Abstract
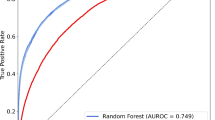
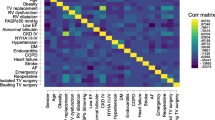
Accurate estimation of surgical risks is important for informing the process of shared decision making and informed consent. Postoperative reintubation (POR) is a severe complication that is associated with postoperative morbidity. Previous studies have divided POR into early POR (within 72 h of surgery) and late POR (within 30 days of surgery). Using data provided by American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP), machine learning classification models (logistic regression, random forest classification, and gradient boosting classification) were utilized to develop scoring systems for the prediction of combined, early, and late POR. The risk factors included in each scoring system were narrowed down from a set of 37 pre and perioperative factors. The scoring systems developed from the logistic regression models demonstrated strong performance in terms of both accuracy and discrimination across the different POR outcomes (Average Brier score, 0.172; Average c-statistic, 0.852). These results were only marginally worse than prediction using the full set of risk variables (Average Brier score, 0.145; Average c-statistic, 0.870). While more work needs to be done to identify clinically relevant differences between the early and late POR outcomes, the scoring systems provided here can be used by surgeons and patients to improve the quality of care overall.


Similar content being viewed by others
References
Hua M, Brady JE, Li G. A scoring system to predict unplanned intubation in patients having undergone major surgical procedures. Anesth Analg. 2012;115(1):88–94. https://doi.org/10.1213/ANE.0b013e318257012b.
Brueckmann B, Villa-Uribe JL, Bateman BT, et al. Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology. 2013;118(6):1276–85. https://doi.org/10.1097/ALN.0b013e318293065c.
Beverly A, Brovman EY, Malapero RJ, Lekowski RW, Urman RD. Unplanned reintubation following cardiac surgery: incidence, timing, risk factors, and outcomes. J Cardiothorac Vasc Anesth. 2016;30(6):1523–9. https://doi.org/10.1053/j.jvca.2016.05.033.
Ramachandran SK, Nafiu OO, Ghaferi A, Tremper KK, Shanks A, Kheterpal S. independent predictors and outcomes of unanticipated early postoperative tracheal intubation after nonemergent. Noncardiac Surg Anesthesiol. 2011;115(1):44–53. https://doi.org/10.1097/ALN.0b013e31821cf6de.
Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250(3):363–76. https://doi.org/10.1097/SLA.0b013e3181b4148f.
Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44(1):251–67. https://doi.org/10.1016/j.yasu.2010.05.003.
Khuri SF, Henderson WG, Daley J, et al. The patient safety in surgery study: background, study design, and patient populations. J Amr Coll Surg. 2007;204(6):1089–102. https://doi.org/10.1016/j.jamcollsurg.2007.03.028.
Hall BL, Richards K, Ingraham A, Ko CY. New approaches to the national surgical quality improvement program: the American College of Surgeons experience. Amr J Surg. 2009;198(5):S56–62. https://doi.org/10.1016/j.amjsurg.2009.07.026.
Shiloach M, Frencher SK, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Amr Coll Surg. 2010;210(1):6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031.
Guo X, Yin Y, Dong C, Yang G, Zhou G (2008) On the class imbalance problem. In: 2008 Fourth international conference on natural computation 4:192–201. https://doi.org/10.1109/ICNC.2008.871
Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–42. https://doi.org/10.1016/j.jamcollsurg.2013.07.385.
Harris DM, Harris SL. State encodings. In: Digital design and computer architecture. 2nd ed. Boston: Elsevier; 2013. p. 129–31.
Mohamad IB, Usman D. Standardization and its effects on K-means clustering algorithm. Res J Appl Sci Eng Technol. 2013;6(17):3299–303. https://doi.org/10.19026/rjaset.6.3638.
Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg. 2013;217(2):336–46. https://doi.org/10.1016/j.jamcollsurg.2013.02.027.
Breiman L. Random forests. Mach Learn. 2001;45(1):5–32. https://doi.org/10.1023/A:1010933404324.
Friedman JH. Greedy function approximation: a gradient boosting machine. Ann Stat. 2001;29(5):1189–232. https://doi.org/10.1214/aos/1013203451.
Brier GW. Verification of forecasts expressed in terms of probability. Mon Weather Rev. 1950;78(1):1–3.
Krzywinski M, Altman N. Nonparametric tests. Nat Methods. 2014;11(5):467–8. https://doi.org/10.1038/nmeth.2937.
Altmann A, Toloşi L, Sander O, Lengauer T. Permutation importance: a corrected feature importance measure. Bioinformatics. 2010;26(10):1340–7. https://doi.org/10.1093/bioinformatics/btq134.
Ojala M, Garriga GC (2009) Permutation tests for studying classifier performance. In: 2009 Ninth IEEE international conference on data mining. IEEE, pp 908–913. https://doi.org/10.1109/ICDM.2009.108
Akobeng AK. Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr. 2007;96(3):338–41. https://doi.org/10.1111/j.1651-2227.2006.00180.x.
Heider S, Schoenfelder J, McRae S, Koperna T, Burner JO. Tactical scheduling of surgeries to level bed utilization in the intensive care unit. IISE Trans Healthc Syst Eng. 2020;10(4):229–42. https://doi.org/10.1080/24725579.2020.1793845.
Funding
MJK: University of Vermont College of Engineering and Mathematical Sciences Summer REU Award; RDU: funding and/or fees from Merck, Covidien/Medtronic, AcelRx and Pfizer.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis was performed by Mathew Koretsky and Dr. Nick Cheney. The first draft of the manuscript was written by Mathew Koretsky and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Given the deidentified nature of the data, the research was deemed Not Human Subjects Research by the Institutional Review Board (Mass General Brigham protocol #2015P002706 and Tufts University protocol described in Supplementary Document 1).
Informed consent
Given the research was deemed Not Human Subjects Research, it is exempted from the informed consent requirement.
Conflict of interest
Other authors report no conflict of interest.
Informed consent
Given the research was deemed Not Human Subjects Research, it is exempted from the consent requirement.
Consent to publish
Given the research was deemed Not Human Subjects Research, it is exempted from the consent requirement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koretsky, M.J., Brovman, E.Y., Urman, R.D. et al. A machine learning approach to predicting early and late postoperative reintubation. J Clin Monit Comput 37, 501–508 (2023). https://doi.org/10.1007/s10877-022-00908-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00908-z