasia, yet long-term failure rates approach 15%. Treatment options for recurrent dysphagia include pneumatic dilation (PD), laparoscopic redo myotomy, per oral endoscopic myotomy (POEM), or esophagectomy. We employ both PD and POEM as first-line treatment for these patients. We evaluated operative success and patient reported outcomes for patients who underwent PD or POEM for recurrent dysphagia after myotomy.
Methods
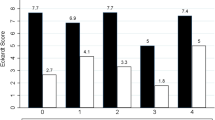
We identified patients with achalasia who underwent PD or POEM for recurrent dysphagia after previous myotomy within a foregut database at our institution between 2013 and 2021. Gastroesophageal Reflux Disease-Health-Related quality of Life (GERD-HRQL) and Eckardt scores, and overall change in each were compared across PD and POEM groups. Successful treatment of dysphagia was defined by Eckardt scores ≤ 3.
Results
103 patients underwent myotomy for achalasia. Of these, 19 (18%) had either PD or POEM for recurrent dysphagia. Nine were treated with PD and 10 with POEM. The mean change in Eckardt and GERD-HRQL scores did not differ between groups. 50% of the PD group and 67% of the POEM group had resolution of their dysphagia symptoms (p = 0.65). Mean procedure length was greater in the POEM group (267 vs 72 min, p < 0.01) as was mean length of stay (1.56 vs 0.3 days, p < 0.01). There was one adverse event after PD and three adverse events after POEM. After PD, 7 patients (70%) required additional procedures compared to four patients (44%) in the POEM group, consisting mostly of repeat PD.
Conclusion
Patients undergoing PD or POEM for recurrent dysphagia after myotomy have similar rates of dysphagia resolution and reflux symptoms. Patients undergoing PD enjoy a shorter length of stay and shorter procedure time but may require more subsequent procedures.

Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383:83–93
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313:1841–1852
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD, Society of American G, Endoscopic S (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311
Gaber CE, Eluri S, Cotton CC, Strassle PD, Farrell TM, Lund JL, Dellon ES (2022) Epidemiologic and economic burden of achalasia in the United States. Clin Gastroenterol Hepatol 20(342–352):e345
Costantino CL, Geller AD, Visenio MR, Morse CR, Rattner DW (2020) Outcomes of laparoscopic Heller myotomy for achalasia: 22-year experience. J Gastrointest Surg 24:1411–1416
Shea GE, Johnson MK, Venkatesh M, Jolles SA, Prout TM, Shada AL, Greenberg JA, Lidor AO, Funk LM (2020) Long-term dysphagia resolution following POEM versus Heller myotomy for achalasia patients. Surg Endosc 34:1704–1711
Doubova M, Gowing S, Robaidi H, Gilbert S, Maziak DE, Shamji FM, Sundaresan RS, Villeneuve PJ, Seely AJE (2021) Long-term symptom control after laparoscopic Heller myotomy and Dor fundoplication for achalasia. Ann Thorac Surg 111:1717–1723
Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG (2018) Laparoscopic heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg 267:451–460
Ortiz A, de Haro LF, Parrilla P, Lage A, Perez D, Munitiz V, Ruiz D, Molina J (2008) Very long-term objective evaluation of heller myotomy plus posterior partial fundoplication in patients with achalasia of the cardia. Ann Surg 247:258–264
Moonen A, Annese V, Belmans A, Bredenoord AJ, BruleydesVarannes S, Costantini M, Dousset B, Elizalde JI, Fumagalli U, Gaudric M, Merla A, Smout AJ, Tack J, Zaninotto G, Busch OR, Boeckxstaens GE (2016) Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 65:732–739
Nurczyk K, Patti MG (2020) Surgical management of achalasia. Ann Gastroenterol Surg 4:343–351
Ieong K, Brown A, Yang J, Zhang X, Altieri MS, Spaniolas K, Pryor AD (2022) The incidence of reintervention and reoperation following Heller myotomy across multiple indications. Surg Endosc 36:1619–1626
Gockel I, Junginger T, Eckardt VF (2007) Persistent and recurrent achalasia after Heller myotomy: analysis of different patterns and long-term results of reoperation. Arch Surg (Chicago, III: 1960) 142:1093–1097
Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Gurudu SR, Jamil LH, Jue TL, Kannadath BS, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Yang J, Wani S (2020) ASGE guideline on the management of achalasia. Gastrointest Endosc 91(213–227):e216
