Abstract
Traditional medicine has provided a basis for health care and disease treatment to Chinese people for millennia, and herbal medicines are regulated as drug products in China. Chinese herbal medicines have two features. They normally possess very complex chemical composition. This makes the identification of the constituents that are together responsible for the therapeutic action of an herbal medicine challenging, because how to select compounds from an herbal medicine for pharmacodynamic study has been a big hurdle in such identification efforts. To this end, a multi-compound pharmacokinetic approach was established to identify potentially important compounds (bioavailable at the action loci with significant exposure levels after dosing an herbal medicine) and to characterize their pharmacokinetics and disposition. Another feature of Chinese herbal medicines is their typical use as or in combination therapies. Coadministration of complex natural products and conventional synthetic drugs is prevalent worldwide, even though it remains very controversial. Natural product–drug interactions have raised wide concerns about reduced drug efficacy or safety. However, growing evidence shows that incorporating Chinese herbal medicines into synthetic drug-based therapies delivers benefits in the treatment of many multifactorial diseases. To address this issue, a drug-combination pharmacokinetic approach was established to assess drug–drug interaction potential of herbal medicines and degree of pharmacokinetic compatibility for multi-herb combination and herbal medicine–synthetic drug combination therapies. In this review we describe the methodology, techniques, requirements, and applications of multi-compound and drug-combination pharmacokinetic research on Chinese herbal medicines and to discuss further development for these two types of pharmacokinetic research.
Similar content being viewed by others
Introduction
Chinese traditional medicine has provided for millennia a basis for disease treatment and health care to the Chinese nation and for China’s social stability. Particularly, this system of medicine has played a key role in management of various life-threatening epidemics in China [1] and is officially recommended for COVID-19 [2,3,4]. Since the foundation of the People’s Republic of China in 1949, the Chinese government has attached much significance to the practice and growth of Chinese traditional medicine, with herbal medicines being regulated as drug products. Chinese herbal medicines are often formulated as tablet, capsule, and droplet pill for oral administration and as injectable formulation for parenteral administration; they are required to be manufactured in compliance with good manufacturing practice as for drugs by licensed pharmaceutical companies [5]. Many Chinese herbal medicines are extensively used and prescribed by physicians of Western medicine, as well as physicians of traditional medicine. Since 1996, an ambitious plan has been underway in China to develop herbal medicines in line with contemporary standards of pharmaceutical sciences [6]; the Chinese National Medical Products Administration (NMPA) requires herbal medicines to be proved safe, effective, and quality-consistent before marketing [7]. Historically, herbal medicines were not extensively tested before they were approved in China, owing to paucity of the requisite technology at the time. Recently, a number of patent herbal medicines, extensively used in clinics, have shown therapeutic benefits in rigorous clinical trials, similar to those for synthetic drugs [8,9,10,11,12]. In addition, data from research on chemistry, pharmacodynamics, pharmacokinetics, drug–drug interaction potential, real-world adverse reactions, and so on have become increasingly available [13,14,15,16,17,18,19,20,21,22,23,24,25]; this facilitates better defining the therapeutic benefits of herbal medicines and conditions for their safe use. All these research efforts are to bring Chinese traditional medicine from empirical medicine into evidence-based one and are necessary to meet expanding regulatory requirements for Chinese herbal medicines and to ensure their sustainable use.
Unlike synthetic medicines, Chinese herbal medicines, which are prepared from single medicinal herbs or much more commonly from herb combinations, possess very complex chemical composition. Thus, identifying the chemical constituents that are together responsible for the therapeutic action of a medicine is vital to provide support for clinical decision-making related to the medicine’s therapeutic use. However, how to select compounds from a complex herbal medicine for pharmacodynamic study remains a big hurdle in such identification efforts. To address this issue, we seek to identify potentially important compounds (bioavailable at the action loci with significant associated exposure levels after dosing an herbal medicine) and to characterize their pharmacokinetics and disposition [26, 27]. We refer to this as multi-compound pharmacokinetic research. Over the past decade, great advances have been achieved in methodology, associated techniques, and applications of such multi-compound pharmacokinetic research on complex Chinese herbal medicines [28,29,30].
Another feature of Chinese herbal medicines is their typical use in a multi-substance-acting manner; this is a polypharmacological approach that impacts multiple targets simultaneously for treating multifactorial diseases. The multi-substance-acting herbal therapy involves three levels, i.e., an herb’s multiple bioactive compounds acting in concert, multi-herb combination as a single medicine (‘FangjiPeiwu’ in Chinese), and coadministration of herbal medicine and synthetic drug as separate medicines. Although combination therapy represents a relatively simple way to gain polypharmacology, a high degree of pharmacokinetic compatibility (PKC) is needed among the co-administered drugs to ensure the optimal therapeutic benefit. PKC is defined as absence of unintentional pharmacokinetic drug–drug interactions (DDIs) that can lead to reduced drug efficacy or increased drug toxicity [24, 29]. Concurrent use of complex natural products (including herbal medicines) with conventional synthetic drugs is prevalent worldwide but remains very controversial. Pharmacokinetic natural product–drug interactions have raised wide concerns about reduced drug efficacy or drug-related toxicity [31,32,33]. However, growing evidence shows that incorporating Chinese herbal medicines into synthetic medicine-based therapies for many multifactorial diseases delivers therapeutic benefits [9,10,11,12, 34, 35]. To address this issue, we seek to assess DDI potential of an herbal medicine and degree of PKC for combination therapies that include herbal medicines [29]. We refer to this as drug-combination pharmacokinetic research. Over the past years, much effort has been made to gain insight into how to evaluate herbal medicines acting as a perpetrator (involving multiple active compounds) or a victim in DDIs and how to evaluate PKC degrees of therapeutic combinations of herbal medicine with synthetic medicine, reflecting clinical reality [24, 36,37,38,39]. In this Review, we describe the methodology, requirements, and applications of both multi-compound and drug-combination pharmacokinetic research on Chinese herbal medicines and discuss their future development.
Multi-compound pharmacokinetic research on Chinese herbal medicines
Constituents responsible for therapeutic action of an herbal medicine
For a complex Chinese herbal medicine, it is hypothesized that only a few key constituents with favorable drug-like properties, rather than all constituents present, are responsible for the medicine’s therapeutic action [26]. An herbal constituent can be defined as ‘drug-like’ if it possesses the desired pharmacodynamic potency, a wide safety margin, appropriate pharmacokinetic properties, an adequate compound dose from the dosed medicine, and compatibility with co-administered drugs. To fully understand how a complex herbal medicine acts on the body to deliver therapeutic benefits, the pharmacodynamic investigation should be properly integrated with the pharmacokinetic investigation; this facilitates translation of the pharmacological findings into clinical application. Multi-compound pharmacokinetic investigations of Chinese herbal medicines have indicated that human subjects and laboratory animals are significantly exposed to only a few constituents, in their unchanged and/or metabolized forms, of the dosed medicine [21,22,23, 26, 27, 38,39,40,41,42,43,44,45,46,47]. Notable difference between the number of constituents present in the herbal medicine and that of compounds circulating after dosing the medicine is usually due to: (1) levels of the herbal constituents in the medicine differing greatly (up to four or five orders of magnitude), (2) influences of the enterohepatic barrier, (3) tissue distribution and systemic elimination (via biotransformation and excretion into bile and urine), etc. Such a pharmacokinetic investigation needs to assess all the chemical constituents (particularly those with a compound dose >0.01 μmol/day) present in the test herbal medicine with respect to body exposure to them and can serve as a sieve to determine which herbal compounds merit pharmacodynamic assessment [27]. In addition to identifying constituents that are together responsible for the therapeutic action of a herbal medicine, the multi-compound pharmacokinetic investigation can also help identify constituents that are together responsible for the medicine’s adverse effect and that can together perpetrate pharmacokinetic DDIs with herbal medicines.
Based on the preceding hypothesis, we recently investigated XueBiJing (an intravenous five-herb injection for sepsis care) pharmacokinetics and pharmacodynamics and successfully identified six constituents that could be together responsible for the injection’s anti-sepsis action (the details pending publication elsewhere). After obtaining a comprehensive understanding of chemical composition of XueBiJing, multi-compound pharmacokinetic investigations were performed to identify potentially important XueBiJing compounds (i.e., those exhibiting significant levels of systemic exposure in humans and in cecal ligation and puncture/CLP rats, both intravenously receiving the injection) and to characterize their pharmacokinetics and disposition. A total of 12 major circulating compounds (unchanged and metabolized) were identified from 124 constituents (compound dose, ≥0.01 μmol/day) of XueBiJing across the five component herbs. After being verified by NMR and LC/MS–MS, all prepared and purified entities of the major circulating compounds were assessed in vitro and in CLP rats for their anti-sepsis activities on immune response, inflammation, and coagulation. Six active XueBiJing compounds were identified and their different combinations were assessed by comparing with XueBiJing in CLP rats for the primary therapeutic outcome percentage survival. Finally, intravenously dosing a combination of the six compounds (at the same respective compound doses as in XueBiJing) resulted in a percentage survival of CLP rats same as that by intravenously dosing XueBiJing, and this was supported by bioequivalence of the six compounds between the combination and XueBiJing and high degree of PKC for both the combination and XueBiJing (i.e., limited potential for interactions among the six active compounds or for influences of other major circulating XueBiJing compounds on these compounds).
Requirements for multi-compound pharmacokinetic research on Chinese herbal medicines
Multi-compound pharmacokinetic investigation is a crucial step in identification of constituents that are together responsible for therapeutic action of an herbal medicine, and the medicine to be investigated needs to be an effective therapy in clinics. To this end, we proposed criteria for appropriately defining clinical efficacy of a patent herbal medicine [15]. An herbal medicine can be considered ‘effective’ if it has clear therapeutic action, i.e., being intended for use in treatment, prevention, mitigation, cure, or diagnosis of a specific disease. Clinical efficacy of the therapeutic action should be demonstrated by well-designed and effectively executed clinical trials, meta-analysis of multiple similarly designed trials, and/or recommendations by authoritative guidelines and expert consensuses. Based on understanding of pathophysiology of the disease, such efficacy needs to be supported by physiological and biochemical effects of the medicine and/or its compounds, observed in clinical and/or animal studies, relevant to the therapeutic action. In addition, the test medicine needs to be standardized for content of constituents and assessed for quality variability. The medicine should be of high-quality consistency.
To identify chemical constituents that are together responsible for the therapeutic action of an herbal medicine, the multi-compound pharmacokinetic investigation is performed and herbal compounds that merit pharmacodynamic assessment are determined. Bioavailability is the measure for this determination. Such bioavailability is defined with respect to a certain type or certain types of body exposure, which should be determined by the medicine’s therapeutic action and associated effects of the medicine and its compounds. For example, extracts of Ginkgo biloba leaves are widely used for prevention and treatment of ischemic cardiovascular and cerebrovascular diseases and cerebral insufficiency. Clinical and experimental studies suggest that G. biloba leaf extracts could dilate arteries, improve coronary and cerebral blood flow, protect endothelia, reduce lipid accumulation in foam cells, decrease blood viscosity and viscoelasticity, reduce erythrocyte malondialdehyde level, promote erythrocyte deformability, etc [48,49,50,51,52,53,54,55]. Meanwhile, neuroprotective effects of G. biloba leaf extracts have been documented, including antioxidation, inhibition of amyloid-β aggregation, attenuation of mitochondrion-induced apoptosis, normalization of neurogenesis reduction in hippocampus, etc [56,57,58,59]. Flavonols and terpene lactones are two classes of bioactive constituents putatively responsible for the preceding effects of G. biloba leaf extracts [60,61,62]. To understand bioavailability of these ginkgo compounds after dosing the extract, multi-compound pharmacokinetic research was focused on systemic and cerebral exposure to the compounds [40, 41, 45]. To date, the human commensal intestinal microbiota has increasingly gained interest for its important roles in training of host immunity, digesting food, regulating gut endocrine function and neurological signaling, modifying drug action and metabolism, eliminating toxins, and producing numerous compounds that influence the host [63, 64]. Imbalances in the composition and function of the microbiota are associated with diseases ranging from localized gastroenterologic disorders to neurologic, respiratory, metabolic, hepatic, cardiovascular diseases, etc. The microbiota is a major player in human health and disease and there has been considerable interest in therapeutic targeting the microbiota as well as mining this rich source in drug discovery efforts [65,66,67]. To better understand interactions between herbal medicines and the intestinal microbiota, the multi-compound pharmacokinetic research also involves investigating access of the medicines’ compounds to the intestinal microbiota by determining intestine-luminal exposure to the compounds.
