Abstract
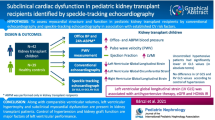
Transthoracic echocardiography is commonly used to identify structural and functional cardiac abnormalities that can be prevalent in childhood chronic kidney failure (KF). Left ventricular mass (LVM) increase is most frequently reported and may persist post-kidney transplant especially with hypertension and obesity. While systolic dysfunction is infrequently seen in childhood chronic KF, systolic strain identified by speckle tracking echocardiography has been frequently identified in dialysis and it can also persist post-transplant. Echocardiogram association with long-term outcomes has not been studied in childhood KF but there are many adult studies demonstrating associations between increased LVM, systolic dysfunction, strain, diastolic dysfunction, and cardiovascular events and mortality. There has been limited study of interventions to improve echocardiogram status. In childhood, improved blood pressure has been associated with better LVM, and conversion from hemodialysis to hemodiafiltration has been associated with better diastolic and systolic function. Whether long-term cardiac outcomes are also improved with these interventions is unclear. Echocardiography is a well-established technique, and regular use in childhood chronic KF seems justified. A case can be made to extend screening to include speckle tracking echocardiography and intradialytic studies in high-risk populations. Further longitudinal studies including these newer echocardiogram modalities, interventions, and long-term outcomes would help clarify recommendations for optimal use as a screening tool.
Similar content being viewed by others
Introduction
The mortality rate for children with chronic kidney failure (KF) is at least 30 times higher than their age-matched healthy peers [1]. Cardiovascular disease (CVD) is a leading cause of this excess mortality, which increases for those who survive into adulthood [2]. Even with transplantation and advances in dialysis care, CVD-associated mortality remains significant [3].
Prevention of cardiovascular (CV) events in chronic KF is a major challenge as CVD is often silent and a significant proportion of CV mortality is from sudden cardiac death [4]. A key focus of pediatric kidney research has been identification of early markers of CVD in order to understand natural history and risk factors, and to inform preventative strategies. Echocardiography has been used since the 1980s in pediatric KF research and clinical practice as a surrogate outcome measure of CV health. Its use can be described as a form of screening; however, protocols for use, and guidance on how echocardiography should inform treatment are limited.
Through this review, we provide a refresher of the natural history of CVD in chronic KF and associated structural and functional cardiac changes that can be identified with echocardiography. We then summarise established and new echocardiographic techniques, and finally we review the evidence for use of echocardiogram as a screening tool in the pediatric dialysis and transplant population. Studies of children with CKD are not included in this review.
The natural history of CVD in pediatric kidney failure
Chronic KF has been associated with all types of structural cardiac disease including myocardial fibrosis and hypertrophy [5], arteriosclerosis [6], myocardial capillary rarefaction [5], conduction system abnormalities [4], valve calcification [7], and coronary atherosclerosis [6]. In children with chronic KF, myocardial change, typically left ventricular (LV) mass increase is most commonly seen. This is thought to be an initial adaptive response to increased cardiac workload and pressure/volume overload [8]. Progression to LV hypertrophy (LVH) however can be maladaptive with potential functional consequence especially with higher cardiac workload demands [8]. There is a complex interplay of many factors that contribute to CVD processes, and in many patients these factors have been at play from earlier stages of chronic kidney disease (CKD), further increasing longer-term risk profile [9]. A summary of CVD risk factors in chronic KF is presented below.
Traditional risk factors
Hypertension is the most common CV risk factor present in children with chronic KF, with uncontrolled hypertension evident in 51% of children after 1 year of dialysis [10] and in 25% 5 years post-transplant [11]. Hypertension causes endothelial injury and arterial stiffness leading to an increase in peripheral vascular resistance and pressure load on the left ventricle [6]. Over time, this causes myocardial injury, ventricular hypertrophy, and remodelling. Hypertension is also a pro-atherogenic state [6].
Dyslipidaemia, another pro-atherogenic state, has been reported in 45% of the pediatric transplant population [12]. An increase in atherogenic lipoproteins is seen, with inhibition of antioxidant pathways. Pro-inflammatory effects contribute to endothelial dysfunction and vascular stiffness [13]. Disturbances in body mass index (BMI) are common in KF, with coronary artery calcification more prevalent with obesity and malnutrition [14, 15]. Metabolic syndrome is increasingly prevalent post-transplantation and this can contribute to vascular inflammation, arterial stiffness, and atheroma [16].
Kidney failure, uremic, and inflammatory risk factors
Chronic KF is a complex state of persistent low-grade inflammation [17]. Pro inflammatory cytokines are elevated, with C-reactive protein (CRP) associated with coronary calcification in children [18], and interleukin-6 (IL-6) and CRP associated with CV mortality in adults [19]. Dialysis is an independent exacerbator of inflammation by mechanisms including peritoneal dialysate and hemodialysis membrane bio-incompatibility, and catheter-associated infections [17]. Fluid overload has also recently been associated with markers of inflammation [20].
Elevated serum calcium, phosphorus, and parathyroid hormone (PTH) are all independently linked to increased risk of coronary artery calcification [18] and carotid intima media thickness (CIMT) [21] in children with chronic KF. Increased ventricular mass can be linked to cellular growth triggered by FGF23, as a result of impaired phosphate and vitamin D metabolism [22]. In addition, there are challenges with achieving an ideal balance of treatment, with overtreatment with activated vitamin D and calcium containing phosphate binders associated with CIMT [23] and coronary artery calcification [24].
Anaemia is a frequent complication of dialysis and reduced GFR and has been associated with LVH and diastolic dysfunction in several pediatric studies [21, 25, 26]. Cardiovascular complications of anaemia are believed to be due to a chronic increase in cardiac output, poor tissue perfusion, and reduced oxygen delivery to the myocardium [27].
Dialysis and mechanical risks
Dialysis is perhaps the most significant risk factor for CVD. Pre-emptive transplantation and reduced cumulative time on dialysis have been associated with improved survival [3, 28]. A multitude of inter-related factors are at play including exaggerated risks of traditional and uremic/inflammatory factors, and of course fluid overload. Risk is potentially most significant for the hemodialysis population, with extremes of volume overload and intra-dialytic hypotension associated with mortality in adults [29]. Temporary global or regional reduction in systolic myocardial function, called myocardial stunning, is seen frequently in children on conventional hemodialysis, and can be related to intradialytic hypotension with reduced coronary perfusion and changes in volume loading [30]. Repeated myocardial stunning may cause chronic injury, contributing in some circumstances to chronic systolic dysfunction [31].
Dialysis patients are at risk of pressure and volume overloaded cardiovascular states, both of which have been associated with increasing LV mass, hypertrophy, and functional changes including impaired ventricular relaxation (diastolic dysfunction) and ventricular contraction (systolic dysfunction). There is significant interdependence of hypertension and volume overload, although control of volume state may be the most important factor in reducing LV mass [32]. The geometry of LVH may give a clue as to the predominant risk state, with volume overload and ventricular dilatation leading to a more eccentric hypertrophy, and pressure overloaded systems characterised by a concentric hypertrophy [33]. Arterial stiffness identified by increased aortic pulse wave velocity (PWV) can contribute to this pressure overload. It is often described as a marker of vessel ageing, which is seen in children with KF [34]. With a lifetime of kidney replacement therapy ahead of them, these changes are significant.