Huang Z, Cui Y, Li Y, Chen M, Xing X (2021) Peroral endoscopic myotomy for patients with achalasia with previous Heller myotomy: a systematic review and meta-analysis. Gastrointest Endosc 93(47–56):e45
Stewart RD, Hawel J, French D, Bethune D, Ellsmere J (2018) S093: pneumatic balloon dilation for palliation of recurrent symptoms of achalasia after esophagomyotomy. Surg Endosc 32:4017–4021
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, Consortium RE (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Eckardt VF, Aignherr C, Bernhard G (1992) Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology 103:1732–1738
Dorsey YC, Song EJ, Leiman DA (2021) Beyond the Eckardt Score: patient-reported outcomes measures in esophageal disorders. Curr Gastroenterol Rep 23:29
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, Swanstrom LL, Vassiliou MC (2014) Per-oral endoscopic myotomy white paper summary. Surg Endosc 28:2005–2019
(2021) Stata Statistical Software: Release 17. StataCorp LLC, College Station, TX
Capovilla G, Salvador R, Provenzano L, Valmasoni M, Moletta L, Pierobon ES, Merigliano S, Costantini M (2021) Laparoscopic revisional surgery after failed heller myotomy for esophageal achalasia: long-term outcome at a single tertiary center. J Gastrointest Surg 25:2208–2217
Smith KE, Saad AR, Hanna JP, Tran T, Jacobs J, Richter JE, Velanovich V (2020) Revisional surgery in patients with recurrent dysphagia after heller myotomy. J Gastrointest Surg 24:991–999
Veenstra BR, Goldberg RF, Bowers SP, Thomas M, Hinder RA, Smith CD (2016) Revisional surgery after failed esophagogastric myotomy for achalasia: successful esophageal preservation. Surg Endosc 30:1754–1761
Ngamruengphong S, Inoue H, Ujiki MB, Patel LY, Bapaye A, Desai PN, Dorwat S, Nakamura J, Hata Y, Balassone V, Onimaru M, Ponchon T, Pioche M, Roman S, Rivory J, Mion F, Garros A, Draganov PV, Perbtani Y, Abbas A, Pannu D, Yang D, Perretta S, Romanelli J, Desilets D, Hayee B, Haji A, Hajiyeva G, Ismail A, Chen YI, Bukhari M, Haito-Chavez Y, Kumbhari V, Saxena P, Talbot M, Chiu PW, Yip HC, Wong VW, Hernaez R, Maselli R, Repici A, Khashab MA (2017) Efficacy and safety of peroral endoscopic myotomy for treatment of achalasia after failed heller myotomy. Clin Gastroenterol Hepatol 15(1531–1537):e1533
Kamal F, Ismail MK, Khan MA, Lee-Smith W, Sharaiha RZ, Sharma S, McDonough S, Tariq R, Marella HK, Khan Z, Heda RP, Tombazzi C, Howden CW, Adler DG (2021) Efficacy and safety of peroral endoscopic myotomy in the management of recurrent achalasia after failed Heller myotomy: a systematic review and meta-analysis. Ann Gastroenterol 34:155–163
Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE (2013) Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg 217:598–605
Acknowledgements
We would like to thank Glen Leverson, PhD for his insightful comments and feedback.
Funding
Effort on this study and manuscript was made possible by a George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award from the American College of Surgeons and a VA Career Development Award to Dr. Funk (CDA 015-060). The views represented in this article represent those of the authors and not those of the DVA or the US Government.
Author information
Authors and Affiliations
Contributions
CZ, NT, AS contributed to the study design and data collection. All coauthors participated in the data interpretation and revisions. All coauthors approved the version to be published and agree to be accountable for all aspects of the work and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Disclosures
Luke Funk received funding for this study through a George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award from the American College of Surgeons and a VA Career Development Award. Christopher Zimmermann, Nate Torell, Anne Lidor, and Amber Shada have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zimmermann, C., Torell, N., Lidor, A. et al. Recurrent dysphagia after myotomy for achalasia: pneumatic dilation or POEM?. Surg Endosc 37, 4812–4817 (2023). https://doi.org/10.1007/s00464-022-09556-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09556-5