Successful identification of constituents that are together responsible for the therapeutic action of an herbal medicine necessitates a comprehensive approach to the multi-compound pharmacokinetic investigation such that the potentially important herbal compounds are singled out with their accurate pharmacokinetic and disposition data and that no such compound is missed (in a few words, ‘precision without omission’). To this end, the multi-compound pharmacokinetic research should be performed on the basis of a comprehensive understanding of the chemical composition of the test medicine. To deal with the complex chemical composition of herbal medicines, the pharmacokinetic research is performed by integrating human study with various animal and in vitro studies and by integrating experimental approaches with informatics-based approach. In addition, pharmacokinetic matrix effects of an herbal medicine on pharmacokinetics of its major circulating compounds should be assessed in humans but more frequently in experimental animals (because single compound formulation that can be dosed is frequently not available for humans). The pharmacokinetic matrix effect is defined as a significant discrepancy in an exposure parameter (such as AUC, Cmax, or t1/2) or a primary pharmacokinetic parameter (such as CLtot,p or Vd) of an herbal compound, between dosing the medicine and dosing the single compound at the same dose level (for AUC and Cmax only) via the same administration route. Such pharmacokinetic matrix effects often result from substantial biotransformation of some other major constituents (i.e., matrix compounds) in the medicine into the measured compound and/or from perpetration of a significant pharmacokinetic interaction by the medicine’s matrix compounds with the measured compound. For example, circulating ginsenoside Rd after intravenously dosing XueShuanTong (a lyophilized extract of Panax notoginseng roots/Sanqi for intravenous administration) in humans exhibited notably longer t1/2 (58‒307 h) than that after intravenous dosing of pure ginsenoside Rd (about 18 h), while such t1/2 discrepancy in rats was 58 h versus 7.5 h [27, 39, 46, 68]. In this case, the matrix effect results from a transformation of ginsenoside Rb1 into ginsenoside Rd by hepatic glucosidase.
Methodology for multi-compound pharmacokinetic research on patent herbal medicines
Since most herbal medicines were, historically, not extensively tested before being approved (owing to paucity of the requisite technology at the time), the multi-compound pharmacokinetic research is performed, particularly for those medicines effective and extensively used in clinics, to support their sustainable use as medicines. For such patent medicines, methodology for multi-compound pharmacokinetic research is an integration of multiple studies and methods, i.e., comprising one forerunner study, one main study, two types of supportive studies, and three groups of supportive techniques (Fig. 1).
(Reprinted from Li et al., 2021 [30] with permission of Acta Pharm Sin).
The forerunner study is composition analysis of the test herbal medicine; this is pivotal for ensuring the whole multi-compound pharmacokinetic investigation to be ‘precision without omission’. Such composition analysis is usually based on liquid chromatography–mass spectrometry for polar and nonvolatile compounds and gas chromatography–mass spectrometry for nonpolar and volatile compounds and involves detection, characterization, and quantification of the medicine’s constituents. The assay for composition analysis is required to be of high ‘analyte-capacity’ simultaneously for the three component steps: sample preparation, chromatographic separation, and mass spectrometric detection. The levels of detected constituents of the medicine are defined with respect to compound dose from the dosed medicine; the dose is estimated by multiplying the content level of the constituent by the dose of the medicine. Although both the compound dose and the content level are equally governing factors in generating systemic exposure to the constituents, unchanged and metabolized, after dosing medicine, the former, rather than the latter, can be used to compare different medicines for the compound. The assay is also used to evaluate quality variability of the medicine, particularly for those constituents with a compound dose ≥1 μmol/day, because only one batch of medicine is usually assessed in the pharmacokinetic investigation. High quality consistency among different batches of medicine suggests the pharmacokinetic data of one test batch is applicable to other batches.
The main study is a human pharmacokinetic study by dosing the test herbal medicine. Constituents, bioavailable in unchanged and/or metabolized forms with significant levels of body exposure, are identified in the human study where the volunteers receive the medicine usually at the label daily dose. Such identification should be achieved for each component herb of the medicine (to reflect the entirety of the medicine’s formula), because all the component herbs are believed to contribute to the therapeutic action of the medicine. In a human pharmacokinetic study, three types of samples, i.e., blood, urine, and feces, are usually collected before and after the volunteers receive a single dose and sometimes repeated doses of the medicine. Blood samples are frequently heparinized and centrifuged to yield the respective plasma samples, which are analyzed to assess systemic exposure to unchanged and/or metabolized constituents after dosing and pharmacokinetics of the major circulating compounds. Urine samples are analyzed to facilitate assessing the systemic exposure to herbal constituents and to assess the role of renal excretion in elimination of the major circulating compounds and associated mechanisms. Feces samples are analyzed to assess intestine-luminal exposure to herbal constituents and their intestinal absorption, microbiota-mediated metabolism, and fecal excretion. Despite its significance to an herbal medicine, not all the desired pharmacokinetic data of the constituents after dosing the medicine can be obtained from a human pharmacokinetic study. Data for tissue distribution, hepatobiliary excretion, etc. are usually difficult to be obtained from the human study. When intravenous formulation of the medicine is not available for dosing in humans, the pharmacokinetic parameters oral bioavailability (F), plasma total clearance (CLtot,p), apparent volume of distribution (Vd), etc. often can not be obtained in humans. Dosing individual constituent compound is often another challenge faced in the human pharmacokinetic study. To address this issue, the human study is often supplemented with various animal and in vitro studies.
The two types of supportive studies are performed in experimental animals and in vitro. Regarding the animal studies that are performed to gain additional pharmacokinetic information on important constituents of an herbal medicine, it is pivotal to evaluate interspecies similarities and differences between animals (such as rats) and humans in body exposure, enzyme-mediated metabolism, transporter-mediated transport, plasma protein binding, etc. To compare body exposure to constituents between animals and humans, blood, urine, and feces samples are collected from the animals receiving the medicine and analyzed for the unchanged and metabolized constituents. The data on animal exposure to the constituents are compared with the respective human data gained from the preceding main study. To compare constituents’ enzyme-mediated metabolism, transporter-mediated transport, and plasma protein binding between animals and humans, in vitro studies of the compounds with animal proteins are performed in parallel with the respective in vitro studies with human proteins. Based on these comparisons, supportive animal pharmacokinetic studies are performed for those herbal compounds without significant interspecies differences. Frequently performed supportive animal studies include: studies by dosing individual chemical constituents (such as for assessing pharmacokinetic matrix effects of the test medicine) and by dosing via intravenous administration route and studies of dose–exposure correlation, tissue distribution, brain microdialysis, hepatobiliary excretion, enterohepatic circulation, portal-vein exposure, and intestine-luminal movement and disposition. Besides evaluating the preceding interspecies similarities and differences, the in vitro studies are performed to characterize important compounds of the medicine with respect to in vivo phase I and II metabolism, transport, and their interplay. In addition, in vitro studies of herbal compounds also involve characterizing, under anaerobic conditions, intestinal microbiota-mediated metabolism and assessing membrane permeability, water solubility, plasma protein binding, lysosomal trapping, blood-to-plasma ratio, etc.
The three groups of supportive techniques in pharmacokinetic investigation of an herbal medicine are methods for literature mining, sample analysis, and data processing. The literature mining is performed to improve the efficiency and performance of the preceding experimental studies for dealing with a complex herbal medicine. Literature mining (comprising retrieval, extraction, and review of information) involves defining desired information, setting right search terms, and using appropriate electronic databases to meet the aim of the whole pharmacokinetic investigation and the needs of each component experimental study. Regarding the sample analysis, four types of analytical methods are frequently developed and used in the pharmacokinetic investigation, i.e., assays for composition analysis of the herbal medicine, for chemical profiling of herbal compounds (unchanged and metabolized) in various in vivo study samples, for quantification of selected herbal compounds in various in vivo and in vitro study samples, and for quantification of tool compounds (such as known metabolites and known substrates for positive control) in various in vitro study samples. The first two types of assay are needed to be of high analyte-capacity, while the last two types are needed to be of high sample-throughput. Precisely and comprehensively obtaining the desired information is the core of sample analysis in a pharmacokinetic investigation. To achieve successful analysis, five elements should be carefully considered, i.e., information mining before assay development, collection of right samples, analyte prediction or selection of right analytes, analytical technique development and condition optimization, and data processing. This manner of sample analysis is referred to as ‘one core and five elements’. The data processing in a pharmacokinetic investigation of an herbal medicine frequently involves using literature-mined data to build or update herb-constituent libraries that support composition analysis of the herbal medicine, using measured compound doses to rank constituents detected in the medicine with respect to compound dose, using literature-mined data or metabolism software to predict metabolism of the medicine’s major constituents, using measured levels of body exposure to rank bioavailable constituents (unchanged and metabolized) in humans or animals receiving the medicine, proposing metabolic pathways of major constituents, using pharmacokinetics software to estimate pharmacokinetic parameters of the medicine’s major circulating compounds, using physiologically based pharmacokinetic (PBPK) modeling software to predict pharmacokinetics and disposition of the major circulating compounds, using GraFit software or the like to estimate metabolism and transport kinetic parameters of the medicine’s important compounds, using statistics software to perform statistical analysis, etc.
Differential pharmacokinetics of a class of herbal compounds and interspecies differences
Different classes of constituents may have significantly different compound doses from a dosed herbal medicine. In this case, the levels of systemic exposure to constituents of different classes can be very different. Even for a class of constituents with comparable compound dose levels, the compounds can also exhibit significantly different body exposure, pharmacokinetics, and interactions with drug metabolizing enzymes and transporters. For example, phenolic constituents of Salvia miltiorrhiza roots (Danshen) are caffeic acid derivatives, occurring as monomers (tanshinol), dimers (rosmarinic acid and salvianolic acid D), trimers (salvianolic acid A and lithospermic acid), and tetramers (salvianolic acid B), these Danshen compounds contain one or more catechol moieties with one or more carboxyl groups. In addition, protocatechuic aldehyde is also a major Danshen constituent, which contains a catechol compound without any carboxyl group. After oral administration of compound Danshen droplet pills (a Danshen-containing herbal medicine extensively used to treat angina pectoris) in humans, tanshinol was the only Danshen constituent that exhibited significant systemic exposure [26]. The other Danshen constituents salvianolic acids A, B, and D, rosmarinic acid, lithospermic acid, and protocatechuic aldehyde were either poorly absorbed from the gastrointestinal tract or were extensively metabolized, which resulted in poor detection of their unchanged forms in plasma after dosing. After intravenously dosing DanHong injection (another Danshen-containing herbal medicine extensively used to treat coronary artery disease and ischemic stroke), these Danshen phenolic compounds exhibit different interactions with hepatic and renal uptake transporters, resulting in different profiles of hepatobiliary and renal excretion [43, 69]. Lithospermic acid and salvianolic acid B (both >500 Da) underwent systemic elimination, initiated by OATP1B1/OATP1B3-mediated hepatic uptake; rosmarinic acid and salvianolic acid D (350–450 Da), initiated by OATP1B1/OATP1B3/OAT2-mediated hepatic uptake and by OAT1/2-mediated renal uptake; and protocatechuic acid and tanshinol (both <200 Da), initiated by OAT1/OAT2-mediated renal uptake and OAT2-mediated hepatic uptake. Here, protocatechuic acid is an oxidized metabolite of protocatechuic aldehyde by hepatic aldehyde dehydrogenase. Panax notoginseng roots (Sanqi) is a Chinese medicinal herb extensively used to treat ischemic cardiovascular and cerebrovascular diseases. Triterpene saponins (most of them derived from tetracyclic dammarane), including ginsenoside Rb1 and ginsenoside Rd of 20(S)-protopanaxadiol-type (ppd-type; with O-attached sugar moieties at C3 and/or C20 positions) and ginsenoside Rg1 and notoginsenoside R1 of 20(S)-protopanaxatriol-type (ppt-type; with a free hydroxyl group at the C-3 and O-attached sugar moieties at C6 and/or C20 positions), are the major bioactive constituents of Sanqi. Despite their structural similarity, significantly different elimination kinetics occurs between the ppd-type and ppt-type ginsenosides, as indicated by human t1/2 of 53.5‒175.9 h for the former and 1.3‒1.4 h for the later [39]. The different elimination kinetics results from differences both in hepatobiliary excretion and in renal excretion [36]. Unlike the ppt-type ginsenosides, the human hepatic transporters OATP1B3 and MRP2/BCRP/BSEP/MDR-1 do not mediate the excretion of ppd-type ginsenosides. In addition, extensive plasma protein binding limits glomerular-filtration-based excretion of the ppd-type ginsenosides, while low plasma protein binding facilitates such renal excretion of the ppt-type ginsenosides.