Echocardiography techniques and limitations
Trans-thoracic echocardiography is the most widely used diagnostic modality available for structural and functional cardiac assessment. Conventional modes of echocardiography use two-dimensional (2D) assessments of structure and motion to assess myocardial wall thickness, wall mass, chamber size, and systolic function. Accurate assessment requires gating with an electrocardiogram to determine timing of systole and diastole. Integration of Doppler measures allows evaluation of pressure, velocity, valvular function, and diastolic/systolic function (including tissue Doppler imaging TDI). Newer methods such as strain imaging and three-dimensional (3D) echocardiography may provide more accurate assessments and early detection of sub-clinical systolic dysfunction [35]. Overall echocardiogram limitations include inter- and intra-observer variation, indirect derivation of some measurements, and system and resource considerations. Specific to KF, volume state dependence of some measures needs to be taken into consideration. A summary of echo modalities, clinical utility, and limitations is discussed below and further detail of commonly reported parameters in chronic KF publications is provided in Table 1.
Modalities
2-D echocardiography (2DE)
2-D echocardiography is the most commonly used modality and provides cross-sectional views for basic assessment of cardiac structure and function. Left ventricular ejection fraction (LVEF) is calculated by the biplane Simpson’s method using the formula (left ventricular end-diastolic volume − end-systolic volume)/end-diastolic volume in 2 planes (apical four chamber and apical two chamber) [39]. Systolic and diastolic ventricular volumes are measured by tracing the endocardial border of the ventricle, which is typically then divided into 20 disks (Fig. 1a). Due to the nature of the tracing, certain geometric assumptions are made, leading to potential inaccuracies in non-ellipsoid ventricles.
M-mode
Motion-mode or M-mode is a time gated view of structures along a single ultrasound line. It is generally used as a complementary tool in assessment of ventricular wall thickness, chamber dimension, and abnormal valvular movement. Measurements can be acquired in circumferential (short-axis) or longitudinal (long-axis) planes. Linear measurement of left ventricular end diastolic diameter (LVEDD) and left ventricular end systolic diameter (LVESD) are used to calculate fractional shortening (FS) as a measure of LV systolic function ((LVEDD − LVESD / LVEDD) × 100) [39]. However, due to the inter-observer variability and inability to detect regional wall motion abnormalities, M-mode is largely being phased out in favour of more robust and reproducible modalities such as multiplanar imaging, 2DE calculated ejection fraction, and functional analysis using strain.
3-D echocardiography (3DE)
3-D echocardiography obviates the need for geometric assumptions and provides more accurate measurements of ventricular volume and function than 2DE [39]. It is, however, currently limited by quality of image acquisition and time, and is reliant on technical capabilities of the software, and thus, it is not routinely integrated into echocardiographic assessments. Automated and artificial intelligence-optimised 3DE imaging packages can improve standardisation and optimise resource utilisation but are vendor-dependent and currently used on a limited basis. Cardiac magnetic resonance imaging (MRI) also provides 3D imaging and may become standard of care; however, there are safety considerations in KF including requirement for sedation in younger children, and when gadolinium contrast is required.
Doppler assessments
Doppler echocardiography allows assessment of velocity and direction of blood flow to provide precise hemodynamic evaluation of the heart. Doppler velocity data is used to derive pressure data using the Bernouilli equations to estimate systemic and pulmonary pressures. Data across valves is useful to gauge valvular function and ventricular diastolic function. For LV diastolic function, velocities are measured at the level of the mitral valve, with the E wave representing early diastolic flow (Fig. 1bi), and the A wave representing late diastolic flow or the flow during atrial contraction. LV filling pressure is most often expressed as the E/A ratio, with impaired ventricular relaxation and diastolic dysfunction often defined by E/A < 1. Continuous wave, pulsed wave (PWD), and colour Doppler are the main modalities utilised. Limitations with Doppler studies include underestimation of the gradient if the sound beam is not exactly parallel to jet. In addition, fast heart rates can make assessment of A and E waves difficult. Finally, volume status can influence some parameters (typically higher E/A ratio), thus standardisation of scanning in relation to dialysis schedules is important.
Tissue Doppler imaging
Tissue Doppler imaging (TDI) measures myocardial velocities in specific locations. Typically, pulsed wave TDI is used. Measurements include velocity data during early diastole (E′), late diastole (A′), and systole (S′). Peak measurements are most commonly undertaken at the LV free wall myocardium just below the mitral valve annulus (lateral), medial wall just at the top of the ventricular septum (medial), and at the right ventricular free wall just below the tricuspid valve annulus (RV). TDI assessment of mitral annular velocity (E′) (Fig. 1bii) is a validated measure of LV diastolic function correlating with invasive assessment on catheter, and is less pre-load dependent than Doppler mitral inflow velocity (E) [40]. As with conventional Doppler, in diastolic dysfunction, impaired relaxation will decrease E′ more than A′, and TDI E′/A′ is another measure of diastolic function. Conventional E to tissue Doppler E′ (E/E′) may be the most reliable and sensitive Doppler measure of diastolic dysfunction [41]. TDI can also be used to quantify regional and global systolic LV function (S′), and to measure strain. There may be limitations of TDI due to discrepancies in the beam angle and limitations in plane of assessment (assessment of radial and circumferential strain is limited), although inter and intra-observer reproducibility appears reasonable [42].
Speckle tracking echocardiography (STE)
Speckle tracking echocardiography (STE) tracks the motion of individual reflections within the myocardium to assess myocardial deformation and provides an assessment of strain (also known as strain imaging) during systole or diastole. Strain is associated with myocardial hypertrophy and fibrosis in human and animal studies [43, 44]. Microvascular dysfunction has also been associated with impaired strain [45]. Typically used with 2DE, STE can detect myocardial displacement along longitudinal, radial, and circumferential planes. Global longitudinal strain (GLS) is measured as the relative change of LV myocardium between end-diastole and end-systole, and should be a negative value (Fig. 1c). A less negative value is indicative of worse systolic LV function. GLS is a sensitive measure of systolic function and has recently been identified in adult KF as a more precise predictor of cardiovascular mortality than ejection fraction [46]. Regional strain can be assessed by STE and has been used to help define mechanical dyssynchrony [30]. Software can also be used to calculate speckle derived ventricular volumes and derive an ejection fraction [47]. Some of the limitations with STE include its dependency on 2D image quality and frame rates, and it remains volume dependent, especially for hemodialysis patients. STE however is non-angle dependent and is mostly reproduceable. Strain measures by STE (versus TDI) are often preferred for this reason, and also because STE is less time consuming. 3D STE is an emerging new technology that may overcome some of the inaccuracies of 2D STE but is not yet validated in the pediatric cohort [48].
