Abstract
Objective
To quantitatively assess the impact of supine and standing positions on the morphological changes in the lumbar intervertebral foramen (LIF) in patients with adult spinal deformity (ASD) using upright CT and conventional supine CT.
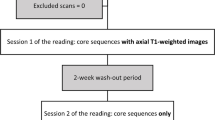
Materials and methods
Thirty patients with ASD were prospectively enrolled in this study. All subjects underwent standing whole spine posterior/anterior radiographs, lateral radiographs, and whole spine CT, both in the supine and upright standing positions. Two orthopedic surgeons independently measured nine radiographic parameters in the radiograph and the lumbar foraminal area (FA) and height (FH) in supine and upright CT. Statistical analyses were performed to evaluate the risk of LIF decrease when standing upright compared to the supine position. The chi-squared, t test, Pearson’s coefficients, intra- and inter-rater reliabilities, and ROC curves were calculated. The level of significance was set at p < 0.05.
Results
Among the 300 LIFs, both the lumbar FA and FH were either increased or decreased by > 5% in approximately 30% of LIFs each. The FA decreased in the lower lumbar spine. The concave side had a significantly higher rate of decreased FA and FH than the convex side (p < 0.05 and < 0.05, respectively). ROC analysis showed that narrowing of the intervertebral disc (cutoff > 0.05°) is a risk factor for decreased FA and FH.
Conclusions
This study describes the details of the changes in the neuroforamen using a novel upright CT. In patients with ASD, approximately 30% of LIFs either increased or decreased in size by > 5% when standing. The risk factors for LIF decrease are the lower lumbar spine, concave side, and narrow side of the disc wedge.





Similar content being viewed by others
References
Hasegawa T, An HS, Haughton VM, Nowicki BH. Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina. A cryomicrotome study in cadavera. J Bone Joint Surg Am. 1995;77(1):32–8. https://doi.org/10.2106/00004623-199501000-00005.
Kunogi J, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine. 1991;16(11):1312–20. https://doi.org/10.1097/00007632-199111000-00012.
Porter RW, Hibbert C, Evans C. The natural history of root entrapment syndrome. Spine. 1984;9(4):418–21. https://doi.org/10.1097/00007632-198405000-00017.
Vanderlinden RG. Subarticular entrapment of the dorsal root ganglion as a cause of sciatic pain. Spine. 1984;9(1):19–22. https://doi.org/10.1097/00007632-198401000-00006.
Jenis LG, An HS. Spine update. Lumbar foraminal stenosis. Spine. 2000;25(3):389–94. https://doi.org/10.1097/00007632-200002010-00022.
Mauch F, Jung C, Huth J, Bauer G. Changes in the lumbar spine of athletes from supine to the true-standing position in magnetic resonance imaging. Spine. 2010;35(9):1002–7. https://doi.org/10.1097/BRS.0b013e3181bdb2d3.
Inufusa A, An HS, Lim TH, Hasegawa T, Haughton VM, Nowicki BH. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine. 1996;21(21):2412–20. https://doi.org/10.1097/00007632-199611010-00002.
Iwata T, Miyamoto K, Hioki A, Ohashi M, Inoue N, Shimizu K. In vivo measurement of lumbar foramen during axial loading using a compression device and computed tomography. J Spinal Disord Tech. 2013;26(5):E177–82. https://doi.org/10.1097/BSD.0b013e318286f635.
Schmid MR, Stucki G, Duewell S, Wildermuth S, Romanowski B, Hodler J. Changes in cross-sectional measurements of the spinal canal and intervertebral foramina as a function of body position: in vivo studies on an open-configuration MR system. AJR Am J Roentgenol. 1999;172(4):1095–102. https://doi.org/10.2214/ajr.172.4.10587155.
Splendiani A, Ferrari F, Barile A, Masciocchi C, Gallucci M. Occult neural foraminal stenosis caused by association between disc degeneration and facet joint osteoarthritis: demonstration with dedicated upright MRI system. Radiol Med. 2014;119(3):164–74. https://doi.org/10.1007/s11547-013-0330-7.
Panjabi MM, Takata K, Goel VK. Kinematics of lumbar intervertebral foramen. Spine. 1983;8(4):348–57. https://doi.org/10.1097/00007632-198305000-00002.
Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077–82. https://doi.org/10.1097/BRS.0b013e31823e15e2.
Jinzaki M, Yamada Y, Nagura T, et al. Development of upright computed tomography with area detector for whole-body scans: phantom study, efficacy on workflow, effect of gravity on human body, and potential clinical impact. Invest Radiol. 2020;55(2):73–83. https://doi.org/10.1097/RLI.0000000000000603.
Yamada Y, Yamada M, Chubachi S, et al. Comparison of inspiratory and expiratory lung and lobe volumes among supine, standing, and sitting positions using conventional and upright CT. Sci Rep. 2020;10(1):16203. https://doi.org/10.1038/s41598-020-73240-8.
Yamada Y, Yamada M, Yokoyama Y, et al. Differences in lung and lobe volumes between supine and standing positions scanned with conventional and newly developed 320-detector-row upright CT: intra-individual comparison. Respiration. 2020;99(7):598–605. https://doi.org/10.1159/000507265.
Yamada Y, Jinzaki M, Hosokawa T, et al. Dose reduction in chest CT: comparison of the adaptive iterative dose reduction 3D, adaptive iterative dose reduction, and filtered back projection reconstruction techniques. Eur J Radiol. 2012;81(12):4185–95. https://doi.org/10.1016/j.ejrad.2012.07.013.
Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–86. https://doi.org/10.1001/archinternmed.2009.427.
Fujita N et al (2021) Determining the validity and reliability of spinopelvic parameters through comparing standing whole spinal radiographs and upright computed tomography images. BMC Musculoskelet Disord 22:899. https://doi.org/10.1186/s12891-021-04786-5
Modi HN, Suh SW, Song HR, Yang JH, Kim HJ, Modi CH. Differential wedging of vertebral body and intervertebral disc in thoracic and lumbar spine in adolescent idiopathic scoliosis – a cross sectional study in 150 patients. Scoliosis. 2008;3:11. https://doi.org/10.1186/1748-7161-3-11.
Liu H, Qian BP, Qiu Y, et al. Vertebral body or intervertebral disc wedging: which contributes more to thoracolumbar kyphosis in ankylosing spondylitis patients?: a retrospective study. Medicine. 2016;95(38):e4855. https://doi.org/10.1097/MD.0000000000004855.
Pugely AJ, Ries Z, Gnanapragasam G, Gao Y, Nash R, Mendoza-Lattes SA. Curve characteristics and foraminal dimensions in patients with adult scoliosis and radiculopathy. Clin Spine Surg. 2017;30(2):E111–8. https://doi.org/10.1097/BSD.0b013e3182aab1e3.
Fedorov A, Beichel R, Kalpathy-Cramer J, et al. 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30(9):1323–41. https://doi.org/10.1016/j.mri.2012.05.001.
Fujiwara A, An HS, Lim TH, Haughton VM. Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine. 2000;25(23):3036–44. https://doi.org/10.1097/00007632-200104150-00010.
Zhong W, Driscoll SJ, Tsai TY, et al. In vivo dynamic changes of dimensions in the lumbar intervertebral foramen. Spine J. 2015;15(7):1653–9. https://doi.org/10.1016/j.spinee.2015.03.015.
Aubin CE, Bellefleur C, Joncas J, et al. Reliability and accuracy analysis of a new semiautomatic radiographic measurement software in adult scoliosis. Spine. 2011;36(12):E780–90. https://doi.org/10.1097/BRS.0b013e3181f0825a.
Hasegawa T, Mikawa Y, Watanabe R, An HS. Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine. 1996;21(9):1005–9. https://doi.org/10.1097/00007632-199605010-00001.
Orita S, Inage K, Eguchi Y, et al. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 2016;26(7):685–93. https://doi.org/10.1007/s00590-016-1806-7.
Fu KM, Rhagavan P, Shaffrey CI, Chernavvsky DR, Smith JS. Prevalence, severity, and impact of foraminal and canal stenosis among adults with degenerative scoliosis. Neurosurgery. 2011;69(6):1181–7. https://doi.org/10.1227/NEU.0b013e31822a9aeb.