Significant interspecies differences in body exposure, pharmacokinetics, and interactions with drug metabolizing enzymes and transporters are another factors that need to be considered in multi-compound pharmacokinetic research on herbal medicines. For example, senkyunolides G and I are two phthalide constituents of XueBiJing injection and originate from the injection’s component herbs Ligusticum chuanxiong rhizomes (Chuanxiong) and Angelica sinensis roots (Danggui). After intravenously dosing XueBiJing, both the phthalides are major circulating compounds in humans, but only senkyunolide I is the major circulating phthalide in rats with senkyunolide G limitedly detected [23]. Terpene lactones are a class of bioactive constituents of ShuXueNing injection (a botanical drug product of Ginkgo biloba leaf extract, used as add-on therapies in patients with ischemic cardiovascular and cerebrovascular diseases). In humans, the terpene lactones ginkgolides A (molecular mass, 408 Da) and B (424 Da) were eliminated from the systemic circulation predominantly via glomerular-filtration-based renal excretion [45]. However, these two terpene lactones were eliminated both via renal and hepatobiliary excretion in rats [41]. After orally dosing Sanqi extract in humans, ppt-type ginsenosides are extensively deglycosylated by the colonic microbiota into 20(S)-protopanaxatriol, which can be absorbed in the colon and oxidized into several circulating metabolites by the host enterohepatic CYP3A. [42] However, such microbial deglycosylation occurs poorly in rats [27].
Research example: pharmacokinetics-based identification of pseudoaldosterogenic compounds of Glycyrrhiza uralensis roots (Gancao)
Glycyrrhiza uralensis root (Gancao) is a widely used medicinal herb in Chinese traditional medicine. However, Gancao-induced pseudoaldosteronism (characterized by hypokalaemia, hypertension, and peripheral edema) could be an adverse effect of Gancao-containing medicines and dietary products, via inhibition of renal 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) [70]. Given that Gancao is widely used as a component in Chinese herbal medicines, uncovering the compounds that are together responsible for the Gancao-induced adverse effect has implications for precisely defining conditions for safe use of Gancao-containing medicines, such as LianhuaQingwen capsule (an herbal medicine officially recommended as treatment for COVID-19 in China). Although glycyrrhizin is a major Gancao constituent with bioactivities such as inhibiting the replication of the SARS-associated virus, [71] this saponin and its several metabolites have been documented to inhibit 11β-HSD2 [72,73,74,75,76,77,78,79,80]. We identified pseudoaldosterogenic Gancao compounds from circulating Gancao compounds of dosed LianhuaQingwen, based on the compounds’ in vivo access to and in vitro inhibition of human renal 11β-HSD2 [47]. This renal enzyme is highly expressed in the epithelia of the distal tubule and collecting duct [81, 82]. After composition analysis of LianhuaQingwen for constituents originating from Gancao, we performed a multi-compound pharmacokinetic investigation by dosing the capsule in human volunteers, as well as in rats, to identify the major circulating Gancao compounds and to assess their in vivo access to renal 11β-HSD2. The identified potentially important Gancao compounds were then assessed in vitro for their inhibition of human renal 11β-HSD2. Among the 41 Gancao constituents detected in LianhuaQingwen, glycyrrhizin (1) and licorice saponin G2 (2) are the major Gancao saponin constituents. Poor intestinal absorption of 1 and 2 and their access to colonic microbiota result in significant levels of their respective deglycosylated metabolites glycyrrhetic acid (8) and 24-hydroxyglycyrrhetic acid (M2D) occurring in the systemic circulation after colonic absorption. These circulating metabolites are glucuronized/sulfated in the liver and then excreted into bile. Hepatic oxidation of 8 yields M2D. Due to their good membrane permeability, circulating 8 and M2D gain access to (via glomerular filtration and then passive tubular reabsorption) and potently inhibit renal 11β-HSD2. Collectively, 1 and 2 are metabolically activated to the pseudoaldosterogenic compounds 8 and M2D (Fig. 2). Although the microbial metabolites 8 and M2D are not the only Gancao-related compounds exhibiting inhibitory activities on 11β-HSD2, they are the only ones that are bioaccessible for the renal enzyme. Both 8 and M2D are extensively bound to plasma albumin (fu, <1%), limiting the renal glomerular filtration of 8 and M2D, with such binding acting as a ‘safety belt’ that allows the herb Gancao and Gancao-containing medicines to be widely used in Chinese traditional medicine. This finding allows us watch out for people who may susceptible to Gancao-induced pseudoaldosteronism, i.e., patients with hypoalbuminemia.
The Gancao constituents glycyrrhizin (1) and licorice saponin G2 (2) are metabolically activated by glucuronidase of the colonic microbiota to the metabolites 8 and M2D, respectively, which can access (via passive tubular reabsorption) and inhibit renal 11β-HSD2. (Reprinted from Lan et al., 2021 [47] with permission of Acta Pharmacol Sin).
Excessive and prolonged use of Gancao-containing herbal medicines and dietary products, as well as glycyrrhizin formulations, is a main cause of pseudoaldosteronism [72]. To ensure safe use of Gancao-containing medicines like LianhuaQingwen, (1) it is pivotal to increase awareness of Gancao-induced pseudoaldosteronism; (2) caution should be exercised when a Gancao-containing medicine is administered concurrently with other Gancao-containing medicines and dietary products; (3) a Gancao-containing medicine should not be administered to patients with decreased 11β-HSD2 activity, hypokalemia, hypertension, impaired liver function, or hypoalbuminemia; and (4) once pseudoaldosteronism occurs, the Gancao-containing medicine and co-administered Gancao-containing products should be withdrawn, and diuretics (such as spironolactone and eplerenone) and drugs (that can alkalinize pH of tubular fluid) may be administered to reduce tubular reabsorption of 8 and M2D.
Drug-combination pharmacokinetic research on Chinese herbal medicines
Pharmacokinetic compatibility (PKC) of a combination therapy
In the practice of Chinese traditional medicine, multi-herb combination therapies (FangjiPeiwu) have been extensively used to achieve therapeutic advantages of enhanced efficacy and safety. Two principles, i.e., QiqingHehe and JunChenZuoShi, guide how to select and combine herbs for the multi-herb combination therapy [83]. QiqingHehe sums up seven ways of using herbs, i.e., using an herb alone (Danxing) and using herbs in combination (to achieve beneficial combination effects and to avoid adverse combination effects). The beneficial combination effects are Xiangxu (the salutary effects of two herbs of similar actions being synergistic), Xiangshi (the salutary effect of an herb being enhanced by another herb exerting an additional or different action), Xiangwei (the adverse effect of an herb being reduced or minimized by another herb), and Xiangsha (an herb reducing or minimizing the adverse effect of another herb), while the adverse combination effects are Xiang’e (the salutary effect of an herb being reduced when combined with another herb) and Xiangfan (an herb producing adverse effect when combined with another herb). The QiqingHehe principle tells that combining herbs are not only necessarily beneficial/desirable but may also lead to undesirable/harmful effects and that the component herbs of such a combination should work in concert with one another to achieve desired therapeutic outcome. For multi-herb combination therapies, pharmacokinetic interactions among the component herbs remain a major concern. To this end, a combination therapy necessitates evaluation for PKC among its herbs. Recent advances in multi-compound pharmacokinetic research on Chinese herbal medicines are now revolutionizing the analytical toolbox available to support evaluation and understanding of herb-herb interaction potentials in a multi-herb combination, as well as PKC degree of the multi-herb combination. The JunChenZuoShi principle calls for hierarchy in a Chinese multi-herb combination by ranking the component herbs in order of importance of their therapeutic role in the combination. Component herbs of such a combination serve differently as monarch (the chief herb(s) treating the disease), minister (the herb(s) strengthening the therapeutic action of the monarch herb by acting similarly), adjuvant (the herb(s) treating the secondary comorbidity, reducing adverse effects of the monarch and minister herbs, or counteracting the drastic action of the monarch herb to suit the patient), and guiding herbs (the herb(s) facilitating the other component herbs’ access to their sites of action or agreeing in a friendly way). For a multi-herb combination, the role of a component herb is associated with the active compounds that it provides. The importance of such compounds depends on their pharmacodynamic activities and pharmacokinetic profiles, particularly their exposure levels and associated target engagement in the body.
The traditional ‘one drug-one target’ paradigm is based on a direct cause−effect relationship between the activity of a gene product and a particular phenotype. Consequently, a ‘magic bullet’ drug, which is designed to act on a single target with high selectivity and potency, is considered able to remedy a pathological phenotype, with limited adverse reactions. Although the idea of the ‘magic bullet’ is great, it is probably not the answer to treating multifactorial diseases [84, 85]. Indeed, there has been wide recognition that many multifactorial diseases with unmet therapeutic needs may require the polypharmacological approach to modulating multiple targets in concert. Polypharmacology encompasses both the combination therapy with multiple drugs acting on different targets and the multi-target single drug [86,87,88]. Although multi-target drugs have experienced growing interest [89,90,91], combination therapies are among the most promising and simple avenues towards treating multifactorial diseases [92,93,94]. Combination therapies are used to therapeutic advantage, because the beneficial effects are synergistic or additive by acting on different targets, because beneficial effects can be achieved with fewer adverse effects by using submaximal drug doses, or because drug resistance can be overcome. The combination therapy has proven effective in combating several multifactorial diseases, including acquired immune deficiency syndrome, hypertension, and cancer [95,96,97]. Despite these advantages, DDI issue is a major concern in the development of combination therapies. DDIs can occur at all levels, particularly pharmacokinetic DDIs that can lead to variability in drug exposure and disposition. Failure to identify the DDI risk can be a major source of overdosing or undertreatment, with severe clinical consequences. Accordingly, evaluating PKC degree is necessary to understand whether the therapeutic advantage of combination therapy is obstructed by serious pharmacokinetic DDIs.
In China, treatment of diseases using Chinese traditional medicine combined with Western medicine is a common practice. Many herbal medicines are incorporated into synthetic drug-based management of multifactorial diseases for therapeutic advantage, either because the salutary effects of the two types of medicines are complementary and/or synergistic or because such effects can be achieved with reduced drug adverse effects or reduced drug resistance [9,10,11,12, 98, 99]. In USA and many European countries, the use of dietary supplements or herbal medicinal products is prevalent, particularly in patient populations already exposed to synthetic medicines. Natural products, either as herbal medicines or as dietary supplements, can perpetrate clinically significant DDIs, leading to undesired alterations in exposure and disposition of the concomitant drugs [31, 33, 100]. For example, both grapefruit juice and St. John’s wort can perpetrate clinically significant natural product–drug interactions, by inhibiting and inducing CYP3A4, respectively [101,102,103,104,105,106]. These textbook examples of natural product–drug interaction have raised wide concerns about concurrent use of natural products and synthetic drugs, suggesting some overlap in interactions with drug metabolizing enzymes and/or drug transporters between the natural product and the synthetic drug. In addition, Chinese herbal medicines are regarded as therapeutic, hence are regulated as drug products in China. Therefore, when a Chinese herbal medicine is used concurrently with synthetic medicines, the herbal medicine can act as not only the perpetrator but also the victim in potential DDIs. Investigation of potentials both for herbal medicine–synthetic drug interactions and synthetic drug–herbal medicine interactions is important to facilitate evaluation of PKC degrees of a Chinese herbal medicine and the concomitant synthetic drug. High degree of pharmacokinetic compatibility (PKC) is desired for success of such combination therapy.
Chinese herbal medicine as potential perpetrator of pharmacokinetic DDI
Natural product–drug interactions are widely recognized as an issue for many drug therapies. However, the evidence of such interactions is often based on data derived from in vitro or animal studies, isolated case reports that frequently lack pertinent information, or some clinical trial results. Early evaluations of potential natural product–drug interactions were fraught with difficulties and often yielded inconclusive and contradictory results. These DDI investigations of natural products did not reveal their compounds that could together perpetrate the potential DDIs or define the conditions under which the interactions could take place. Also, the natural products tested were not systematically characterized for their chemical composition and pharmacokinetics in humans. In other words, a multi-compound pharmacokinetic investigation was not performed to facilitate drug-combination pharmacokinetic investigation of the herbal medicine by singling out their compounds that were bioavailable with significant body exposure levels and accessible to the human interacting protein (drug metabolizing enzyme or drug transporter). Thus, more rigorous drug-combination pharmacokinetic research is needed.