Contrast enhanced echocardiography (CEE)
CEE has been recently approved for use in children in the USA. This technique uses intravenous microbubble contrast agents in conjunction with echocardiography, and is considered to improve resolution, with utility especially in obese patients [49]. Clear resolution to trace the endocardial border may provide more accurate LV function assessment, and may be more helpful in identifying perfusion associated regional wall dysfunction [49].
Stress echocardiography
2DE in conjunction with exercise- or drug- (e.g. dobutamine) induced myocardial work can be used to detect coronary artery disease through detection of regional wall abnormalities. It is rarely clinically used in children but in research has been shown to demonstrate that children with chronic KF on dialysis have reduced contractile reserve during exercise and dobutamine stress [8, 50]. These authors hypothesised that this may predict future systolic dysfunction and heart failure; however, long-term follow-up outcomes have not been determined to our knowledge.
Novel techniques
The cardiac work index (CWI) is a non-invasive assessment of strain and LV pressure. Strain data derived from STE is superimposed on population reference LV pressure measures at time of LV peak pressure, mitral valve opening, and closure. The derived LV pressure curve is then matched with the patient’s strain data to develop a pressure-strain loop. The area of the loop is the CWI [51]. CWI can accurately and independently predict mortality in an adult hemodialysis population, and may be superior to LVEF and GLS [52]. CWI has not been assessed in a pediatric KF population to our knowledge.
Pediatric echocardiography standards in kidney failure and reference range challenges
Wall thickness, chamber size, and functional assessment should form part of each echocardiogram assessment and there are published recommendations to guide this [39], as well as to standardise reporting [53].
Given the potential hemodynamic changes in chronic KF, echocardiogram standardisation can be a challenge [54]. Ideally, routine assessment of patients on dialysis should occur at rest, on an interdialytic day when close to or at ideal/target weight, and at target hemoglobin concentration. Ideal weight, however, can be difficult to assess and echocardiography may also be used to help define this. Inferior vena cava (IVC) parameters along with clinical correlation have been shown to accurately predict fluid status in dialysis patients with adult studies showing improved cardiac mechanics and left ventricular mass (LVM) with dry weights adjusted according to IVC diameter [55]. Additional data can be derived from echocardiograms performed during dialysis or in the immediate post-dialysis period [30, 56] and a number of methods incorporating time have been used to reduce the impact of volume status on echocardiogram measures. An example is the myocardial performance index (MPI), or Tei index. It is assessed using Doppler imaging and is defined as the sum of the isovolumic contraction and relaxation times divided by the ejection time [38]. It is considered a reliable parameter for global LV function assessment but is mainly used in a research capacity in children. Other echocardiogram confounders include age, gender, race, and body composition. To account for body composition, LVM is commonly indexed to body surface area (BSA) or height, and presented as the left ventricular mass index (LVMI). To compare with healthy reference populations, values in pediatric echocardiography have been recommended to be presented as Z-scores [39]. Given body composition issues in chronic KF, presentation of height or BSA-based Z-scores for LVM may be most accurate [57]. The most relevant reference intervals should be used which are best representative of one’s cohort, and in accordance with one’s vendor’s equipment. There may, however, still be challenges in finding the most appropriate reference for the individual given the substantial variability in the healthy population, particularly for LVM.
Echocardiogram patterns of relevance in chronic kidney failure
An increasing array of echocardiogram changes in chronic KF are now described. In many of these, associations with cardiac events and mortality have been reported in adult populations. Longer outcome studies in pediatrics are required. Detailed definitions of more commonly described markers in clinical and research use are provided in Table 1.
Echocardiogram studies in pediatric kidney failure
There are countless observational studies of prevalence and risk of echocardiogram changes in pediatric chronic KF. Many incorporate control populations to demonstrate significantly worse LVM, diastolic and systolic function [21, 41, 58,59,60,61]. Each publication must be interrogated closely. Demographic factors such as duration of dialysis can significantly impact findings, and definitions of abnormal values vary. Table 2 presents key studies evaluating children with chronic KF, aiming to highlight the prevalence of echocardiogram abnormalities, multivariable analysis-derived risk factors, and follow-up of echocardiogram changes over time.
LVM/LVH is the most commonly studied echocardiogram parameter, with some studies also assessing LVM influence on function, demonstrating a correlation with worse diastolic [21, 59], and systolic [66] function. Hypertension has been consistently identified as a key risk factor for LVH in dialysis [8, 25, 58, 63, 64, 70] and transplant [70, 71] populations, with overweight/obese BMI also associated with LVH in dialysis [25] and transplant populations [61, 71]. LVM risk appears to increase from CKD to dialysis in children, although longitudinal studies are not available. In both peritoneal dialysis (PD) [65] and hemodialysis (HD) [8, 25] volume-related factors, anaemia [25, 58, 65] and hyperparathyroidism [21] are key risks. Where these are carefully managed, LVM and LV geometry can improve [57]. With transplantation, some regression in LVM can also be seen [72], although hypertension and metabolic risks can lead to persistent changes, or deterioration over time [71, 73]. A recent study has correlated LVM in children on dialysis with pulse wave velocity (PWV), a marker of vascular stiffness [74]. A direct causal relationship between PWV and LVM/LVH has not been established, and the correlation may simply reflect that hypertension is a common risk factor. CIMT is also associated with LVH in PD patients [65], again suggesting the presence of a common risk state. In this publication, inflammation was postulated as important given that both LVH and CIMT were significantly associated with CRP [65].
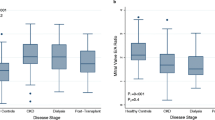
Global LV systolic function as measured by conventional echo-based LVEF/FS is mostly preserved in childhood chronic KF [35, 75]. During HD sessions, however, regional myocardial systolic dysfunction assessed by SF% (stunning) is a common finding [30]. In adults stunning has been demonstrated to progress to fixed regional systolic dysfunction and global reduction in LVEF by 12 months [31] and is associated with 12-month mortality [76]. Impaired GLS measured by STE has been demonstrated in childhood chronic KF in the absence of conventional echocardiography measures of systolic dysfunction [56]. In adult dialysis patients, GLS is associated with CV mortality independent of age and conventionally measured EF [43]. The HD population appears to be most at risk, especially if assessed during or immediately following a HD session [35, 47, 56, 77] and if there are more significant falls in systolic blood pressure or higher ultrafiltration volumes [56, 77]. Segmental differences in LV strain can also be seen at this time [47] including where measured by the asynchrony index (Table 1) [77]. This is a marker of LV mechanical dyssynchrony which is where there are regional differences in timing of ventricular contraction and relaxation. The asynchrony index is associated with ventricular arrythmias and sudden cardiac death in adult dialysis patients independent of LVEF [78]. A recent study using 2D STE post-hemodialysis has shown impaired LVEF derived by STE versus normal LVEF by conventional echocardiogram in children, providing further evidence of the sensitivity of STE [47]. Strain by STE or TDI has been shown in some pediatric transplant cohorts to be significantly worse than controls [35, 59], and has been associated with hypertension, metabolic syndrome, obesity, dyslipidaemia, lower EGFR, and past HD (versus PD or pre-emptive transplant) [61]. Longitudinal patient assessment has demonstrated that GLS can improve with transplantation [75], although it remains significantly worse versus controls [61]. Mitsnefes et al. have demonstrated evidence of LV hypercontractility in dialysis [8] and transplant patients [79]. In dialysis, the contractile reserve in exercise was reduced compared with controls, whereas in transplant patients the reserve was maintained. It was postulated that this could suggest an adaptive response perhaps mediated by sympathetic overactivity, and that over the long-term, this may be disadvantageous. To date, however, associated long-term outcomes have not been assessed to our knowledge. Kim et al. identified in the post-transplant cohort poorer LV performance, defined by the Tei index, and worse GLS by TDI, in the setting of increased FS and EF, and that this was associated with a longer time on dialysis prior to transplant [59]. Again, no longer-term follow-up data is available.