Simmons EH, Jackson RP. The management of nerve root entrapment syndromes associated with the collapsing scoliosis of idiopathic lumbar and thoracolumbar curves. Spine. 1979;4(6):533–41. https://doi.org/10.1097/00007632-197911000-00016.
Liu H, Ishihara H, Kanamori M, Kawaguchi Y, Ohmori K, Kimura T. Characteristics of nerve root compression caused by degenerative lumbar spinal stenosis with scoliosis. Spine J. 2003;3(6):524–9. https://doi.org/10.1016/S1529-9430(03)00490-X.
Epstein JA, Epstein BS, Lavine LS. Surgical treatment of nerve root compression caused by scoliosis of the lumbar spine. J Neurosurg. 1974;41(4):449–54. https://doi.org/10.3171/jns.1974.41.4.0449.
Nowicki BH, Haughton VM, Schmidt TA, et al. Occult lumbar lateral spinal stenosis in neural foramina subjected to physiologic loading. AJNR Am J Neuroradiol. 1996;17(9):1605–14.
Hasegawa K, Okamoto M, Hatsushikano S, Caseiro G, Watanabe K. Difference in whole spinal alignment between supine and standing positions in patients with adult spinal deformity using a new comparison method with slot-scanning three-dimensional X-ray imager and computed tomography through digital reconstructed radiography. BMC Musculoskelet Disord. 2018;19(1):437. https://doi.org/10.1186/s12891-018-2355-5.
Haimoto S, Nishimura Y, Hara M, et al. Clinical and radiological outcomes of microscopic lumbar foraminal decompression: a pilot analysis of possible risk factors for restenosis. Neurol Med Chir (Tokyo). 2018;58(1):49–58. https://doi.org/10.2176/nmc.oa.2017-0121.
Ohba T, Ebata S, Fujita K, Sato H, Devin CJ, Haro H. Characterization of symptomatic lumbar foraminal stenosis by conventional imaging. Eur Spine J. 2015;24(10):2269–75. https://doi.org/10.1007/s00586-015-3859-4.
Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003;16(1):44–50. https://doi.org/10.1097/00024720-200302000-00008.
Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20(12):1351–8. https://doi.org/10.1097/00007632-199520120-00005.
Vedantam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine. 1998;23(2):211–5. https://doi.org/10.1097/00007632-199801150-00012.
Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96(19):1631–40. https://doi.org/10.2106/JBJS.M.01459.
Ryan DJ, Protopsaltis TS, Ames CP, et al. T1 pelvic angle (TPA) effectively evaluates sagittal deformity and assesses radiographical surgical outcomes longitudinally. Spine. 2014;39(15):1203–10. https://doi.org/10.1097/BRS.0000000000000382.
Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine. 2009;34(17):1828–33. https://doi.org/10.1097/BRS.0b013e3181a13c08.
Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19(11):1824–36. https://doi.org/10.1007/s00586-010-1476-9.
Hioki A, Miyamoto K, Sakai H, Shimizu K. Lumbar axial loading device alters lumbar sagittal alignment differently from upright standing position: a computed tomography study. Spine. 2010;35(9):995–1001. https://doi.org/10.1097/BRS.0b013e3181bb8188.
Singh V, Montgomery SR, Aghdasi B, Inoue H, Wang JC, Daubs MD. Factors affecting dynamic foraminal stenosis in the lumbar spine. Spine J. 2013;13(9):1080–7. https://doi.org/10.1016/j.spinee.2013.03.041.
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (grant number 20K08056).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Japanese Ministry of Health, Labor, and Welfare, Japan Registry of Clinical Trails (jRCTs032180266). All methods were performed in accordance with the Declaration of Helsinki and the ethical standards of the institutional research committee. Signed informed consent was obtained from all individual participants included in the study.
Conflict of interest
One of the authors received a grant from Canon Medical Systems, which loaned the upright CT device to his institution. The funder was not involved in the design of the study; the collection, analysis, or interpretation of the data; or the writing of the manuscript. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fujita, N., Yagi, M., Yamada, Y. et al. Changes in the lumbar intervertebral foramen between supine and standing posture in patients with adult spinal deformity: a study with upright computed tomography. Skeletal Radiol 52, 215–224 (2023). https://doi.org/10.1007/s00256-022-04185-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04185-4