When documented case reports suggest possible DDIs are perpetrated by an herbal medicine or when chemical constituents of an herbal medicine show significant modulation of drug metabolizing enzymes and/or drug transporters, the herbal medicine should be considered for evaluation of its potential for perpetrating DDI. Unlike synthetic drugs that usually contain single chemical entities, herbal medicines often contain multiple constituents, many of them bearing structural resemblance. Such structurally related herbal compounds can interact with the same interacting protein to different extents and together perpetrate the DDI. Accurate evaluation of interaction potential of an herbal medicine relies on identifying all its constituents that may contribute considerably to perpetrating the DDI. Recently, we have proposed an approach for rigorously investigating potential of an herbal medicine for perpetrating DDI: (1) thoroughly characterizing the chemical composition of the test herbal medicine; (2) identifying major circulating herbal compounds, unchanged and metabolized, that are accessible to the locus of interaction; (3) assessing the modulation potencies of these herbal compounds on the relevant interacting proteins; (4) characterizing the herbal compounds’ disposition factors that can affect their exposure levels and access to the interacting protein; and (5) evaluating how the identified herbal compounds together modulate the same interacting protein [38]. Results from such investigations will inform PBPK model-based prediction and, if necessary, clinical DDI studies of the herbal medicine.
The triterpene saponins ginsenosides of ppd-type and ppt-type are the major bioactive constituents of three medicinal ginseng herbs Panax ginseng root (Renshen), P. notoginseng root (Sanqi), and P. quinquefolius root (Xiyangshen). Considerable speculation regarding DDIs perpetrated by products of ginseng herb frequents the literature, but conclusive evidence for such interactions is lacking [31, 32, 107,108,109,110,111]. For example, significantly reduced levels of systemic exposure to oral midazolam (a probe substrate for CYP3A phenotyping) after a 28-day oral administration of P. ginseng capsule (500 mg, b.i.d.; Vitamer, CA, USA) in healthy volunteers were reported, suggesting possible induction of CYP3A by the botanical product [112]. However, another human DDI investigation reported that 28-day administration of the same P. ginseng capsule (500 mg, t.i.d.; Vitamer, CA, USA) did not significantly alter midazolam metabolism [113]. In addition to the approach of midazolam phenotyping being different between the two investigations, information was not provided on interaction-related human pharmacokinetics of the test botanical products and the quality consistency between the product lots used in the two investigations. Ginsenosides are the main pharmacologically active constituents of XueShuanTong, a lyophilized extract of Sanqi for intravenous administration. Recently, ginsenosides, particularly those of ppd-type, were found to potently inhibit hepatic OATP1B3 and, to a lesser extent, OATP1B1 [36, 38]. Given that co-medication of XueShuanTong with synthetic drugs is common for treatment of ischemic cardiovascular or cerebrovascular diseases and that levels of systemic exposure to ginsenosides via intravenous administration route are much higher than the respective ones via oral administration route [39, 42], DDI information is essential for making clinical decision on therapies co-administering XueShuanTong with synthetic drugs. To this end, XueShuanTong-drug interaction potential was evaluated and the investigation focused on assessment of CYP3A induction and OATP1B inhibition.
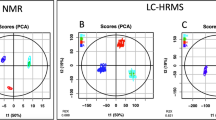
Literature-mined information, as well as our earlier related study findings [39, 42], was used to facilitate the DDI investigation by avoiding missing potentially important XueShuanTong compounds. After thorough composition analysis of XueShuanTong for ginsenosides and evaluation of associated lot-to-lot quality variability, a multi-compound pharmacokinetic study was performed in healthy volunteers (intravenously receiving XueShuanTong) to identify circulating ginsenosides, unchanged and metabolized, with significant levels of systemic exposure and their pharmacokinetics that was important for perpetrating the DDI. Two types of XueShuanTong-perpetrated DDI study were performed: (1) evaluation of potential of XueShuanTong for inducing CYP3A in healthy volunteers and the results were confirmed by a cell-based induction study with respect to mRNA level and enzyme activity, using the major circulating ginsenosides and (2) prediction of XueShuanTong’s potential for inhibiting OATP1B3 by the major circulating ginsenosides using their time-dependent unbound plasma concentrations in humans. In the CYP3A induction study, possible influence of enzyme inhibition on the results was assessed in vivo and in vitro. In the OATP1B inhibition study, inhibition of OATP1B together by multiple XueShuanTong ginsenosides was assessed in vitro, and the data were processed using the Chou-Talalay method. Samples were analyzed by liquid chromatography/mass spectrometry.
A total of 50 ginsenosides with compound doses of >0.01 μmol/day were detected and characterized in XueShuanTong: 14 ppd-type ginsenosides, 18 ppt-type ginsenosides, and 18 ginsenosides of other types. As shown in Fig. 3, ginsenosides Rb1 and Rd of ppd-type and ginsenoside Rg1 and notoginsenoside R1 of ppt-type were the major circulating XueShuanTong compounds; their DDI-related pharmacokinetics comprised compound dose-dependent levels of systemic exposure and, for ginsenosides Rb1 and Rd, long terminal half-lives (32‒57 and 58‒307 h, respectively) and low unbound fractions in plasma (0.8%‒2.9% and 0.4%‒3.0%, respectively). Repeatedly dosing intravenous XueShuanTong does not induce human CYP3A4/3A5. Based on human pharmacokinetics and overall inhibitory potency of its bioavailable ginsenosides, intravenously dosed XueShuanTong is found to have high potential for OATP1B3-mediated drug interactions, which is attributed chiefly to ginsenoside Rb1. This finding informs a need for further PBPK model-based prediction of the interaction potential for XueShuanTong and, if necessary, clinical DDI studies of XueShuanTong. Because the ginsenosides selectively inhibit OATP1B3, XueShuanTong is likely to alter pharmacokinetics of selective substrates of OATP1B3 when co-administered, rather than selective substrates of OATP1B1 or dual substrates of OATP1B1/1B3. Several selective OATP1B3 substrates, such as cholecystokinin-8, telmisartan, amanitin, dioscin, convallatoxin, ouabain, dihydroouabain, ouabagenin, and ppt-type ginsenosides, have been reported [36, 114,115,116,117,118]. Information on potential DDIs should be an important part of the patient information leaflet of herbal medicines. However, most Chinese herbal medicines currently lack such information. Increased awareness of ginsenosides’ pharmacokinetics and XueShuanTong-drug interaction potential will help ensure safe use and effective combination therapies of XueShuanTong and synthetic drugs.
Ginsenosides present in XueShuanTong (a), their systemic exposure and renal excretion in human volunteers who received a 2.5-h infusion of XueShuanTong at 500 mg/person (b), and estimated total DDI indexes on OATP1B1 and OATP1B3 for a single 2.5-h intravenous infusion of XueShuanTong at 500 mg/person and for repeated doses of XueShuanTong at 500 mg/person every day on day 18 (c). Chemical structures of the major circulating ginsenosides after dosing XueShuanTong are shown in panel (d). The XueshuanTong constituents 1‒14 are ppd-type ginsenosides; 31‒48 are ppt-type ginsenosides; and 51‒68 are other type ginsenosides. M4, M6, M8, and M11‒M14 are metabolites of the ppt-type ginsenosides (see Ref. [42] for more information about these metabolites). 1, ginsenoside Rb1; 2, ginsenoside Rd; 31, ginsenoside Rg1; 32, notoginsenoside R1; PPD, 20(S)-protopanaxadiol; and PPT, 20(S)-protopanaxatriol. Glc glucopyranosyl, Xyl xylopyranosyl. (Reprinted from Pintusophon et al., 2019 [39] with permission of Acta Pharmacol Sin).
Chinese herbal medicine as potential victim of pharmacokinetic DDI
In China, herbal medicines are regarded as therapeutic and regulated as drug products. This requires evaluating potential of Chinese herbal medicines not only for perpetrating DDIs but also for acting as victim in DDIs. Natural products such as dietary supplements in many Western countries are not drug products; their therapeutic effects and adverse effects do not need to be and are normally not well defined, like those of conventional drugs. So, little is known which compounds are responsible for these effects of the natural products. Unlike natural product–drug interactions, drug-natural product interactions have been limitedly investigated and documented for their potential.
As a prerequisite for evaluating drug–herbal medicine interaction potential, it should be understood which compounds are responsible for therapeutic or adverse effect of the test herbal medicine and whether altered levels of exposure to these active compounds are associated with reduced efficacy or increased toxicity of the herbal medicine. An herbal medicine is deemed a potential victim of DDI if the enzyme(s) or transporter(s) mediating the intestinal absorption or systemic elimination of its active compounds can be inhibited without other route(s) that can significantly compensate the impaired route or if the interacting protein(s) can be induced.
Inflammation in the liver precedes and promotes the progression towards liver cirrhosis and hepatocellular carcinoma. Intravenous glycyrrhizin has been incorporated into the management of liver diseases (including cause-specific treatment) due to its additional value of anti-inflammation and hepatoprotection [119,120,121,122,123]. Glycyrrhizin, triterpene saponin, is a major constituent present in Glycyrrhiza uralensis root (Gancao) and other medicinal Gancao species (G. inflate root and G. glabra root). Despite the therapeutic effects, high dose and prolonged use of intravenous glycyrrhizin formulations, as specified on the patient information leaflets, possibly induce pseudoaldosteronism by inhibiting 11β-HSD2. Pseudoaldosteronism can result from increased AUC0-∞ of glycyrrhizin. Unlike oral administration, intravenous administration yields unchanged glycyrrhizin as the major circulating form. Unchanged glycyrrhizin is eliminated mainly via hepatobiliary excretion, rather than renal excretion and metabolism. Therefore, level of systemic exposure to and hepatobiliary excretion of unchanged glycyrrhizin are factors influencing intravenous glycyrrhizin-induced pseudoaldosteronism. To this end, human transporters mediating hepatobiliary excretion of glycyrrhizin were characterized at the cellular and vesicular levels and compared with rat hepatic transporters. The role of Oatp1b2 in glycyrrhizin’s elimination and pharmacokinetics was evaluated in rats using the inhibitor rifampin. A PBPK model for glycyrrhizin, incorporating transporter-mediated hepatobiliary excretion, was established and applied to predict human systemic exposure to glycyrrhizin and its potential as the victim in DDI [37].
Glycyrrhizin is of poor membrane permeability. Hepatobiliary excretion of glycyrrhizin involves human OATP1B1/1B3 (Oatp1b2 in rats)-mediated hepatic uptake from blood and human MRP2/BCRP/BSEP/MDR1 (Mrp2/Bcrp/Bsep in rats)-mediated hepatic efflux into bile. No other hepatic transporters exhibit such hepatic uptake activity. In rats, rifampin-impaired hepatic uptake of glycyrrhizin can significantly increase its systemic exposure to glycyrrhizin (Fig. 4). Glomerular-filtration-based renal excretion of glycyrrhizin is slow due to extensive protein binding in plasma. Quantitative analysis using the PBPK model suggests a high likelihood for glycyrrhizin to be a victim of hepatic DDIs when co-medicated with potent dual inhibitors of OATP1B1/1B3 (Fig. 4).
Observed (dots) and PBPK model-simulated (lines) plasma concentration-time profiles of glycyrrhizin in rifampin-untreated (control) and rifampin-treated rats that intravenously received glycyrrhizin at 2.6 mg/kg (a), such plasma concentration-time profiles in humans who received a 12-min intravenous infusion of glycyrrhizin at 40 (in green), 80 (in blue), and 120 (in red) mg/person (b), and PBPK model-predicted influence of impaired hepatic OATP1B1/1B3 activities on levels of systemic exposure to glycyrrhizin (c and d). Chemical structure and comparative elimination routes of glycyrrhizin are shown in panel (e). The plasma levels of glycyrrhizin were prospectively predicted under a 12-min i.v. infusion of glycyrrhizin at 120 mg/person. The assumption, used as a worst-case estimate, was that the inhibition of OATP1B1/1B3 was constant over time. Sustaining the impairment of OATP1B1/1B3 activities by the inhibitory perpetrator depends on the perpetrator’s inhibition potency and pharmacokinetics (the unbound plasma concentrations and elimination t1/2). The observed human plasma concentration data of glycyrrhizin were digitalized from a publication by Yamamura et al. [148] with permission of Elsevier and APhA. Glu glucuronosyl. (Reprinted from Dong et al., 2018 [37] with permission of John Wiley and Sons).
The OATP1B1/1B3-mediated hepatic uptake governs systemic clearance of and systemic exposure to glycyrrhizin. Given that there are many dual OATP1B1/1B3 inhibitors (including the direct-acting antiviral agents paritaprevir and ritonavir) used in clinics and that substantial impairment of OATP1B1/1B3 activities (by ≥80%) can result in a significantly increased plasma AUC0-∞ and prolonged t1/2 of glycyrrhizin, caution should be exercised in the use of intravenous glycyrrhizin, due to its high likelihood to be a victim in DDIs. This DDI information facilitates ensuring safe glycyrrhizin-including combination therapies for liver diseases. To prevent such drug-glycyrrhizin interactions, plasma concentrations of both glycyrrhizin and co-administered dual inhibitors of OATP1B1/1B3 should be monitored and their dosages optimized accordingly. OATP1B1 and OATP1B3 can compensate for the lack of each other. So, coadministration with a selective inhibitor of OATP1B1 or OATP1B3 may not lead to significant changes in level of systemic exposure to glycyrrhizin.