LV diastolic function can be impaired in both dialysis and transplantation [21, 41, 59, 60, 80]. Most studies evaluate this as a continuous parameter using the ratios E/A, E′/A′, or E/E′, although some define specific criteria for diastolic dysfunction [41, 60, 64, 66]. TDI measures of diastolic function may be more sensitive than PWD [41]. Duration of dialysis has been associated with markers of LV stiffness [80], and diastolic dysfunction (DD) may persist post-transplant [59, 60, 75]. DD has been associated with LVH/LVMI in HD [66] and transplant [67, 79]; however, this is not a consistent finding [41, 73], and could reflect how LVMI or DD was defined/measured, or other risk factors for DD in the studied population. Markers of volume overload [65], and hyperparathyroidism [21] have been associated with worse diastolic function. Risk post-transplant may be independent of hypertension [41, 73]. In adults, DD measured by E/E′ ratio has been associated with mortality [81]. In HD, left atrial strain (LAS) measures may be an even more sensitive measure of DD and cardiac events [82]. LAS has recently been demonstrated to worsen during HD in children [56].
Right heart changes are infrequently reported in childhood chronic KF, although these are still an important part of standard echocardiogram assessment. Right heart geometry has been reported to change in adolescents on HD, especially in the presence of an arterio-venous fistula [83], with increased right atrial and right ventricular (RV) free wall thickness and reduced RV volumes reported. This may be due to an increase in venous return.
Ascending aortic dilatation appears to be somewhat of a novel finding for children (versus adults) with chronic KF [68, 84, 85], and it is also seen in childhood CKD [86]. Poor nutrition may be an important risk factor [86]. Pre-emptive transplantation may be protective, and there appears to be an association with post-transplant hypertension [85]. We were unable to find publications with aortic measurements reported in adult chronic KF populations.
Current guidelines for echocardiography use in kidney failure
Guidelines that incorporate routine echocardiography assessment of chronic kidney failure patients are listed in Table 3. These have mainly focused on pre-transplantation screening of adult patients to determine suitability, as cardiac mortality in the first few months post-transplant can be high [87]. Identification of ischaemic heart disease (IHD) via non-invasive tests including stress echocardiograms is the predominant focus, although this is controversial, especially for asymptomatic patients. The American Society of Transplantation guidelines incorporate LVEF into their risk stratification for progressing to non-invasive IHD screening in transplant candidates, with routine echocardiogram screening suggested for those who are identified at risk based on clinical screening, X-ray and ECG [88]. The NKK-KDOQI guidelines are the only guidelines that recommend more regular echocardiography in dialysis [89]. In addition, these are the only guidelines that reference children, in whom a resting echocardiogram is recommended in the first 3 months following dialysis initiation [89]. No guidelines address routine echocardiogram screening in transplant recipients.
Should routine echocardiogram screening be recommended in pediatric kidney failure?
While prevalence of echocardiogram abnormalities is significant across childhood dialysis and transplant populations, current pediatric recommendations for echocardiogram screening in chronic KF are limited. A key screening test principle is that screening followed by an intervention should reduce clinical events. Currently, there are no trials assessing whether echocardiogram triggered interventions improve CV events. Physiologic principles, longitudinal studies, and multivariable analyses, including adult studies and those assessing echocardiogram outcomes, do, however, suggest that some interventions could be of benefit. For example, improved volume state and blood pressure in children is associated with better LVM in PD and HD [25, 63]. In adults, more frequent HD has been associated with reduced myocardial stunning [92], and in longitudinal studies, LVH regression with improved systolic function [93]. Shroff et al. demonstrated an increase in LVMI over 12 months for children on HD, with no significant change seen for patients on hemodiafiltration (HDF) [25], and Fadel identified an improvement in diastolic and systolic function for children converted to online-HDF with associated decrease in CRP [69]. In adults, some studies have shown improved survival with HDF [94]. Low hemoglobin has been associated with LVMI/LVH in childhood dialysis [25, 58], and in adults, correction of anaemia has been associated with regression of LVH [95]. Hemodialysate cooling was associated with less myocardial stunning in a randomised crossover trial in adults [96], and in a cross-sectional study of adults, stunning was rare in PD versus HD [97].
One could argue that many echocardiogram abnormalities are associated with volume overload or hypertension, and that a screening echocardiogram should not be required to identify these states. Regular echocardiogram screening to identify subclinical and potentially reversible end-organ damage could be of benefit, however, to prompt an earlier change in management and a more complete evaluation of patient CV risk and therapy options. This could be individualised with screening further extended or increased in frequency according to local echocardiogram access or baseline suspected risk. For example, HD patients could be screened during dialysis or immediately post-dialysis to identify stunning or strain. Given that stunning has been associated in adults with irreversible systolic dysfunction and mortality by 12 months [31], and there are indicators that strain is associated with myocardial fibrosis, any accessible intervention that has some level of evidence and is without harm should be considered. For example, change in modality to PD may be associated with less cumulative risk of stunning/strain, and more frequent HD or hemodialysate cooling may reduce stunning. Transplantation may also reduce these risks, with some evidence that impaired strain can be reversed [61]. Post-transplant, CV screening recommendations include metabolic and BP screening [98, 99], with ambulatory BP screening recommended due to the higher risk of masked hypertension in this population [99]. Of note, based on the American Association of Pediatrics (AAP) hypertension guidelines, any child with hypertension and kidney disease should have a yearly echocardiogram [99].
Minimum recommended standards for pediatric echocardiography have been published by the American Society of Echocardiography [39, 53]. These standards include all the important assessments from a chronic KF perspective, including measures of the left ventricle and aorta, an assessment of systolic function, and Doppler-based diastolic function. Given that longitudinal chronic KF studies identify evolving echocardiogram changes within 12 months [25, 61, 69, 70], a minimum of annual frequency of echocardiogram screening seems appropriate but can be adjusted according to findings and risk factors.
Conclusions
Given future lifelong exaggerated CV risks in childhood chronic KF, and the complexities of these risk states, it is our opinion that regular assessment of CV risk factors and subclinical CV health is warranted during dialysis, pre- and post-transplant. Annual echocardiography, even with minimum standard assessment, is well-placed to help screen overall cardiac health. Further extended screening using newer modalities such as STE could be considered dependent on baseline suspected or known CV risk status. Echocardiography is a well-established technique which does not involve risk or significant time commitment for patients, and also provides important functional data. Further long-term research and interventional studies would help further clarify the specific utility of echocardiogram screening in the childhood chronic KF population.
