Abstract
Background
Atypical triplane fractures (ATFs) defined as a triplane fracture that did not involve the weight-bearing articulating surface or as an extra-articular triplane fracture. ATFs are scarcely reported and the incidence may be underestimated. Moreover, there is no consensus on treatment. This study aimed to evaluate ATFs incidence, fracture pattern, and treatment outcome, and propose treatment recommendations.
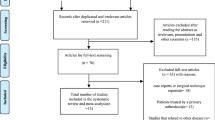
Methods
Twenty-five ATFs of 46 triplane fractures were retrospectively reviewed between 2011 and 2017. ATFs were classified according to the modified ATF classification. Treatment methods were analyzed. Radiologic outcomes were measured based on fracture displacement. Clinical outcomes included the American Orthopedic Foot and Ankle Society score, visual analogue scale, ankle range of motion, and complications at final follow-up period.
Results
A total of 11 type IV, 11 type III, and three type II ATFs were identified. All type II ATFs (intra-articular fracture) were treated with operative treatment. Nine patients were treated with operative treatment and 18 patients were treated with non-operative treatment in type III or IV ATFs (extra-articular fracture). Good radiologic and clinical outcomes were observed in all patients. The residual displacement after initial trial of closed reduction was between 4 and 5 mm in ten cases of type III or IV ATFs; however, no complications were observed, and all cases had good clinical results after non-operative treatment.
Conclusions
ATFs may be under-recognized. Operative treatment and non-operative treatment showed good outcome. Non-operative closed reduction and cast immobilization can be recommended for extra-articular ATF with displacement < 4 mm.
Level of Evidence
Level IV, case series.





Similar content being viewed by others
References
Marmor, L. (1970). An unusual fracture of the tibial epiphysis. Clinical Orthopaedics and Related Research, 73, 132–135.
Landin, L. A., et al. (1986). Late results in 65 physeal ankle fractures. Acta Orthopaedica Scandinavica, 57(6), 530–534.
Peterson, H.A., et al., Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979–1988. J Pediatr Orthop, 1994. 14(4): p. 423–430.
Schnetzler, K. A., & Hoernschemeyer, D. (2007). The pediatric triplane ankle fracture. Journal of American Academy of Orthopaedic Surgeons, 15(12), 738–747.
Ogden, J. A., & McCarthy, S. M. (1983). Radiology of postnatal skeletal development. VIII. Distal tibia and fibula. Skeletal Radiology, 10(4), 209–220.
Ertl, J. P., et al. (1988). Triplane fracture of the distal tibial epiphysis. Long-term follow-up. The Journal of Bone & Joint Surgery. American Volume, 70(7), 967–976.
Spiegel, P. G., et al. (1984). Triplane fractures of the distal tibial epiphysis. Clinical Orthopaedics and Related Research, 188, 74–89.
von Laer, L. (1985). Classification, diagnosis, and treatment of transitional fractures of the distal part of the tibia. Journal of Bone and Joint Surgery. American Volume, 67(5), 687–698.
Yung, C. S., Kuong, E. E., & Chow, W. (2019). A previously unreported type of extra-articular triplane fracture: A revised classification system. Journal of Orthopaedic Surgery (Hong Kong), 27(1), 2309499019828500.
Brown, S. D., et al. (2004). Analysis of 51 tibial triplane fractures using CT with multiplanar reconstruction. American Journal of Roentgenology, 183(5), 1489–1495.
Shin, A. Y., Moran, M. E., & Wenger, D. R. (1997). Intramalleolar triplane fractures of the distal tibial epiphysis. Journal of Pediatric Orthopedics, 17(3), 352–355.
Thawrani, D., et al. (2011). Reliability and necessity of computerized tomography in distal tibial physeal injuries. Journal of Pediatric Orthopedics, 31(7), 745–750.
Kling, T. F., Jr. (1990). Operative treatment of ankle fractures in children. Orthopedic Clinics of North America, 21(2), 381–392.
Mann, D. C., & Rajmaira, S. (1990). Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0–16 years. Journal of Pediatric Orthopedics, 10(6), 713–716.
Jones, S., et al. (2003). Triplane fractures of the distal tibia requiring open reduction and internal fixation. Pre-operative planning using computed tomography. Injury, 34(4), 293–298.
Salter, R. B., & Harris, R. (1963). Injuries involving the epiphyseal plate. The Journal of Bone and Joint Surgery. American Volume, 45, 587–622.
Denton, J. R., & Fischer, S. J. (1981). The medial triplane fracture: Report of an unusual injury. Journal of Trauma, 21(11), 991–995.
van Laarhoven, C. J., & van der Werken, C. (1992). “Quadriplane” fracture of the distal tibia: A triplane fracture with a double metaphyseal fragment. Injury, 23(7), 497–499.
Ryu, S. M., et al. (2018). Is an operation always needed for pediatric triplane fractures? Preliminary results. Journal of Pediatric Orthopaedics B, 27(5), 412–418.
Kim, J. R., et al. (2010). Treatment outcomes of triplane and Tillaux fractures of the ankle in adolescence. Clinics in Orthopedic Surgery, 2(1), 34–38.
Choudhry, I. K., et al. (2014). Functional outcome analysis of triplane and tillaux fractures after closed reduction and percutaneous fixation. Journal of Pediatric Orthopedics, 34(2), 139–143.
Rapariz, J. M., et al. (1996). Distal tibial triplane fractures: Long-term follow-up. Journal of Pediatric Orthopedics, 16(1), 113–118.
Lurie, B., et al. (2020). Functional Outcomes of Tillaux and Triplane Fractures with 2 to 5 Millimeters of Intra-Articular Gap. Journal of Bone and Joint Surgery. American Volume, 102(8), 679–686.
O’Connor, D. K., & Mulligan, M. E. (1998). Extra-articular triplane fracture of the distal tibia: A case report. Pediatric Radiology, 28(5), 332–333.
Kay, R. M., & Matthys, G. A. (2001). Pediatric ankle fractures: Evaluation and treatment. Journal of American Academy of Orthopaedic Surgeons, 9(4), 268–278.
Barmada, A., Gaynor, T., & Mubarak, S. J. (2003). Premature physeal closure following distal tibia physeal fractures: A new radiographic predictor. Journal of Pediatric Orthopedics, 23(6), 733–739.
Schurz, M., et al. (2010). Physeal injuries of the distal tibia: Long-term results in 376 patients. International Orthopaedics, 34(4), 547–552.
Funding
This work was supported by a research grant from of Jeju National University Hospital in 2020 (202000390001).
Author information
Authors and Affiliations
Contributions
Study design: CL and HK. Data acquisition: CL and TK. Data analysis: CL and TK. Drafting of manuscript: CL and HK. Review and editing of manuscript: CL, TK, and HK.
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
This retrospective study was conducted in accordance with the relevant guidelines and regulations outlined in the Declaration of Helsinki, and was approved by the institutional review board (IRB) of our hospital (IRB Approval No.: 2020-01-009).
Informed Consent
The requirement for informed consent was waived by the IRB of our hospital owing to the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, H., Kang, T. & Lim, C. The Incidence and Treatment Outcome of Atypical Triplane Fractures in Adolescents. JOIO 56, 2133–2140 (2022). https://doi.org/10.1007/s43465-022-00679-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00679-4