PKC evaluation for an herbal-synthetic medicine combination
Drugs in a combination therapy, particularly for multifactorial diseases, can have distinct mechanisms of action and exert enhanced pharmacodynamic effect. To ensure such therapeutic benefit, a high degree of PKC within the combination therapy is desired, i.e., absence of serious pharmacokinetic DDI among the co-administered drugs. In China, growing evidence shows that incorporating herbal medicines into synthetic drug-based therapies for multifactorial diseases delivers therapeutic benefits [9,10,11,12, 98, 99]. However, pharmacokinetic natural product–drug interactions are a widely recognized issue that may negate such benefits. Therefore, a drug-combination pharmacokinetic approach to assessing degree of PKC for an herbal medicine in combination with synthetic drugs was proposed to provide evidence to guide clinical decision on such combination therapies [24]. So far, more commonly known is the evaluation of pharmacokinetic natural product–drug interactions, which mostly seeks to identify natural products (like grapefruit juice and St. John’s wort) that can perpetrate therapeutically significant DDIs with synthetic drugs. Although the recently proposed assessment of PKC degree for a therapeutically promising herbal medicine/synthetic drug combination follows the same mechanistic basis of DDI, it differs in some aspects. The PKC investigation seeks to define the degree of PKC between the herbal medicine and the co-administered synthetic drugs and to provide mechanistic evidence for any DDI risks if existing within the combination therapy. In the PKC investigation, the test herbal medicine (like the test co-administered synthetic drugs) is evaluated for its potential both as perpetrator and victim for DDIs, because it is also regarded as therapeutic. In contrast, the test natural product is usually not considered therapeutic in natural product–drug interaction studies, and so is evaluated for its potential as perpetrator only, (and not as victim) of the DDIs, with the goal to avoid or minimize therapeutic failure of synthetic medicines. In addition, to support decision-making regarding clinical use of a drug combination, the PKC investigation considers all interacting proteins that are related to the combination therapy and highlighted for DDIs, while the traditional investigation of natural product–drug interaction often focuses on one or a few of interacting proteins.
As a life-threatening organ dysfunction caused by a dysregulated host response to infection, sepsis is a critical condition, for which treatment guideline and expert consensuses in China recommend adding the Chinese herbal medicine XueBiJing (an intravenous five-herb injection) to antibiotic-based sepsis care [124,125,126,127]. Because infection is the triggering event in sepsis, prompt initiation of appropriate antibiotic therapies to eradicate the pathogens is a cornerstone of sepsis care [128]. Meanwhile, attenuating the host response to infection is also significant and needs to be promptly initiated. However, search for synthetic therapeutic agents for modulating the host response has been unsuccessful [129,130,131]. Combining XueBiJing with conventional sepsis care was found to further reduce 28-day mortality of patients with sepsis and incidence of complications and improves prognosis, with low incidence of adverse effects [12, 132]. Pharmacological studies suggest that XueBiJing could modulate the septic response by inhibiting the uncontrolled release of inflammatory mediators, relieving an early overabundant innate immune response and potentially cumulative immunosuppression, attenuating the crosstalk between inflammation and coagulation, protecting endothelial cells, and maintaining physiological functions of vital organs [18,19,20, 133,134,135]. The therapeutic effects of XueBiJing are distinct from and complementary to the antibiotic therapy. Despite its extensive use in sepsis care (over 600,000 patients yearly in China), report on DDIs with XueBiJing is scarce; this may be attributed to under-recognition, under-reporting, and under-researching of such DDIs. Many antibiotics have high potential for DDIs, particularly in critically ill patients who are predisposed to DDIs due to multi-drug usage and who often present with organ dysfunction and multiple comorbidities [136,137,138]. Given these factors, as well as complex chemical composition of and many bioactive constituents present in XueBiJing, it became important to evaluate systematically the PKC degree of the XueBiJing/antibiotics combination therapy.
The PKC investigation, considering potential for both XueBiJing-antibiotic interactions (perpetrated by XueBiJing) and antibiotic-XueBiJing interactions (perpetrated by the antibiotic), involved evaluation of the therapy’s PKC degree and identification of DDI risks in the combination [24]. The drug-combination pharmacokinetic investigation required: (1) a wealth of data on the pharmacokinetics/disposition of XueBiJing and antibiotics and their DDI liabilities and (2) a method for data processing. Data on human pharmacokinetics of XueBiJing compounds that were bioavailable for DDIs were obtained from our earlier multi-compound pharmacokinetic investigations of the injection. Literature mining was performed to identify antibiotics used for sepsis care in China and to obtain data on their pharmacokinetics/disposition and DDI liabilities, as well as data on DDI liabilities of XueBiJing and its herbal compounds. In addition, in vitro studies were performed to obtain additional required data on DDI potential of the XueBiJing compounds, and of the antibiotics, by modulating drug metabolizing enzymes and drug transporters. Data processing was then performed in steps, i.e., pairing the compounds, assessing the desirability of the pair-associated DDIs and estimating PKC index (ranging from 0 to 1) of the combination therapy. A high PKC index (close to 1) represents a high degree of PKC for the combination therapy, i.e. with a low undesirable DDI risk, whereas a low PKC index indicates a low degree of PKC, with a high undesirable DDI risk. Figure 5 summarizes the elements considered in evaluating the PKC of the XueBiJing/antibiotic combination therapy. Low DDI potential indicated by static-mechanistic-model-based investigation usually correlates with low clinical DDI potential, but high interaction potential indicated by such investigation does not necessarily translate to high clinical DDI potential. To this end, only the identified undesirable interactions with high potential would be further investigated by performing PBPK model-based prediction and, if necessary, relevant clinical DDI studies.
By integrating informatics-based approach with experimental approach and by developing a compound pair-based method for data processing, the PKC degree of XueBiJing/antibiotic combination therapy was systematically evaluated to guide clinical decision on XueBiJing/antibiotic combination for sepsis care [24]. To reflect clinical reality, 45 antibiotics commonly used in sepsis care in China and 12 XueBiJing compounds bioavailable for DDIs were selected for the drug-combination pharmacokinetic investigation. No XueBiJing compound could pair, as perpetrator, with the antibiotics. Although some antibiotics could, due to their inhibition of UGT2B15, OAT1/2 and/or OATP1B3, pair with senkyunolide I, tanshinol and salvianolic acid B, the potential interactions (resulting in increased systemic exposure) were likely desirable due to these XueBiJing compounds’ low baseline exposure levels. Inhibition of aldehyde dehydrogenase (ALDH) by seven antibiotics (i.e., imipenem, meropenem, ceftazidime, penicillin, ampicillin, oxacillin, and flucloxacillin) probably led to undesirable reduction of systemic exposure to protocatechuic acid from XueBiJing. The XueBiJing/antibiotic combination exhibited a high degree of PKC at clinically relevant doses, with a PKC index of 0.94, which supports concurrent use of the two types of medicines in sepsis care. Figure 6 depicts this evaluation of PKC degree of combination therapy of XueBiJing and antibiotics. Although the early identification and treatment of sepsis is desirable, prompt administration of all the necessary medications increases the drug interaction risk. For optimal sepsis care, a high degree of PKC is desirable not only between XueBiJing and antibiotics but also between XueBiJing and other medicines and among different types of synthetic medicine. The preceding drug-combination pharmacokinetic approach can be applied to investigate other drug combination therapies.
A1‒A45, 45 antibiotics commonly used in sepsis care in China (see Ref. [24] for the detailed information); X1‒X12, 12 major XueBiJing compounds, unchanged and metabolized, that are bioavailable for drug DDIs and bioactive for sepsis care (see Ref. [24] for the detailed information). (Reprinted from Li et al., 2019 [24] with permission of Acta Pharm Sin B).
Outlook
Despite the many advances and successes described in this Review, only a limited numbers of Chinese herbal medicines have been extensively investigated and the impact of pharmacokinetic research on the modernization of Chinese traditional medicine is still limited owing to the sophistication, expertise, extensive experimental work, high cost, and long study period required. We believe that this situation is changing as pharmacokinetic research is increasingly recognized as a powerful and versatile tool to help identify therapeutically important constituents of complex Chinese herbal medicines and develop herbal medicines for use as or in combination therapies of multifactorial diseases by acting on multiple targets in concert.
More technological advances and broader studies are needed in multi-compound pharmacokinetic research on the Chinese herbal medicine to enhance our ability to identify the medicine’s important constituents that are together responsible for the therapeutic action and/or adverse effect of the medicine. Recently, abundant high-quality data exist and are searchable; understanding of in vitro and in vivo methodology continues to improve; and computational power continues to increase. All these have boosted drug discovery, including the ability to identify drug candidates with appropriate pharmacokinetic properties [139, 140]. By utilizing artificial intelligence/machine learning, the pharmacokinetic properties and overall profiles of numerous constituents can be predicted for an herbal medicine in a more high-throughput and cost-effective manner than traditional methods. Rational and effective integration of the artificial intelligence-based predictions with various experimental measurements can fuel the multi-compound pharmacokinetic research on complex herbal medicines. Initiatives to incorporate artificial intelligence into pharmacokinetic prediction of herbal compounds and medicines are already underway and the main questions are how to best utilize the technique and how to evaluate the benefit of its applications. One of the challenges posed in this field is lack of high-quality experimental data.
In the multi-compound pharmacokinetic research, all types of body exposure that are relevant to the therapeutic action and/or adverse effect of an herbal medicine should be investigated for the medicine’s constituents. Given that the human intestinal microbiota is integral to the physiology of its host [63, 64] and is a major source of variability in pharmacokinetics of and response to many drugs [141, 142], intestine-luminal exposure to the herbal compounds after dosing an herbal medicine should be assessed to determine the compounds’ access to the microbiota. Traditionally, pharmacokinetic investigations have focused on systemic exposure to the drugs and have mostly ignored the intestine-luminal exposure and the significant direct and indirect impacts of the intestinal microbiota on the systemic exposure of drugs. The intestine-luminal exposure to herbal compounds after an orally dosed herbal medicine involves multiple elements: passage of the unchanged constituents through the digestive tract, loss of the unchanged constituents owing to intestinal absorption (particularly in the upper gastrointestinal tract), loss of the unchanged constituents owing to metabolism by the intestinal enzymes (such as lactase-phlorizin hydrolase) or the microbiota, appearance of the metabolites owing to these intestinal metabolism, loss of the metabolites owing to intestinal absorption or further metabolism by the microbiota, and appearance of the metabolites owing to biliary excretion of the conjugated metabolites (most often glucuronides) [143]. After intravenously dosing an herbal injection, the intestine-luminal exposure to herbal compounds is initiated by biliary excretion of the herbal compounds (unchanged and metabolized) and occasionally by intestinal excretion of such compounds. The intestine-luminal exposure via intravenous administration is normally much lower than that via oral administration. In addition, the intestine-luminal exposure to herbal compounds is influenced by many factors, including physicochemical properties of the herbal compounds, expression and function of the intestinal enzymes and transporters and the interplay of these proteins, thickness and pH of mucus, intestinal tissue structure, composition and function of the intestinal microbiota, DDI, gene variants, etc. It is generally thought that drug compounds most accessible to the intestinal microbiota are those that are orally administered but not absorbed in the upper gastrointestinal tract. However, after orally dosing Gancao-containing medicine, the compounds that exhibit significant colon-intestinal exposure are the microbial metabolites glycyrrhetic acid and 24-hydroxyglycyrrhetic acid, rather than the respective unabsorbed parent constituents glycyrrhizin and licorice saponin G2, which appear not to occur in the colon [47]. Assessment of human intestine-luminal exposure to herbal medicines is usually based on analysis of the feces samples, but further investigating the exposure is difficult in healthy volunteer and patient studies. Animal models can be informative but have limited translational potential due to significant interspecies variations in the intestinal microbiota. Therefore, human microbiota-associated animal models have been used widely in intestinal microbiome research [144,145,146]. We have started to utilize human microbiota-associated rats in intestine-luminal exposure studies of herbal medicines. Overall, current understanding of intestine-luminal exposure to herbal medicines is incomplete and there are questions still to be answered.