References
McDonald SP, Craig JC (2004) Long-term survival of children with end-stage renal disease. N Engl J Med 350:2654–2662. https://doi.org/10.1056/NEJMoa031643
Parekh RS, Carroll CE, Wolfe RA, Port FK (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:91–197. https://doi.org/10.1067/mpd.2002.125910
Meier-Kriesche HU, Schold JD, Srinivas TR, Reed A, Kaplan B (2004) Kidney transplantation halts cardiovascular disease progression in patients with end-stage renal disease. Am J Transplant 4:1662–1668. https://doi.org/10.1111/j.1600-6143.2004.00573.x
Genovesi S, Boriani G, Covic A, Vernooij RWM, Combe C, Burlacu A, Davenport A, Kanbay M, Kirmizis D, Schneditz D, van der Sande F, Basile C (2021) Sudden cardiac death in dialysis patients: different causes and management strategies. Nephrol Dial Transplant 36:396–405. https://doi.org/10.1093/ndt/gfz182
Amann K, Rychlík I, Miltenberger-Milteny G, Ritz E (1998) Left ventricular hypertrophy in renal failure. Kidney Int Suppl 68:S78–S85. https://doi.org/10.1046/j.1523-1755.1998.06818.x
London GM (2000) Alterations of arterial function in end-stage renal disease. Nephron 84:111–118. https://doi.org/10.1159/000045557
Rong S, Qiu X, Jin X, Shang M, Huang Y, Tang Z, Yuan W (2018) Risk factors for heart valve calcification in chronic kidney disease. Medicine (Baltimore) 97:e9804. https://doi.org/10.1097/md.0000000000009804
Mitsnefes MM, Kimball TR, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2003) Left ventricular mass and systolic performance in pediatric patients with chronic renal failure. Circulation 107:864–868. https://doi.org/10.1161/01.cir.0000049744.23613.69
Mitsnefes MM (2021) Cardiovascular disease risk factors in chronic kidney disease in children. Semin Nephrol 41:434–438. https://doi.org/10.1016/j.semnephrol.2021.09.005
Mitsnefes M, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Am J Kidney Dis 45:309–315. https://doi.org/10.1053/j.ajkd.2004.11.006
Sinha MD, Kerecuk L, Gilg J, Reid CJ (2012) Systemic arterial hypertension in children following renal transplantation: prevalence and risk factors. Nephrol Dial Transplant 27:3359–3368. https://doi.org/10.1093/ndt/gfr804
Silverstein DM (2004) Risk factors for cardiovascular disease in pediatric renal transplant recipients. Pediatr Transplant 8:386–393. https://doi.org/10.1111/j.1399-3046.2004.00105.x
Shroff R, Speer T, Colin S, Charakida M, Zewinger S, Staels B, Chinetti-Gbaguidi G, Hettrich I, Rohrer L, O'Neill F, McLoughlin E, Long D, Shanahan CM, Landmesser U, Fliser D, Deanfield JE (2014) HDL in children with CKD promotes endothelial dysfunction and an abnormal vascular phenotype. J Am Soc Nephrol 25:2658–2668. https://doi.org/10.1681/asn.2013111212
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483. https://doi.org/10.1056/nejm200005183422003
Srivaths PR, Silverstein DM, Leung J, Krishnamurthy R, Goldstein SL (2010) Malnutrition-inflammation-coronary calcification in pediatric patients receiving chronic hemodialysis. Hemodial Int 14:263–269. https://doi.org/10.1111/j.1542-4758.2010.00442.x
Paik JK, Kim M, Kwak JH, Lee EK, Lee SH, Lee JH (2013) Increased arterial stiffness in subjects with impaired fasting glucose. J Diabetes Complications 27:224–228. https://doi.org/10.1016/j.jdiacomp.2012.10.012
Cobo G, Lindholm B, Stenvinkel P (2018) Chronic inflammation in end-stage renal disease and dialysis. Nephrol Dial Transplant 33:iii35–iii40. https://doi.org/10.1093/ndt/gfy175
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105. https://doi.org/10.1161/01.cir.0000020222.63035.c0
Panichi V, Rizza GM, Paoletti S, Bigazzi R, Aloisi M, Barsotti G, Rindi P, Donati G, Antonelli A, Panicucci E, Tripepi G, Tetta C, Palla R (2008) Chronic inflammation and mortality in haemodialysis: effect of different renal replacement therapies. Results from the RISCAVID study. Nephrol Dial Transplant 23:2337–2343. https://doi.org/10.1093/ndt/gfm951
Dekker MJE, van der Sande FM, van den Berghe F, Leunissen KML, Kooman JP (2018) Fluid overload and inflammation axis. Blood Purif 45:159–165. https://doi.org/10.1159/000485153
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2796–2803. https://doi.org/10.1681/asn.2005030291
Stevens KK, McQuarrie EP, Sands W, Hillyard DZ, Patel RK, Mark PB, Jardine AG (2011) Fibroblast growth factor 23 predicts left ventricular mass and induces cell adhesion molecule formation. Int J Nephrol 2011:297070. https://doi.org/10.4061/2011/297070
Litwin M, Wühl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Tröger J, Mehls O, Schaefer F (2005) Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16:1494–1500. https://doi.org/10.1681/asn.2004110932
Civilibal M, Caliskan S, Adaletli I, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Kuruoglu S, Arisoy N (2006) Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol 21:1426–1433. https://doi.org/10.1007/s00467-006-0159-6
Shroff R, Smith C, Ranchin B, Bayazit AK, Stefanidis CJ, Askiti V, Azukaitis K, Canpolat N, Ağbaş A, Aitkenhead H, Anarat A, Aoun B, Aofolaju D, Bakkaloglu SA, Bhowruth D, Borzych-Dużałka D, Bulut IK, Büscher R, Deanfield J, Dempster C, Duzova A, Habbig S, Hayes W, Hegde S, Krid S, Licht C, Litwin M, Mayes M, Mir S, Nemec R, Obrycki L, Paglialonga F, Picca S, Samaille C, Shenoy M, Sinha MD, Spasojevic B, Stronach L, Vidal E, Vondrák K, Yilmaz A, Zaloszyc A, Fischbach M, Schmitt CP, Schaefer F (2019) Effects of hemodiafiltration versus conventional hemodialysis in children with ESKD: the HDF, heart and height study. J Am Soc Nephrol 30:678–691. https://doi.org/10.1681/asn.2018100990
Yu JJ, Jun HO, Shin EJ, Baek JS, Lee JH, Kim YH, Park YS, Ko JK (2018) Factors associated with reduction of left ventricular mass in children on peritoneal dialysis. Nephrology (Carlton) 23:338–344. https://doi.org/10.1111/nep.13033
Radhakrishnan A, Pickup LC, Price AM, Law JP, McGee KC, Fabritz L, Senior R, Steeds RP, Ferro CJ, Townend JN (2021) Coronary microvascular dysfunction is associated with degree of anaemia in end-stage renal disease. BMC Cardiovasc Disord 21:211. https://doi.org/10.1186/s12872-021-02025-2
Amaral S, Sayed BA, Kutner N, Patzer RE (2016) Preemptive kidney transplantation is associated with survival benefits among pediatric patients with end-stage renal disease. Kidney Int 90:1100–1108. https://doi.org/10.1016/j.kint.2016.07.028
Chou JA, Streja E, Nguyen DV, Rhee CM, Obi Y, Inrig JK, Amin A, Kovesdy CP, Sim JJ, Kalantar-Zadeh K (2018) Intradialytic hypotension, blood pressure changes and mortality risk in incident hemodialysis patients. Nephrol Dial Transplant 33:149–159. https://doi.org/10.1093/ndt/gfx037
Hothi DK, Rees L, Marek J, Burton J, McIntyre CW (2009) Pediatric myocardial stunning underscores the cardiac toxicity of conventional hemodialysis treatments. Clin J Am Soc Nephrol 4:790–797. https://doi.org/10.2215/cjn.05921108
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced repetitive myocardial injury results in global and segmental reduction in systolic cardiac function. Clin J Am Soc Nephrol 4:1925–1931. https://doi.org/10.2215/cjn.04470709
Georgianos PI, Agarwal R (2015) Relative importance of aortic stiffness and volume as predictors of treatment-induced improvement in left ventricular mass index in dialysis. PLoS One 10:e0135457. https://doi.org/10.1371/journal.pone.0135457
Gaasch WH, Zile MR (2011) Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 58:1733–1740. https://doi.org/10.1016/j.jacc.2011.07.022
Shroff RC, Donald AE, Hiorns MP, Watson A, Feather S, Milford D, Ellins EA, Storry C, Ridout D, Deanfield J, Rees L (2007) Mineral metabolism and vascular damage in children on dialysis. J Am Soc Nephrol 18:2996–3003. https://doi.org/10.1681/asn.2006121397
van Huis M, Schoenmaker NJ, Groothoff JW, van der Lee JH, van Dyk M, Gewillig M, Koster L, Tanke R, Lilien M, Blom NA, Mertens L, Kuipers IM (2016) Impaired longitudinal deformation measured by speckle-tracking echocardiography in children with end-stage renal disease. Pediatr Nephrol 31:1499–1508. https://doi.org/10.1007/s00467-016-3362-0
Foster BJ, Khoury PR, Kimball TR, Mackie AS, Mitsnefes M (2016) New reference centiles for left ventricular mass relative to lean body mass in children. J Am Soc Echocardiogr 29:441-447.e442. https://doi.org/10.1016/j.echo.2015.12.011
Foster BJ, Mackie AS, Mitsnefes M, Ali H, Mamber S, Colan SD (2008) A novel method of expressing left ventricular mass relative to body size in children. Circulation 117:2769–2775. https://doi.org/10.1161/circulationaha.107.741157
Tei C (1995) New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol 26:135–136
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK, Lai WW, Geva T (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23:465–495. https://doi.org/10.1016/j.echo.2010.03.019 (quiz 576–577)
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW (1997) J Am Coll Cardiol 30:474–480. https://doi.org/10.1016/s0735-1097(97)88335-0
Schoenmaker NJ, Kuipers IM, van der Lee JH, Tromp WF, van Dyck M, Gewillig M, Blom NA, Groothoff JW (2014) Diastolic dysfunction measured by tissue Doppler imaging in children with end-stage renal disease: a report of the RICH-Q study. Cardiol Young 24:236–244. https://doi.org/10.1017/s1047951113000188
Eidem BW, McMahon CJ, Cohen RR, Wu J, Finkelshteyn I, Kovalchin JP, Ayres NA, Bezold LI, O'Brian Smith E, Pignatelli RH (2004) Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr 17:212–221. https://doi.org/10.1016/j.echo.2003.12.005
Kramann R, Erpenbeck J, Schneider RK, Röhl AB, Hein M, Brandenburg VM, van Diepen M, Dekker F, Marx N, Floege J, Becker M, Schlieper G (2014) Speckle tracking echocardiography detects uremic cardiomyopathy early and predicts cardiovascular mortality in ESRD. J Am Soc Nephrol 25:2351–2365. https://doi.org/10.1681/asn.2013070734
Krämer J, Niemann M, Liu D, Hu K, Machann W, Beer M, Wanner C, Ertl G, Weidemann F (2013) Two-dimensional speckle tracking as a non-invasive tool for identification of myocardial fibrosis in Fabry disease. Eur Heart J 34:1587–1596. https://doi.org/10.1093/eurheartj/eht098
Dubin RF, Guajardo I, Ayer A, Mills C, Donovan C, Beussink L, Scherzer R, Ganz P, Shah SJ (2016) Associations of macro- and microvascular endothelial dysfunction with subclinical ventricular dysfunction in end-stage renal disease. Hypertension 68:913–920. https://doi.org/10.1161/hypertensionaha.116.07489
Terhuerne J, van Diepen M, Kramann R, Erpenbeck J, Dekker F, Marx N, Floege J, Becker M, Schlieper G (2021) Speckle-tracking echocardiography in comparison with ejection fraction for prediction of cardiovascular mortality in patients with end-stage renal disease. Clin Kidney J 14:1579–1585. https://doi.org/10.1093/ckj/sfaa161
Rakha S, Hafez M, Bakr A, Hamdy N (2020) Changes of cardiac functions after hemodialysis session in pediatric patients with end-stage renal disease: conventional echocardiography and two-dimensional speckle tracking study. Pediatr Nephrol 35:861–870. https://doi.org/10.1007/s00467-019-04460-y
Muraru D, Niero A, Rodriguez-Zanella H, Cherata D, Badano L (2018) Three-dimensional speckle-tracking echocardiography: benefits and limitations of integrating myocardial mechanics with three-dimensional imaging. Cardiovasc Diagn Ther 8:101–117. https://doi.org/10.21037/cdt.2017.06.01
Kutty S, Biko DM, Goldberg AB, Quartermain MD, Feinstein SB (2021) Contrast-enhanced ultrasound in pediatric echocardiography. Pediatr Radiol 51:2408–2417. https://doi.org/10.1007/s00247-021-05119-3
Mese T, Guven B, Yilmazer MM, Serdaroglu E, Tavli V, Haydar A, Bak M (2010) Contractility reserve in children undergoing dialysis by dobutamine stress echocardiography. Pediatr Cardiol 31:937–943. https://doi.org/10.1007/s00246-010-9721-x
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, Haugaa KH, Opdahl A, Fjeld JG, Gjesdal O, Edvardsen T, Smiseth OA (2012) A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J 33:724–733. https://doi.org/10.1093/eurheartj/ehs016
Chen KW, Hsieh WT, Huang CY, Huang CC, Liang HY, Wang GJ (2021) Estimated left ventricular pressure-myocardial strain loop as an index of cardiac work predicts all-cause mortality in patients receiving regular hemodialysis. J Diabetes Complications 35:107890. https://doi.org/10.1016/j.jdiacomp.2021.107890
Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, Pignatelli RH, Rychik J (2006) Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr 19:1413–1430. https://doi.org/10.1016/j.echo.2006.09.001
Ie EH, Vletter WB, ten Cate FJ, Nette RW, Weimar W, Roelandt JR, Zietse R (2003) Preload dependence of new Doppler techniques limits their utility for left ventricular diastolic function assessment in hemodialysis patients. J Am Soc Nephrol 14:1858–1862. https://doi.org/10.1097/01.asn.0000072745.94551.fc
Hirayama S, Ando Y, Sudo Y, Asano Y (2002) Improvement of cardiac function by dry weight optimization based on interdialysis inferior vena caval diameter. ASAIO J 48:320–325. https://doi.org/10.1097/00002480-200205000-00020
Doan TT, Srivaths P, Liu A, Kevin Wilkes J, Idrovo A, Akcan-Arikan A, Swartz S, Geer J, Altman CA, Ayres NA, Loar RW, Pignatelli R (2021) Left ventricular strain and left atrial strain are impaired during hemodialysis in children. Int J Cardiovasc Imaging 37:3489–3497. https://doi.org/10.1007/s10554-021-02350-9
Melhem N, Savis A, Wheatley A, Copeman H, Willmott K, Reid CJD, Simpson J, Sinha MD (2019) Improved blood pressure and left ventricular remodelling in children on chronic intermittent haemodialysis: a longitudinal study. Pediatr Nephrol 34:1811–1820. https://doi.org/10.1007/s00467-019-04272-0
Civilibal M, Caliskan S, Oflaz H, Sever L, Candan C, Canpolat N, Kasapcopur O, Bugra Z, Arisoy N (2007) Traditional and “new” cardiovascular risk markers and factors in pediatric dialysis patients. Pediatr Nephrol 22:1021–1029. https://doi.org/10.1007/s00467-007-0451-0
Kim GB, Kwon BS, Kang HG, Ha JW, Ha IS, Noh CI, Choi JY, Kim SJ, Yun YS, Bae EJ (2009) Cardiac dysfunction after renal transplantation; incomplete resolution in pediatric population. Transplantation 87:1737–1743. https://doi.org/10.1097/TP.0b013e3181a63f2f
Lindblad YT, Axelsson J, Balzano R, Vavilis G, Chromek M, Celsi G, Bárány P(2013) Left ventricular diastolic dysfunction by tissue Doppler echocardiography in pediatric chronic kidney disease. Pediatr Nephrol 28:2003–2013. https://doi.org/10.1007/s00467-013-2504-x
Sgambat K, Clauss S, Lei KY, Song J, Rahaman SO, Lasota M, Moudgil A(2018) Effects of obesity and metabolic syndrome on cardiovascular outcomes in pediatric kidney transplant recipients: a longitudinal study. Pediatr Nephrol 33:1419–1428. https://doi.org/10.1007/s00467-017-3860-8
Mitsnefes MM, Daniels SR, Schwartz SM, Meyer RA, Khoury P, Strife CF (2000) Severe left ventricular hypertrophy in pediatric dialysis: prevalence and predictors. Pediatr Nephrol 14:898–902. https://doi.org/10.1007/s004670000303
Mitsnefes MM, Daniels SR, Schwartz SM, Khoury P, Strife CF (2001) Changes in left ventricular mass in children and adolescents during chronic dialysis. Pediatr Nephrol 16:318–323. https://doi.org/10.1007/s004670000557
Gruppen MP, Groothoff JW, Prins M, van der Wouw P, Offringa M, Bos WJ, Davin JC, Heymans HS (2003) Cardiac disease in young adult patients with end-stage renal disease since childhood: a Dutch cohort study. Kidney Int 63:1058–1065. https://doi.org/10.1046/j.1523-1755.2003.00814.x
Bakkaloglu SA, Saygili A, Sever L, Noyan A, Akman S, Ekim M, Aksu N, Doganay B, Yildiz N, Duzova A, Soylu A, Alpay H, Sonmez F, Civilibal M, Erdem S, Kardelen F (2009) Assessment of cardiovascular risk in paediatric peritoneal dialysis patients: a Turkish Pediatric Peritoneal Dialysis Study Group (TUPEPD) report. Nephrol Dial Transplant 24:3525–3532. https://doi.org/10.1093/ndt/gfp297
Shamszad P, Slesnick TC, Smith EO, Taylor MD, Feig DI (2012) Association between left ventricular mass index and cardiac function in pediatric dialysis patients. Pediatr Nephrol 27:835–841. https://doi.org/10.1007/s00467-011-2060-1
Hirth A, Edwards NC, Greve G, Tangeraas T, Gerdts E, Lenes K, Norgård G (2012) Left ventricular function in children and adults after renal transplantation in childhood. Pediatr Nephrol 27:1565–1574. https://doi.org/10.1007/s00467-012-2167-z
Kaddourah A, Uthup S, Madueme P, O'Rourke M, Hooper DK, Taylor MD, Colan SD, Jefferies JL, Rao MB, Goebel J (2015) Prevalence and predictors of aortic dilation as a novel cardiovascular complication in children with end-stage renal disease. Clin Nephrol 83:262–271. https://doi.org/10.5414/cn108489
Fadel FI, Makar SH, Zekri H, Ahmed DH, Aon AH (2015) The effect of on-line hemodiafiltration on improving the cardiovascular function parameters in children on regular dialysis. Saudi J Kidney Dis Transpl 26:39–46. https://doi.org/10.4103/1319-2442.148731
Mitsnefes MM, Schwartz SM, Daniels SR, Kimball TR, Khoury P, Strife CF (2001) Changes in left ventricular mass index in children and adolescents after renal transplantation. Pediatr Transplant 5:279–284. https://doi.org/10.1034/j.1399-3046.2001.005004279.x
Hamdani G, Nehus EJ, Hanevold CD, Sebestyen Van Sickle J, Woroniecki R, Wenderfer SE, Hooper DK, Blowey D, Wilson A, Warady BA, Mitsnefes MM (2017) Ambulatory blood pressure, left ventricular hypertrophy, and allograft function in children and young adults after kidney transplantation. Transplantation 101:150–156. https://doi.org/10.1097/tp.0000000000001087
Becker-Cohen R, Nir A, Ben-Shalom E, Rinat C, Feinstein S, Farber B, Frishberg Y (2008) Improved left ventricular mass index in children after renal transplantation. Pediatr Nephrol 23:1545–1550. https://doi.org/10.1007/s00467-008-0855-5
Basiratnia M, Esteghamati M, Ajami GH, Amoozgar H, Cheriki C, Soltani M, Derakhshan A, Fallahzadeh MH (2011) Blood pressure profile in renal transplant recipients and its relation to diastolic function: tissue Doppler echocardiographic study. Pediatr Nephrol 26:449–457. https://doi.org/10.1007/s00467-010-1724-6
Filip C, Cirstoveanu C, Bizubac M, Berghea EC, Căpitănescu A, Bălgrădean M, Pavelescu C, Nicolescu A, Ionescu MD (2021) Pulse wave velocity as a marker of vascular dysfunction and its correlation with cardiac disease in children with end-stage renal disease (ESRD). Diagnostics (Basel) 12:71. https://doi.org/10.3390/diagnostics12010071