After the major exposed compounds are identified for an herbal medicine, two important aspects need to be further investigated, particularly for those that are pharmacologically and/or toxicologically active, i.e., (1) effective modulation of their body exposure levels and (2) their in vivo access to the associated targets. These aspects are seldom investigated in traditional pharmacokinetic research, but can influence the medicine’s therapeutic outcome. Understanding how the exposure levels of active herbal compounds can be effectively modulated is important for ensuring effectiveness of an herbal medicine, by optimally matching the compounds’ pharmacokinetic concentrations (after dosing the medicine) to their respective therapeutic concentrations, or for avoiding occurrence of adverse effect of the medicine, by containing the pharmacokinetic concentrations not to exceed the respective toxic concentrations. Meanwhile, understanding whether the exposure levels of the major active herbal compounds could be significantly modulated is vital for evaluating potential for the medicine to be a victim in a DDI. Our pioneering investigations have involved modulating levels of systemic exposure to several herbal compounds [36, 37, 147]. In traditional pharmacokinetic investigations, drugs are evaluated for systemic exposure and associated disposition, but little is known about their further access to the therapeutic/toxic targets. There are biological barriers for drug molecules moving from the systemic circulation to the locus of action, so it is important to understanding the physiological structures of the target tissues at cellular level. Revealing how pseudoaldosterogenic glycyrrhetic acid and 24-hydroxyglycyrrhetic acid access the renal 11β-HSD2 allows us to identify the ‘safety belt’ for extensive use of Gancao and Gancao-containing medicines in Chinese traditional medicine and people who are susceptible to Gancao-induced pseudoaldosteronism (such as patients with hypoalbuminemia) [47].
So far, drug-combination pharmacokinetic research on Chinese herbal medicines has focused mainly on identifying risks of unintentional DDI associated with herbal medicines used as or in combination therapies. Safe and effective combination therapies are ensured by avoiding the identified risks. In practice of Chinese traditional medicine, many toxic herbs are used for therapeutic purposes, and FangjiPeiwu is used to minimize their toxicities. This deliberate combination for minimizing herb’s toxicity (‘JianduPeiwu’ in Chinese) is another way of ensuring safe combination therapies. Based on the QiqingHehe principle, JianduPeiwu is hypothesized to involve three mechanisms of two types; they are toxicity antagonism, associated with ‘Xiangwei’/’Xiangsha’, that utilizes the combination’s other herb(s) to minimize the toxicity of the toxic herb by counteracting the toxic effect or by reducing the level of exposure to the toxic compounds via pharmacokinetic DDI and efficacy synergism, associated with ‘Xiangxu’ and’Xiangshi’, that decreases the dosage of the toxic herb but maintains the same efficacy while minimizing the toxicity. Last year, the National Natural Science Foundation of China approved support for a major project in JianduPeiwu for therapeutic use of toxic Chinese herbs. The funded project (82192910) involves both multi-compound and drug-combination pharmacokinetic research (which works closely with other disciplines) and selects the commonly used toxic Chinese medicinal herbs Euodia rutaecarpa fruit (Wuzhuyu) and Psoralea corylifolia fruit (Buguzhi) and their formulated herb combinations (i.e., Wuzhuyu decoction, Zuojin pill, Eshen pill, and Sishen pill) for investigation. The multi-compound pharmacokinetic approach is used as the forerunner for identification of toxic compounds of the toxic herbs, as well as interacting and/or therapeutically active compounds of the combinations’ other component herbs. The identified compounds are investigated for the disposition factors governing their levels of body exposure, the pharmacokinetic differences among them, and the simultaneous accessibility to their respective targets. The drug-combination pharmacokinetic approach is used to evaluate PKC degrees of combinations for possible toxicity antagonism that counteracts the toxic effect and for possible efficacy synergism that reduces the dosage of the toxic herb; the approach is also used to evaluate the potential for and toxicological outcome of pharmacokinetic DDIs that result in possible toxicity antagonism. The pharmacokinetic research is to support elucidating potential mechanisms of JianduPeiwu and efficacy–toxicity relationship of the herbs in combinations and serves as a translational discipline. The whole project is multidisciplinary and aims to develop rational strategy for safe and therapeutically effective use of toxic Chinese herbs in clinics.
Over the past decade, great advances have been achieved in the theory, methodology, techniques, and requirements of, together with their applications in, pharmacokinetic research on Chinese herbal medicines, which has become an emerging field in pharmacokinetics. This is a great window of opportunity for the modernization of Chinese traditional medicine to capitalize on the pharmacokinetic approaches, with the valuable ultimate goal of ‘more effective and safe herbal medicines available to patients’.
References
Outline of the main points of prevention and treatment of epidemic diseases with traditional Chinese medicine. Beijing J Tradit Chin Med (Beijing Zhongyiyao). 2014;33:910–2.
Chinese National Health Commission and Chinese State Administration of Traditional Chinese Medicine, Diagnosis and Treatment of Adults with Coronavirus Disease 2019 (COVID-19) (the ninth version), March 15th, 2022 http://www.nhc.gov.cn/yzygj/s7653p/202203/b74ade1ba4494583805a3d2e40093d88/files/ef09aa4070244620b010951b088b8a27.pdf. (accessed on 27th March, 2022)
Zhang BL. Traditional Chinese medicine in China’s combating of Covid-19, brimming with cultural confidence. Red Flag Manuscr (Hongqi Wengao). 2021;6:37–40.
Ni LQ, Chen LL, Huang X, Han CP, Xu JR, Zhang H, et al. Combating COVID-19 with integrated traditional Chinese and Western medicine in China. Acta Pharm Sin B 2020;10:1149–62.
National Medical Products Administration, The notification regarding the implementation of Good Manufacturing Practice of Medical Products (version 2010), https://www.nmpa.gov.cn/xxgk/fgwj/gzwj/gzwjyp/20110225152101646.html. (Accessed 7 June 2022).
Zhang BL, Chen CH, editors-in-chief. Modernization of Chinese medicine for twenty years (1996–2015). Shanghai: Shanghai Science & Technology Press; 2016.
National People’s Congress Standing Committee. Drug Administration Law of the People’s Republic of China. Beijing: Law Press China; 2019.
Wang C, Cao B, Liu QQ, Zou ZQ, Liang ZA, Gu L, et al. Oseltamivir compared with the Chinese traditional therapy Maxingshigan–Yinqiaosan in the treatment of H1N1 influenza. Ann Intern Med. 2011;155:217–25.
Li XL, Zhang J, Huang J, Ma AQ, Yang JF, Li WM, et al. A multicenter, randomized, double-blind, parallel-group, placebo-controlled study of the effects of Qili Qiangxin capsules in patients with chronic heart failure. J Am Coll Cardiol. 2013;62:1065–72.
Shang HC, Zhang JH, Yao C, Liu BY, Gao XM, Ren M, et al. Qi-Shen-Yi-Qi dripping pills for the secondary prevention of myocardial infarction: a randomised clinical trial. Evid Based Complement Altern Med. 2013;2013:738391.
Zhang L, Li P, Xing CY, Zhao JY, He YN, Wang JQ, et al. Efficacy and safety of Abelmoschus manihot for primary glomerular disease: a prospective, multicenter randomized controlled clinical trial. Am J Kidney Dis. 2014;64:57–65.
Song YL, Yao C, Yao YM, Han H, Zhao XD, Yu KJ, et al. XueBiJing injection versus placebo for critically ill patients with severe community-acquired pneumonia: a randomized controlled trial. Crit Care Med. 2019;47:e735–43.
Huang H, Ji LX, Song SY, Wang J, Wei N, Jiang M, et al. Identification of the major constituents in XueBiJing injection by HPLC-ESI-MS. Phytochem Anal. 2011;22:330–8.
Sun Z, Zuo LH, Sun TW, Tang JF, Ding DL, Zhou L, et al. Chemical profiling and quantification of XueBiJing injection, a systematic quality control strategy using UHPLC-Q exactive hybrid quadrupole-orbitrap high-resolution mass spectrometry. Sci Rep. 2017;7:16921.
Yu X, Niu W, Wang YY, Olaleye OE, Wang JN, Duan MY, et al. Novel assays for quality evaluation of XueBiJing: quality variability of a Chinese herbal injection for sepsis management. J Pharm Anal. 2022. https://doi.org/10.1016/j.jpha.2022.01.001.
Yin Q, Li CS. Treatment effects of XueBiJing injection in severe septic patients with disseminated intravascular coagulation. Evid Based Complement Altern Med. 2014;2014:949254.
Wang Q, Wu X, Tong XW, Zhang ZL, Xu B, Zhou WG. XueBiJing ameliorates sepsis-induced lung injury by downregulating HMGB1 and RAGE expressions in mice. Evid Based Complement Altern Med. 2015;2015:860259.
Wang L, Liu ZY, Dong Z, Pan JY, Ma XC. Effects of XueBiJing injection on microcirculation in septic shock. J Surg Res. 2016;202:147–54.
Dong TH, Zhang GP, Dong K, Liu S, Yao YM. Research progress on mechanism of action of XueBiJing injection in the treatment of sepsis. Chin J Tradit Chin Med West Med Crit Care. 2016;23:554–7.
Chen X, Feng YX, Shen XY, Pan GX, Fan GW, Gao XM, et al. Anti-sepsis protection of XueBiJing injection is mediated by differential regulation of pro- and anti-inflammatory Th17 and T regulatory cells in a murine model of polymicrobial sepsis. J Ethnopharmacol. 2018;211:358–65.
Cheng C, Lin JZ, Li L, Yang JL, Jia WW, Huang YH, et al. Pharmacokinetics and disposition of monoterpene glycosides derived from Paeonia lactiflora roots (Chishao) after intravenous dosing of antiseptic XueBiJing injection in human subjects and rats. Acta Pharm Sin. 2016;37:530–44.
Li XX, Cheng C, Wang FQ, Huang YH, Jia WW, Olaleye OE, et al. Pharmacokinetics of catechols in human subjects intravenously receiving XueBiJing injection, an emerging antiseptic herbal medicine. Drug Metab Pharmacokinet. 2016;31:95–8.
Zhang NT, Cheng C, Olaleye OE, Sun Y, Li L, Huang YH, et al. Pharmacokinetics-based identification of potential therapeutic phthalides from XueBiJing, a Chinese herbal injection used in sepsis management. Drug Metab Dispos. 2018;46:823–34.
Li J, Olaleye OE, Yu X, Jia WW, Yang JL, Lu C, et al. High degree of pharmacokinetic compatibility exists between the five-herb medicine XueBiJing and antibiotics comedicated in sepsis care. Acta Pharm Sin B 2019;9:1035–49.
Zheng R, Wang H, Liu Z, Wang XH, Li J, Lei X, et al. A real-world study on adverse drug reactions to XueBiJing injection: hospital intensive monitoring based on 93 hospitals (31,913 cases). Ann Transl Med 2019;7:117.
Lu T, Yang JL, Gao XM, Chen P, Du FF, Sun Y, et al. Plasma and urinary tanshinol from Salvia miltiorrhiza (Danshen), can be used as pharmacokinetic markers for cardiotonic pills, a cardiovascular herbal medicine. Drug Metab Dispos. 2008;36:1578–86.
Liu HF, Yang JL, Du FF, Gao XM, Ma XT, Huang YH, et al. Absorption and disposition of ginsenosides after oral administration of Panax notoginseng extract to rats. Drug Metab Dispos. 2009;37:2290–8.
Li C. Multi-compound pharmacokinetic research on Chinese herbal medicines: approach and methodology. China J Chin Mater Med. 2017;42:607–17.
Li C, Yang JL, Cheng C, Jia WW, Olaleye OE. Pharmacokinetic research on Chinese herbal medicines. Bull Jpn China Med Assoc. 2018;33:9–14.
Li C, Cheng C, Jia WW, Yang JL, Yu X, Olaleye OE. Multi-compound pharmacokinetic research on Chinese herbal medicines: identifying the medicines’ potentially therapeutic compounds and characterizing their disposition and pharmacokinetics. Acta Pharm Sin. 2021;56:2426–46.
Fugh-Berman A. Herb-drug interactions. Lancet. 2000;355:134–8.
Hermann R, Richter O. Clinical evidence of herbal drugs as perpetrators of pharmacokinetic drug interactions. Planta Med. 2012;78:1458–77.
Stieger B, Mahdi ZM, Jager W. Intestinal and hepatocellular transporters: therapeutic effects and drug interactions of herbal supplements. Annu Rev Pharm Toxicol. 2017;57:399–416.
Zhang MM, Liu XM, Li J, He L, Tripathy D. Chinese medicinal herbs to treat the side-effects of chemotherapy in breast cancer patients. Cochrane Database Syst Rev. 2007;18:CD004921.
Lam W, Bussom S, Guan FL, Jiang ZL, Zhang W, Gullen EA, Liu SH, Cheng YC. The four-herb Chinese medicine PHY906 reduces chemotherapy-induced gastrointestinal toxicity. Sci Transl Med. 2010;2:45ra59.
Jiang RR, Dong JJ, Li XX, Du FF, Jia WW, Xu F, et al. Molecular mechanisms governing different pharmacokinetics of ginsenosides and potential for ginsenoside-perpetrated herb-drug interactions on OATP1B3. Br J Pharmacol. 2015;172:1059–73.