Rumman RK, Ramroop R, Chanchlani R, Ghany M, Hebert D, Harvey EA, Parekh RS, Mertens L, Grattan M (2017) Longitudinal assessment of myocardial function in childhood chronic kidney disease, during dialysis, and following kidney transplantation. Pediatr Nephrol 32:1401–1410. https://doi.org/10.1007/s00467-017-3622-7
Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol 4:914–920. https://doi.org/10.2215/cjn.03900808
Hothi DK, Rees L, McIntyre CW, Marek J (2013) Hemodialysis-induced acute myocardial dyssynchronous impairment in children. Nephron Clin Pract 123:83–92. https://doi.org/10.1159/000351984
Hensen LCR, Goossens K, Podlesnikar T, Rotmans JI, Jukema JW, Delgado V, Bax JJ (2018) Left ventricular mechanical dispersion and global longitudinal strain and ventricular arrhythmias in predialysis and dialysis patients. J Am Soc Echocardiogr 31:777–783. https://doi.org/10.1016/j.echo.2018.01.010
Mitsnefes MM, Kimball TR, Border WL, Witt SA, Glascock BJ, Khoury PR et al (2004) Abnormal cardiac function in children after renal transplantation. Am J Kidney Dis 43:721–726. https://doi.org/10.1053/j.ajkd.2003.12.033
Choi AW, Fong NC, Li VW, Ho TW, Chan EY, Ma AL, Cheung YF (2020) Left ventricular stiffness in paediatric patients with end-stage kidney disease. Pediatr Nephrol 35:1051–1060. https://doi.org/10.1007/s00467-020-04484-9
Farshid A, Pathak R, Shadbolt B, Arnolda L, Talaulikar G (2013) Diastolic function is a strong predictor of mortality in patients with chronic kidney disease. BMC Nephrol 14:280. https://doi.org/10.1186/1471-2369-14-280
Tsai WC, Lee WH, Wu PY, Huang JC, Chen YC, Chen SC, Hsu PC, Lee CS, Lin TH, Voon WC, Su HM (2019) Ratio of transmitral E wave velocity to left atrial strain as a useful predictor of total and cardiovascular mortality in hemodialysis patients. J Clin Med 9:85. https://doi.org/10.3390/jcm9010085
Çakıcı EK, Çakıcı M, Gümüş F, Tan Kürklü TS, Yazılıtaş F, Örün UA, Bülbül M (2020) Effects of hemodialysis access type on right heart geometry in adolescents. J Vasc Access 21:658–664. https://doi.org/10.1177/1129729819897454
Quennelle S, Ovaert C, Cailliez M, Garaix F, Tsimaratos M, El Louali F (2021) Dilatation of the aorta in children with advanced chronic kidney disease. Pediatr Nephrol 36:1825–1831. https://doi.org/10.1007/s00467-020-04887-8
Surak A, Filler G, Sharma AP, Torres Canchala LA, Grattan M (2020) Lower prevalence of aortic dilatation among preemptive pediatric renal transplant recipients - a cross-sectional cohort study. Pediatr Transplant 24:e13716. https://doi.org/10.1111/petr.13716
Madueme PC, Ng DK, Guju L, Longshore L, Moore V, Jefferies L, Warady BA, Furth S, Mitsnefes M (2020) Aortic dilatation in children with mild to moderate chronic kidney disease. Pediatr Nephrol 35:1023–1031. https://doi.org/10.1007/s00467-019-04469-3
Wyld MLR, De La Mata NL, Masson P, O’Lone E, Kelly PJ, Webster AC (2021) Cardiac mortality in kidney transplant patients: a population-based cohort study 1988–2013 in Australia and New Zealand. Transplantation 105:413–422. https://doi.org/10.1097/tp.0000000000003224
Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, Rush DN, Vazquez MA, Weir MR (2001) The evaluation of renal transplantation candidates: clinical practice guidelines. Am J Transplant 1(Suppl 2):3–95
K/DOQI Working Group (2005) K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45:S1–S153
Chadban SJ, Ahn C, Axelrod DA, Foster BJ, Kasiske BL, Kher V, Kumar D, Oberbauer R, Pascual J, Pilmore HL, Rodrigue JR, Segev DL, Sheerin NS, Tinckam KJ, Wong G, Knoll GA (2020) KDIGO Clinical practice guideline on the evaluation and management of candidates for kidney transplantation. Transplantation 104:S11–S103. https://doi.org/10.1097/tp.0000000000003136
Lentine KL, Costa SP, Weir MR, Robb JF, Fleisher LA, Kasiske BL, Carithers RL, Ragosta M, Bolton K, Auerbach AD, Eagle KA (2012) Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation: endorsed by the American Society of Transplant Surgeons, American Society of Transplantation, and National Kidney Foundation. Circulation 126:617–663. https://doi.org/10.1161/CIR.0b013e31823eb07a
Jefferies HJ, Virk B, Schiller B, Moran J, McIntyre CW (2011) Frequent hemodialysis schedules are associated with reduced levels of dialysis-induced cardiac injury (myocardial stunning). Clin J Am Soc Nephrol 6:1326–1332. https://doi.org/10.2215/cjn.05200610
Susantitaphong P, Koulouridis I, Balk EM, Madias NE, Jaber BL (2012) Effect of frequent or extended hemodialysis on cardiovascular parameters: a meta-analysis. Am J Kidney Dis 59:689–699. https://doi.org/10.1053/j.ajkd.2011.12.020
Maduell F, Moreso F, Pons M, Ramos R, Mora-Macià J, Carreras J, Soler J, Torres F, Campistol JM, Martinez-Castelao A (2013) High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J Am Soc Nephrol 24:487–497. https://doi.org/10.1681/asn.2012080875
Cannella G, La Canna G, Sandrini M, Gaggiotti M, Nordio G, Movilli E, Mombelloni S, Visioli O, Maiorca R (1991) Reversal of left ventricular hypertrophy following recombinant human erythropoietin treatment of anaemic dialysed uraemic patients. Nephrol Dial Transplant 6:31–37. https://doi.org/10.1093/ndt/6.1.31
Selby NM, Burton JO, Chesterton LJ, McIntyre CW (2006) Dialysis-induced regional left ventricular dysfunction is ameliorated by cooling the dialysate. Clin J Am Soc Nephrol 1:1216–1225. https://doi.org/10.2215/cjn.02010606
Selby NM, McIntyre CW (2011) Peritoneal dialysis is not associated with myocardial stunning. Perit Dial Int 31:27–33. https://doi.org/10.3747/pdi.2010.00007
Chapman JR (2010) The KDIGO clinical practice guidelines for the care of kidney transplant recipients. Transplantation 89:644–645. https://doi.org/10.1097/TP.0b013e3181d62f1b
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140. https://doi.org/10.1542/peds.2017-1904
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Le Page, A.K., Nagasundaram, N., Horton, A.E. et al. Echocardiogram screening in pediatric dialysis and transplantation. Pediatr Nephrol 38, 957–974 (2023). https://doi.org/10.1007/s00467-022-05721-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05721-z