Dong JJ, Olaleye OE, Jiang RR, Li J, Lu C, Du FF, et al. Glycyrrhizin has a high likelihood to be a victim of drug-drug interactions mediated by hepatic OATP1B1/1B3. Br J Pharmacol. 2018;175:3486–503.
Olaleye OE, Niu W, Du FF, Wang FQ, Xu F, Pintusophon S, et al. Inhibition of hepatic OATP1Bs by circulating saponins from intravenous ShenMai: potential joint precipitants of drug interactions. Acta Pharmacol Sin. 2019;40:833–49.
Pintusophon S, Niu W, Duan XN, Olaleye OE, Huang YH, Wang FQ, et al. Intravenous formulation of Panax notoginseng root extract: human pharmacokinetics of ginsenosides and potential for perpetrating drug interactions. Acta Pharmacol Sin. 2019;40:1351–63.
Li L, Zhao YS, Du FF, Yang JL, Xu F, Ren YH, et al. Intestinal absorption and presystemic elimination of various chemical constituents present in GBE50 extract, a standardized extract of Ginkgo biloba leaves. Curr Drug Metab. 2012;13:494–509.
Chen F, Li L, Xu F, Sun Y, Du FF, Ma XT, et al. Systemic and cerebral exposure to and pharmacokinetics of flavonols and terpene lactones after dosing standardized Ginkgo biloba leaf extracts to rats via different administration routes. Br J Pharmacol. 2013;170:440–57.
Hu ZY, Yang JL, Cheng C, Huang YH, Du FF, Wang FQ, et al. Combinatorial metabolism notably affects human systemic exposure to ginsenosides from orally administered extract of Panax notoginseng roots (Sanqi). Drug Metab Dispos. 2013;41:1457–69.
Li MJ, Wang FQ, Huang YH, Du FF, Zhong CC, Olaleye OE, et al. Systemic exposure to and disposition of catechols, derived from Salvia miltiorrhiza roots (Danshen), after intravenous dosing DanHong injection in human subjects, rats, and dogs. Drug Metab Dispos. 2015;43:679–90.
Cheng C, Du FF, Yu K, Xu F, Wang FQ, Li L, et al. Pharmacokinetics and disposition of circulating iridoids and organic acids after intravenous administration of ReDuNing injection in rats. Drug Metab Dispos. 2016;44:1853–8.
Liu XW, Yang JL, Jia WW, Wen Q, Niu W, Duan XN, et al. Human pharmacokinetics of ginkgo terpene lactones and impact of carboxylation in blood on their platelet-activating factor antagonistic activity. Acta Pharmacol Sin. 2018;39:1935–46.
Zhang HY, Niu W, Olaleye OE, Du FF, Wang FQ, Huang YH, et al. Comparison of intramuscular and intravenous pharmacokinetics of ginsenosides in humans after dosing XueShuanTong, a lyophilized extract of Panax notoginseng roots. J Ethnopharmacol. 2020;253:112658.
Lan XF, Olajide OE, Du FF, Yang JL, Shi YH, Yang W, et al. Pharmacokinetics-based identification of pseudoaldosterogenic compounds originating from Glycyrrhiza uralensis roots (Gancao) after dosing LianhuaQingwen capsule. Acta Pharmacol Sin. 2021;42:2155–72.
Koltermann A, Hartkorn A, Koch E, Furst R, Vollmar AM, Zahler S. Ginkgo biloba extract EGb761 increases endothelial nitric oxide production in vitro and in vivo. Cell Mol Life Sci. 2007;64:1715–22.
Wu YZ, Li SQ, Cui W, Zu XG, Wang FF, Du J. Ginkgo biloba extract improves coronary blood flow in patients with coronary artery disease: role of endothelial-dependent vasodilation. Planta Med. 2007;73:624–8.
Mashayekh A, Pham DL, Yousem DM, Dizon M, Barker PB, Lin DDM. Effects of Ginkgo biloba on cerebral blood flow assessed by quantitative MR perfusion imaging: a pilot study. Neuroradiology 2011;53:185–91.
Ou HC, Lee WJ, Lee IT, Chiu TH, Tsai KL, Lin CY, et al. Ginkgo biloba extract attenuates oxLDL-induced oxidative functional damages in endothelial cells. J Appl Physiol. 2009;106:1674–85.
Chen JW, Chen YH, Lin FY, Chen YL, Lin SJ. Ginkgo biloba extract inhibits tumor necrosis factor-induced reactive oxygen species generation, transcription factor activation, and cell adhesion molecule expression in human aortic endothelial cells. Arterioscler Thromb Vasc Biol. 2003;23:1559–66.
Chen JS, Huang PH, Wang CH, Lin FY, Tsai HY, Wu TC, et al. Nrf-2 mediated heme oxygenase-1 expression, an antioxidant-independent mechanism, contributes to anti-atherogenesis and vascular protective effects of Ginkgo biloba extract. Atherosclerosis. 2011;214:301–9.
Tsai JY, Su KH, Shyue SK, Kou YR, Yu YB, Hsiao SH, et al. EGb761 ameliorates the formation of foam cells by regulating the expression of SR-A and ABCA1: role of haem oxygenase-1. Cardiovasc Res. 2010;88:415–23.
Huang SY, Jeng C, Kao SC, Yu JJH, Liu DZ. Improved haemorrheological properties by Ginkgo biloba extract (Egb761) in type 2 diabetes mellitus complicated with retinopathy. Clin Nutr. 2004;23:615–21.
Luo Y, Smith JV, Paramasivam V, Burdick A, Curry KJ, Buford JP, et al. Inhibition of amyoid-β aggregation and caspase-3 activation by the Ginkgo biloba extract EGb761. Proc Natl Acad Sci USA. 2002;99:12197–202.
Longpré F, Garneau P, Christen Y, Ramassamy C. Protection by Egb761 against β-amyloid-induced neurotoxicity: involvement of NF-κB, SIRT1, and MAPKs pathways and inhibiton of amyloid fibril formation. Free Radic Biol Med. 2006;41:1781–94.
Tchantchou F, Xu Y, Wu YJ, Christen Y, Luo Y. EGb761 enhances adult hippocampal neurogenesis and phosphorylation of CREB in transgenic mouse model of Alzheimer’s disease. FASEB J. 2007;21:2400–8.
Saleem S, Zhuang H, Biswal S, Christen Y, Doré S. Ginkgo biloba extract neuroprotective action is dependent on heme oxygenase 1 in ischemic reperfusion brain injury. Stroke. 2008;39:3389–96.
Strømgaard K, Nakanishi K. Chemistry and biology of terpene trilactones from Ginkgo biloba. Angew Chem Int Ed. 2004;43:1640–58.
Blumenthal M. The ABC Clinical Guide to Herbs. New York: Thieme; 2003. p. 185–200.
van Beek TA, Montoro P. Chemical analysis and quality control of Ginkgo biloba leaves, extracts, and phytopharmaceuticals. J Chromatogr A. 2009;1216:2002–32.
Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375:2369–79.
Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19:55–71.
Jia W, Li HK, Zhao LP, Nicholson JK. Gut microbiota: a potential new territory for drug targeting. Nat Rev Drug Discov. 2008;7:123–9.
He MQ, Shi BY. Gut microbiota as a potential target of metabolic syndrome: the role of probiotics and prebiotics. Cell Biosci. 2017;7:54.
Roberts AB, Gu XD, Buffa JA, Hurd AG, Wang ZN, Zhu WF, et al. Development of a gut microbe-targeted nonlethal therapeutic to inhibit thrombosis potential. Nat Med. 2018;24:1407–17.
Zeng X, Deng YH, Feng Y, Liu YM, Yang L, Huang Y, et al. Pharmacokinetics and safety of ginsenoside Rd following a single or multiple intravenous dose in healthy Chinese volunteers. J Clin Pharmacol. 2010;50:285–92.
Lu JL, Zeng XS, Zhou X, Yang JL, Ren LL, Long XY, et al. Molecular basis underlying hepatobiliary and renal excretion of phenolic acids of Salvia miltiorrhiza roots (Danshen). Front Pharmacol. 2022;13:911982.
Omar HR, Komarova I, El-Ghonemi M, Fathy A, Rashad R, Abdelmalak HD, et al. Licorice abuse: time to send a warning message. Ther Adv Endocrinol Metab. 2012;3:125–38.
Cinatl J, Morgenstern B, Bauer G, Chandra P, Rabenau H, Doerr HW. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet. 2003;361:2045–6.
Omar HR, Komarova I, El-Ghonemi M, Fathy A, Rashad R, Abdelmalak HD, et al. Licorice abuse: time to send a warning message. Ther Adv Endocrinol Metab. 2012;3:125–38.
Kato H, Kanaoka M, Yano S, Kobayashi M. 3-Monoglucuronyl-glycyrrhetinic acid is a major metabolite that causes licorice-induced pseudoaldosteronism. J Clin Endocrinol Metab. 1995;80:1929–33.
Ohtake N, Kido A, Kubota K, Tsuchiya N, Morita T, Kase Y, et al. A possible involvement of 3-monoglucuronyl-glycyrrhetinic acid, a metabolite of glycyrrhizin (GL), in GL-induced pseudoaldosteronism. Life Sci. 2007;80:1545–52.
Makino T, Ohtake N, Watanabe A, Tsuchiya N, Imamura S, Iizuka S, et al. Down-regulation of a hepatic transporter multidrug resistance-associated protein 2 is involved in alteration of pharmacokinetics of glycyrrhizin and its metabolites in a rat model of chronic liver injury. Drug Metab Dispos. 2008;36:1438–43.
Makino T, Okajima K, Uebayashi R, Ohtake N, Inoue K, Mizukami H. 3-Monoglucuronyl-glycyrrhretinic acid is a substrate of organic anion transporters expressed in tubular epithelial cells and plays important roles in licorice-induced pseudoaldosteronism by inhibiting 11β-hydroxysteroid dehydrogenase 2. J Pharmacol Exp Ther. 2012;342:297–304.
Makino T. 3-Monoglucuronyl glycyrrhretinic acid is a possible marker compound related to licorice-induced pseudoaldosteronism. Biol Pharm Bull. 2014;37:898–902.
Ishiuchi K, Morinaga O, Ohkita T, Tian CT, Hirasawa A, Mitamur M, et al. 18β-Glycyrrhetyl-3-O-sulfate would be a causative agent of licorice-induced pseudoaldosteronism. Sci Rep. 2019;9:1587.
Takahashi K, Yoshino T, Maki Y, Ishiuchi K, Namiki T, Ogawa-Ochiai K, et al. Identification of glycyrrhizin metabolites in humans and of a potential biomarker of liquorice-induced pseudoaldosteronism: a multi-centre cross-sectional study. Arch Toxicol. 2019;93:3111–9.
Morinaga O, Ishiuchi K, Ohkita T, Tian C-T, Hirasawa A, Mitamur M, et al. Isolation of a novel glycyrrhizin metabolite as a causal candidate compound for pseudoaldosteronism. Sci Rep. 2018;8:15568.
Chapman K, Holmes M, Seckl J. 11β-hydroxysteroid dehydrogenases: intracellular gate-keepers of tissue glucocorticoid action. Physiol Rev. 2013;93:1139–206.
Hunter RW, Bailey MA. Glucocorticoids and 11β-hydroxysteroid dehydrogenases: mechanisms for hypertension. Curr Opin Pharmacol. 2015;21:105–14.
Jia Beditor-in-chief. FangjiXue (Chinese Medical Formulae: Therapeutic Effects and Use). Beijing, China Press of Traditional Chinese Medicine; 2016. Chinesey
Morphy R, Kay C, Rankovic Z. From magic bullets to designed multiple ligands. Drug Discov Today. 2004;9:641–51.
Hopkins AL. Network pharmacology: the next paradigm in drug discovery. Nat Chem Biol. 2008;4:682–90.
Mestres J, Gregori-Puigjanć E. Conciliating binding efficiency and polypharmacology. Trends Pharmacol Sci. 2009;30:470–4.
Peters J-U. Polypharmacology—foe or friend? J Med Chem. 2013;56:8955–71.
Anighoro A, Bajorath J, Rastelli G. Polypharmacology: challenges and opportunities in drug discovery. J Med Chem. 2014;57:7874–87.
Korcsmáros T, Szalay MS, Böde C, Kovács IA, Csermely P. How to design multi-target drugs. Expert Opin Drug Discov. 2007;2:799–808.
Costantino L, Barlocco D. Designed multiple ligands: basic research vs clinical outcomes. Curr Med Chem. 2012;19:3353–87.
Proschak E, Stark H, Merk D. Polypharmacology by design: a medicinal chemist’s perspective on multitargeting compounds. J Med Chem. 2019;62:420–44.
Lehár J, Krueger AS, Avery W, Heilbut AM, Johansen LM, Price ER, et al. Synergistic drug combinations tend to improve therapeutically relevant selectivity. Nat Biotechnol. 2009;27:659–66.
Jia J, Zhu F, Ma XH, Cao ZW, Li YX, Chen YZ. Mechanisms of drug combinations: interaction and network perspective. Nat Rev Drug Discov. 2009;8:111–28.
Sun W, Sanderson PE, Zheng W. Drug combination therapy increases successful drug repositioning. Drug Discov Today. 2016;21:1189–95.
Shyr ZA, Cheng YS, Lo DC, Zheng W. Drug combination therapy for emerging viral diseases. Drug Discov Today. 2021;26:2367–76.
Gradman AH, Basile JN, Carter BL, Bakris GL. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4:90–8.
Al-Lazikani B, Banerji U, Workman P. Combinatorial drug therapy for cancer in the post-genomic era. Nat Biotechnol. 2012;30:679–92.
Zhang MM, Liu XM, Li J, He L, Tripathy D. Chinese medicinal herbs to treat the side-effects of chemotherapy in breast cancer patients. Cochrane Database Syst Rev. 2007;18:CD004921.
Lam W, Bussom S, Guan FL, Jiang ZL, Zhang W, Gullen EA, et al. The four-herb Chinese medicine PHY906 reduces chemotherapy-induced gastrointestinal toxicity. Sci Transl Med. 2010;2:45ra59.
Brantley SJ, Argikar AA, Lin YS, Nagar S, Paine MF. Herb-drug interactions: challenges and opportunities for improved predictions. Drug Metab Dispos. 2014;42:301–17.
Bailey DG, Spence JD, Munoz C, Arnold JMO. Interaction of citrus juices with felodipine and nifedipine. Lancet. 1991;37:268–9.
Bailey DG, Arnold JMO, Bend JR, Tran LT, Spence JD. Grapefruit juice-felodipine interaction: reproducibility and characterization with the extended release drug formulation. Br J Clin Pharmacol. 1995;40:135–40.
Pirmohanmed M. Drug-grapefruit juice interactions: two mechanisms are clear but individual responses vary. BMJ. 2013;346:f1.
Ruschitzka F, Meier PJ, Turina M, Luscher TF, Noll G. Acute heart transplant rejection due to Saint John’s wort. Lancet. 2000;355:548–9.
Breidenbach T, Kliem V, Burg M, Radermacher J, Hoffmann MW, Klempnauer J. Profound drop of cyclosporine a whole blood trough levels caused by St. John’s wort (Hypericum perforatum). Transplantation. 2000;69:2229–30.
Barone GW, Gurley BJ, Ketel BL, Lightfoot ML, Abul-Ezz SR. Drug interaction between St. John’s wort and cyclosporine. Ann Pharmacother. 2000;34:1013–6.
Sparreboom A, Cox MC, Acharya MR, Figg WD. Herbal remedies in the United States: potential adverse interactions with anticancer agents. J Clin Oncol. 2004;22:2489–503.
Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol. 2010;55:515–25.
Yu K, Chen F, Li C. Absorption and disposition of saponins: what do we know and what do we need to know? Curr Drug Metab. 2012;13:577–98.
Ramanathan MR, Penzak SR. Pharmacokinetic drug interactions with Panax ginseng. Eur J Drug Metab Pharmacokinet. 2017;42:545–57.
Awortwe C, Makiwane M, Reuter H, Muller C, Louw J, Rosenkranz B. Critical evaluation of causality assessment of herb-drug interactions in patients. Br J Clin Pharmacol. 2018;84:679–93.
Malati CY, Robertson SM, Hunt JD, Chairez C, Alfaro RM, Kovacs JA, et al. Influence of Panax ginseng on cytochrome P450 (CYP)3A and P-glycoprotein (P-gp) activity in healthy participants. J Clin Pharmacol. 2012;52:932–9.
Gurley BJ, Gardner SF, Hubbard MA, Williams DK, Gentry WB, Cui Y-Y, et al. Clinical assessment of effects of botanical supplementation on cytochrome P450 phenotypes in the elderly. Drug Aging. 2005;22:525–39.
Ismair MG, Stieger B, Cattori V, Hagenbuch B, Fried M, Meier PJ, et al. Hepatic uptake of cholecystokinin octapeptide by organic anion-transporting polypeptides OATP4 and OATP8 of rat and human liver. Gastroenterology. 2001;121:1185–90.
Ishiguro N, Maeda K, Kishimoto W, Saito A, Harada A, Ebner T, et al. Predominant contribution of OATP1B3 to the hepatic uptake of telmisartan, an angiotensin II receptor antagonist, in humans. Drug Metab Dispos. 2006;34:1109–15.
Letschert K, Faulstich H, Keller D, Keppler D. Molecular characterization and inhibition of amanitin uptake into human hepatocytes. Toxicol Sci. 2006;91:140–9.
Zhang AJ, Wang CY, Liu Q, Meng Q, Peng JY, Sun HJ, et al. Involvement of organic anion-transporting polypeptides in the hepatic uptake of dioscin in rats and humans. Drug Metab Dispos. 2013;41:994–1003.
Komoroski BJ, Zhang S-M, Cai H-B, Hutzler M, Frye R, Tracy TS, et al. Induction and inhibition of cytochromes P450 by the St. John’s wort constituent hyperforin in human hepatocyte cultures. Drug Metab Dispos. 2004;32:512–8.
Asl MN, Hosseinzadeh H. Review of pharmacological effects of Glycyrrhiza sp. and its bioactive compounds. Phytother Res. 2008;22:709–24.
Li JY, Cao HY, Liu P, Cheng GH, Sun MY. Glycyrrhizic acid in the treatment of liver diseases: literature review. Biomed Res Int. 2014;2014:872139.
Arase Y, Ikeda K, Murashima N, Chayama K, Tsubota A, Koida I, et al. The long term efficacy of glycyrrhizin in chronic hepatitis C patients. Cancer. 1997;79:1494–500.
Expert Committee for Prevention and Management of Liver Inflammation, Chinese Society of Infectious Diseases. Consensus statement by the expert committee for prevention and management of liver inflammation in China. Chin J Hepatol. 2014;22:94–103.
Expert Committee on Clinical Application of Glycyrrhizin Preparation in the Treatment of Liver Diseases. Expert consensus on clinical application of glycyrrhizin preparation in the treatment of liver diseases. J Clin Hepatol. 2016;32:844–52.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). J Am Med Assoc. 2016;315:801–10.
Cao Y, Chai YF, Deng Y, Fang BJ, Liu MH, Lu ZQ, et al. Chinese guidelines for emergency management of sepsis and septic shock 2018. J Clin Emerg. 2018;19:567–88.
Zhao GZ, Chen RB, Li B, Guo YH, Xie YM, Liao X, et al. Clinical practice guideline on traditional Chinese medicine therapy alone or combined with antibiotics for sepsis. Ann Transl Med. 2019;7:122.
Cao Y, Chai YF, Chen FY, Chen XH, Chen YG, Deng Y, et al. Chinese emergency medicine expert consensus on diagnosis and treatment of sepsis complicated with disseminated intravascular coagulation. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017;29:577–80.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Fink MP, Warren HS. Strategies to improve drug development for sepsis. Nat Rev Drug Discov. 2014;13:741–58.
Cohen J, Vincent JL, Adhikari NK, Machado FR, Angus DC, Calandra T, et al. Sepsis: a roadmap for future research. Lancet Infect Dis. 2015;15:581–614.
Steinhagen F, Schmidt SV, Schewe JC, Peukert K, Klinman DM, Bode C. Immunotherapy in sepsis—brake or accelerate? Pharmacol Ther. 2020;208:107476.
Li CY, Wang P, Zhang L, Li M, Lei X, Liu S, et al. Efficacy and safety of XueBiJing injection (a Chinese patent) for sepsis: a meta-analysis of randomized controlled trials. J Ethnopharmacol. 2018;224:512–21.
Liu YC, Yao FH, Chai YF, Dong N, Sheng ZY, Yao YM. XueBiJing injection promotes M2 polarization of macrophages and improves survival rate in septic mice. Evid Based Complement Altern Med. 2015;2015:352642.
Li AL, Li J, Bao YH, Yuan DS, Huang ZW. XueBiJing injection alleviates cytokine-induced inflammatory liver injury in CLP-induced septic rats through induction of suppressor of cytokine signaling 1. Exp Ther Med. 2016;12:1531–6.
Li TT, Qian YM, Miao ZL, Zheng PY, Shi T, Jiang XR, et al. XueBiJing injection alleviates Pam3CSK4-induced inflammatory response and protects mice from sepsis caused by methicillin-resistant staphylococcus aureus. Front Pharmacol. 2020;11:104.
Pea F, Furlanut M. Pharmacokinetic aspects of treating infections in the intensive care unit: focus on drug interactions. Clin Pharmacokinet. 2001;40:833–68.
Pereira JM, Paiva JA. Antimicrobial drug interactions in the critically ill patients. Curr Clin Pharmacol. 2013;8:25–38.
Uijtendaal EV, van Harssel LL, Hugenholtz GW, Kuck EM. Zwart-van Rijkom JE, Cremer OL, et al. Analysis of potential drug-drug interactions in medical intensive care unit patients. Pharmacotherapy. 2014;34:213–9.
Danishuddin, Kumar V, Faheem M, Lee KW. A decade of machine learning-based predictive models for human pharmacokinetics: advances and challenges. Drug Discov Today. 2022;27:529–37.
Wright MR. Opportunities and considerations in the application of artificial intelligence to pharmacokinetic prediction. Methods Mol Biol. 2022;2390:461–82.
Clarke G, Sandhu KV, Griffin BT, Dinan TG, Cryan JF, Hyland NP. Gut reactions: breaking down xenobiotic-microbiome interactions. Pharmacol Rev. 2019;71:198–224.
Hitchings R, Kelly L. Predicting and understanding the human microbiome’s impact on pharmacology. Trends Pharmacol Sci. 2019;40:495–505.
Wang YY, Chu ZX, Yang JL, Olaleye OE, He RR, Li MZ, et al. Poteial health benefits of resveratrol: a pharmacokinetics-caused conundrum. Chin J Clin Pharmacol Ther. 2021;26:931–54. Chinese
Hintze KJ, Cox JE, Rompato G, Benninghoff AD, Ward RE, Broadbent J, et al. Broad scope method for creating humanized animal models for animal health and disease research through antibiotic treatment and human fecal transfer. Gut Microbes. 2014;5:18391.
Arrieta M-C, Walter J, Finlay BB. Human microbiota-associated mice: a model with challenges. Cell Host Microbe. 2016;19:575–8.
Staley C, Kaiser T, Beura LK, Hamilton MJ, Weingarden AR, Bobr A, et al. Stable engraftment of human microbiota into mice with a single oral gavage following antibiotic conditioning. Microbiome. 2017;5:87.
Jia WW, Du FF, Liu XW, Jiang RR, Xu F, Yang JL, et al. Renal tubular secretion of tanshinol: molecular mechanisms, impact on its systemic exposure, and propensity for dose-related nephrotoxicity and for renal herb-drug interactions. Drug Metab Dispos. 2015;43:669–78.
Yamamura Y, Kawakami J, Santa T, Kotaki H, Uchino K, Sawada Y, et al. Pharmacokinetic profile of glycyrrhizin in healthy volunteers by a new high-performance liquid chromatographic method. J Pharm Sci. 1992;81:1042–6.
Funding
This work was funded by grants from the National Natural Science Foundation of China (82192912 and 81673582), Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (ZYYCXTD-C-202009), and the Strategic Priority Research Program of the Chinese Academy of Sciences (XDA12050306).
Author information
Authors and Affiliations
Contributions
C.L. wrote the manuscript. W.J., J.Y., C.C., and O.E.O. contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, C., Jia, Ww., Yang, Jl. et al. Multi-compound and drug-combination pharmacokinetic research on Chinese herbal medicines. Acta Pharmacol Sin 43, 3080–3095 (2022). https://doi.org/10.1038/s41401-022-00983-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00983-7
Keywords
This article is cited by
-
Automatic Classification of Antimalarial Herbal Drugs Exposed to Ultraviolet Radiation from Unexposed Ones Using Laser-Induced Autofluorescence with Chemometric Techniques
Journal of Fluorescence (2024)
-
Pharmacologically significant constituents collectively responsible for anti-sepsis action of XueBiJing, a Chinese herb-based intravenous formulation
Acta Pharmacologica Sinica (2024)
-
APS celebrates the 90th anniversary of SIMM
Acta Pharmacologica Sinica (2022)